* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Unit 10 - CDN Site
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Cardiac surgery wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Myocardial infarction wikipedia , lookup
Jatene procedure wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
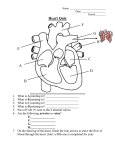
Unit 10 Circulation System 10.1 Blood Vessels A. Arteries and Arterioles Arteries: are large blood vessels that carry blood away from the heart Each time your heart contracts blood enters the arteries Arteries are elastic and can stretch (they are under a lot pressure and need to be able to stretch) Arteries consist of layers o The outer and inner layer is made of connective tissue o The middle layers are made of smooth muscle fibres and elastic connective tissue o It is the elastic connective tissue that allows the arteries to stretch Arteries diameter are regulated by the autonomic nervous system (the part that regulates equilibrium) Nerve impulses cause the smooth muscle of the artery to contract Contraction of the arteries smooth muscle reduces it's diameter = vasoconstriction o vasoconstriction reduces blood flow to the area Relaxation of the smooth muscle causes the artery to increase it's diameter This dilation is referred to a vasodilation o Vasodilation increases blood flow to an area Arterioles: are smaller arteries o They too are elastic o Diameter is regulated by nervous impulses o When the nervous impulse sends a message to contract = vasocontriction (smaller in diameter) There is a blood flow to the tissues o When the nervous impulse sends a message to dilate = vasodialation (larger in diameter) There is a blood flow to the tissues Blood passes from the arteries to the arterioles Heart arteries arterioles Capillaries Atherosclerosis: Cause: a high fat diet can lead to the accumulation of plaque and fat deposits in the artery 1 Effect: can narrow the artery to one-quarter of its original diameter Result: This can make it more difficult for blood to pass through… leading to lead to high blood pressure. Also, blood clots form around the fat deposits. As these accumulate, adequate amounts of blood and oxygen cannot be delivered to the heart muscle, resulting in chest pain. Aneurysm: Cause: birth defects, injury, genetics (weak arteries) Most common sites: aorta, abdominal aorta and arteries in the brain Effect: Weak part of an artery or vein that begins to protrude as blood surges through (it usually is an artery) Result: a bulge in the artery/vein The weakened wall can eventually burst / hemorrhage If this occurs in the brain = hemorrhagic stroke With no blood (nutrients and O2) being supplied brain cells die Precapillary sphincter muscles Control the movement of blood from the arterioles to the capillaries B.Capillaries Composed of a single layer of cells Capillary beds are easily destroyed because capillaries only have a single layer of cells (E.g. high blood pressure) Site of fluid and gas exchange between blood and body cells They are so thin that blood cells can only pass through them in single file The exchange of oxygen and carbon dioxide takes place through the thin capillary wall. The red blood cells inside the capillary release their oxygen (H+ dislodges O2 from oxyhemoglobin) O2 passes through the capillary wall and into the interstitial space Interstitial spaces This is the space that is found between the capillary and the cell It surrounds the cell 2 Bruising occurs when capillaries are damaged and blood flows into the interstitial space C. Veins and Venules Venules Capillaries merge into larger venules Venules are lined with smooth muscles Veins Venules merge into veins which are larger in diameter The diameter of veins increases as they approach the heart Fluid pressure is reduced in veins (makes it harder for blood to flow to the heart) Skeletal Muscle contraction aids blood flow toward the heart o Muscles bulge when they contract o this reduces the diameter of the vein o pressure inside the vein increases o this in pressure causes the valves to push open allowing blood to flow back to the heart Note: These One -way valves prevent blood from flowing backwards and steers blood towards the heart Veins also act as blood reservoirs o When your stressed venous flow to help meet energy demands o Nervous impulses contract the smooth muscle (in the veins) o This blood pressure o Therefore more blood reaches the heart Varicose Veins: Large volumes of blood can damage veins and cause the valves to become damaged Cause: heredity, standing for long periods or compression of veins valves do not close properly causing blood to pool in the veins surface veins become enlarged they begin to bulge = varicose veins Effect: blood pools in areas (legs, anus). 