* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Chapter 6
Survey
Document related concepts
Transcript
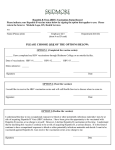
Virology 7105326 Two-Credit Hour Course (Second Semester 2015-2016) Part 10 Hepatitis