3 10.2 The Heart your heart is located in the thoracic cavity behind the sternum your heart has a mass of about 300 g and is about the size of your fist uses up 15% of the bodies O2 and food supply it is surrounded by a fluid-filled membrane called the pericardium which prevents friction a wall of muscle separates the right and left sides of the heart = septum The heart has 4 chambers 2 atria (L&R) 2 ventricles (L&R) atria act like holding chambers for blood entering the heart o blood from the pulmonary system enters the left atrium o blood from the systemic system enters the right atrium ventricles are strong muscular chambers that pump blood away from the heart cardiac muscle is very strong with a layer of fat around the it that acts as a cushion The artery that supplies the heart muscle with blood is the coronary artery Your Assignment: Heart Diagram – label the structures (see page 320) aorta left pulmonary artery septum left pulmonary vein right atrium right pulmonary artery left atrium right pulmonary vein right ventricle 2 semilunar valves left ventricle 2 atrioventricular (AV) valves superior vena cava inferior vena cava chordae tendonae (draw this in) A. One Way Blood Flow pulmonary circulation = blood vessels that carry blood to and from lungs systemic circulation = blood vessels that carry blood to and from body 4 Superior vena cava = carries deoxygenated blood from your head to your heart Inferior vena cava = carries deoxygenated blood from your body to your heart Blood Flow Veins carry blood to the heart 1. deoxygenated blood reaches the heart through inferior and superior vena cava and empties into the right atrium 2. blood moves through atrioventricular or (AV) valve into right ventricle (***note: these are supported by bands of tendons called chordae tendinae) 3. blood pumped through semilunar valve into the left and right pulmonary arteries (***note: these are the only arteries that carry deoxygenated blood) 4. in lungs, oxygen diffuses into the blood 5. oxygenated blood enters pulmonary veins which take it back to the heart (***note: these are the only veins that carry oxygenated blood) 6. blood enters left atrium then moves through atrioventricular or (AV) valve into the left ventricle 7. oxygenated blood pumped through semilunar valve into the aorta (largest artery) where it travels to body tissues (*** note: these valves prevent the backflow of blood from the artery into a ventricle) 8. tissues use oxygen/nutrients/fluids in blood, then deoxygenated blood moves through vein system into inferior and superior vena cava coronary arteries supply the heart muscle cells with O2 and nutrients chest pain (angina) occurs when too little O2 reaches the heart it could be but not always caused by a blockage if it is a blockage, then the blockage can be bypassed by using veins from other parts of the body …these are grafted into the heart 5 Your Assignment: Draw red (oxygenated) and blue (deoxygenated) arrows on heart diagram to show blood flow into and out of heart Your Assignment: Page 320, 1-4 B .Cardiac Catheterization It is a technique used to detect coronary artery blockage A catheter (small thin hollow tube) is passed into an artery in the groin The catheter is then pushed up through the aorta and into the heat A dye is then injected into the catheter The dye travels through the blood vessels while its image is traced by a fluoroscope An area of restricted blood flow pinpoints the region of blockage Figure 5 Page 323 Blood samples can also be taken to determine how much O2 is in the blood in different chambers of the heart C. Setting the Heart's Tempo Cardiac muscle tissue differs from other muscle tissue in that is has a branching pattern It is also the only muscle tissue that can contract without external nerve stimulation Muscle with this ability is called myogenic muscle The heart's tempo is set by the sinoatrial or (SA) node This is a bundle of specialized nerves and muscle located in the upper right atrium The SA nodes acts as a pacemaker, and sets a rhythm of about 70 beats/min the following sequence of events outlines the nervous control of the heart: the beat (contraction) is generated in the SA node electrical impulses pass on to both atria, causing them to simultaneously contract 6 the impulses then move on to a second node called the atrioventricular node (AV node) (which acts like a conductor passing the nerve impulses) the message to contract is then relayed quickly down special nerves in the septum called the Bundle of His the message is sent into extensions of nerves in the ventricle walls called the Perkinje Fibres both ventricles are now stimulated to contract at the same time receptors in the body monitor the concentration of chemicals in the blood and blood pressure: 1. baroreceptors monitor pressure in the aorta and carotid artery 2. chemoreceptors monitor amount of CO2 in blood these receptors send signals to a specialized area in the brain called the medulla oblongata the medulla oblongata responds by stimulating either increasing or decreasing heart rate Autonomic nerve impulses can affect heart rate 1. parasympathetic nervous system: tells heart to beat at a normal rate 2. sympathetic nervous system: tells heart to increase heart rate Stress when you are stressed sympathetic nerves send impulses to the pacemaker to increase heart rate this increases blood flow to the tissues Heart rate exceeding 100 beats/minute = tachychardia Relaxation During relaxation parasympathetic nerves are stimulated and send messages to the pacemaker to slow the heart down Low heart rate = bradycardia Electrical Conductivity of the Heart an electrocardiogram (ECG) is a machine that can measure the electrical activity of the heart changes in the electrical current reveal normal or abnormal events in the cardiac cycle 7 Pwave = atrial contraction QRS = ventricular contraction T = ventricles relaxed Electrical Current (mV) 0 0.5 1.0 Time (s) Electrocardiogram overheads By comparing electrocardiograph tracings doctors can determine areas of the heart that are having problems Case study Page 324 (Diagnosing Heart Conditions) D. Heart Sounds The "lubb-dubb" sound we hear is caused by the opening and closing of heart valves lubb is the closing of the AV valves (ventricles pumping) dubb is the closing of the semilunar valves (atria pumping) The heart also has a period of relaxation = diastole (both atria and ventricles are relaxed) The period of contraction is called systole The Cycle: 1. atria are relaxed and fill with blood-diastole 2. the atria contract and AV valves open 3. blood flows and fills the ventricles 4. the ventricles contract – systole 5. the pressure causes the AV valves to close (lubb sound heard) 6. blood pushes through the semilunar valves and into the ateries 7. semilunar valves close (dubb sound heard) 8. ventricular relaxation (filling with blood again) – diastole 8 Heart Murmur sometimes valves don’t close properly: a heart murmur results heart murmurs occur when blood leaks past a closed heart valve people with heart murmurs must make up for decrease O2 Two ways this can occur 1. the heart will beat faster….delivering blood faster 2. cardiac muscle stretching more than normal the atrium accepts the normal volume of blood plus some from the ventricle (this stretches the atrium) blood is driven to the ventricle with force which causes it to contract with force…. thus more blood to tissues E. Medication and the Heart Beta blockers are often used to treat irregular heartbeats and high blood pressure How they work Epinephrine, a stress hormone, attaches to receptor on heart cells and blood vessels This increases heart rate and narrows blood vessels (both increase blood pressure) Beta blockers work by binding to the receptor site on the cell so epinephrine can’t bind Result = heart is slowed….individuals may feel dizzy because of low blood pressure Your Assignment: page 327, 1-12 9 10.3 Regulation of Blood Flow A. Cardiac Output cardiac output: is the amount of blood that flows from the heart each minute (normally the same on both sides) cardiac output = heart rate x stroke volume = 70 beats/minute x 70 mL/beat = 4900 mL/minute Activity – measure cardiac output, exercise for 3 minutes then measure cardiac output again…explain the change people with well-developed hearts can pump greater volumes of blood, which is why athletes have a low heart rate. a weaker heart is unable to pump as much, but can compensate by increasing the heart rate to meet energy demands Two factors that affect cardiac output: 1. Heart rate 2. Stroke volume Heart rate: is the number of times the heart beats per minute stroke volume: is the amount of blood pumped with each beat of the heart (70 mL)… the stronger the contraction the greater the stroke volume (althetes) B. Blood Pressure blood pressure is the pressure exerted on the walls of the arteries constant BP is needed to maintain the proper functioning of all other systems measured with a sphygmomanometer A cuff with an air bladder is wrapped around the arm A small pump inflates the air bladder which closes off blood flow through the brachial artery (one of the major arteries of the arm) A stethoscope is placed below the cuff and air is released from the bladder until a low-pitch sound is heard The sound is caused by blood re-entering the artery –Systolic blood pressure (contraction ) The cuff is deflated more until the sound disappears and blood flows freely- diastolic blood pressure (relaxation) 10 diastolic (relaxation) pressure is 35% lower than systolic (contraction) pressure typical BP is 120/70 (systolic/diastolic) measured BP varies depending on where in the body it is measured: 1. highest in left ventricle – pumps blood to whole body 2. high in systemic (body) circulation 3. lower in pulmonary (lung) circulation 4. lowest in right side of heart – only pumps to lungs Blood Pressure depends on two factors: 1. Cardiac output 2. Arteriolar resistance 1. Cardiac output: an increased volume coming from the ventricles creates a greater pressure on the walls or the arteries 2. Arteriolar resistance: the diameter is regulated by smooth muscles …as smooth muscle in the arterioles contract, the diameter decreases…..less blood is allowed to pass Result = More blood is left in the artery….blood pressure increases What Else can Cause a Change in Blood Pressure? o Hormones, nerve stimulation (constriction), o Metabolic wastes (acid, CO2)(dilation) C. Regulation of Blood Pressure It is critical that your body regulates blood pressure Too high…damages the vessels…add stress = vessels can rupture Too low…tissues will not receive enough blood controlled by pressure receptors called baroreceptors in the aorta and carotid (detect when its high) also involved is the medulla oblongata (brain), and nerves called the parasympathetic and sympathetic nerves 1. High Pressure also known as hypertension (silent killer) Caused by heredity, and poor diet (E.g. too much salt) There is an increase in resistance to blood flow 11 baroreceptors in aorta and carotid send a nerve impulse to the medulla oblongata parasympathetic nerve (slow down) function increases and sympathetic nerve (stress nerve)function decreases arterioles dilate blood flow increases heart rate cardiac output pressure decreases 2. Low Pressure baroreceptors in aorta and carotid send a nerve impulse to the medulla oblongata sympathetic nerve function and parasympathetic nerve function arterioles constrict blood flow decreases heart rate cardiac output pressure increases 3. Stress/Exercise sympathetic nerve stimulates the adrenal gland which then secretes adrenalin (epinephrine) adrenalin has 3 functions: 1. releases red blood cells from the spleen to increase O2 delivery 2. vasodilation of arterioles in heart, brain, muscles 3. vasoconstriction of arterioles in kidneys, stomach, intestines ***most active tissues get priority ***Fight-or-flight response D. Regulating body Temperature Thermoregulation is the maintenance of body temperature within a range that enables cells to function The body tries to maintain a constant internal temperature of 37 degrees 12 Hot? Sensors in the brain detect a rise in body temperature The hypothalamus (the control center of the brain) sends a nerve impulse to the sweat glands You begin to perspire Evaporation perspiration cools the skin A nerve impulse is also sent to the blood vessels causing them to dilate….increase blood flow to the skin….heat is lost Cold? Thermoreceptors in the skin send a nerve impulse to the hypothalamus The hypothalamus send a message to organs and tissues to increase body temperature Nerves signal the smooth muscle in the arterioles… to constrict (reduces heat loss) Nerves signal the smooth muscle around hair follicles … hair stands on end (trapping heat) Nerve signal is sent from your hypothalamus to your skeletal muscle… initiating shivering…(generating heat) 10.4 Capillary Fluid Exchange every cell in the body is within 0.1 mm of a capillary capillaries: 1. provide cells with nutrients (glucose, O2 etc) 2. take away cell wastes (CO2 etc) 3. maintain a constant fluid level 4. exchange fluid between blood and extracellular fluid (ECF) two forces regulate the movement of water between blood and ECF Fluid pressure Osmotic pressure Force of blood the capillary is 35mmHg.. ..(lower in the ECF) Water moves from an area of high pressure to low 1. Filtration occurs in the arteriole end of the capillary 13 capillaries are selectively permeable water and small ions move out of the capillary into the ECF movement is the result of pressure gradient – from high to low pressure 2. Absorption occurs in the venule end of the capillary water moves from ECF into the capillary – large proteins in the capillary makes the concentration of H2O greater in the ECF movement is the result of osmotic gradient – from high to low concentration of H2O Capillary Fluid Exchange ECF arteriole end high pressure venule end low [H2O] capillary H2O, ions H2O blood proteins low pressure ECF ECF high [H2O] Your Assignment: Use pg 337 to describe the cause and effect of each of the following: hemorrhage, edema, allergic reactions 14 B. Lymphatic System small amount s of protein leak from capillaries to tissue spaces this is dangerous over time…. because osmotic pressure would decrease and tissues would swell proteins are drained from the ECF and returned to the circulatory system by the lymphatic system a noncircular system of vessels that takes fluids from tissues to the bloodstream lymph vessels are similar to veins…they use one-way valves and muscular contractions to move the fluids (lymph) lymph is fluid similar to blood plasma… it contains proteins that collect in the ECF (it’s mostly water) eventually lymph is returned to venous system via the right and left subclavian veins large lymphatic ducts collect the lymph…the main duct is called the thoracic duct o blocking of lymphatic ducts can cause severe edema Enlargements called lymph nodes are located along the vessels Lymph nodes: manufacture and house immune system cells that, by phagocytosis, filter bacteria and debris from the lymph they also filter damaged cells and debris from the lymph and store lymphocytes C. Lymphoid Organs Red bone marrow is where all types of blood cells are produced o In children: found in most bones o In adults: found in the cranium, sternum, ribs, spinal column and long bones Stem cells (in the marrow) differentiate into different types of white blood cells They enter the circulatory system from a variety of sinuses The spleen The spleen is one of the body's largest lymphoid organs Located in the upper left side Richly supplied with blood sinuses which enable it to hold 150mL of blood (reservoir) 15 Releases red blood cells if there is: Low blood pressure O2 levels drop The Thymus gland It gets smaller with age Located in front of the trachea, above the heart It is where T lymphocytes mature Activity – measuring blood pressure 1. Measure and record the blood pressure of everyone in your group. 2. How does exercise affect your blood pressure and why? 3. How would atherosclerosis affect your blood pressure and why? Your Assignment: Page 339 1-7 Your Assignment: Review Page 346 1-16 16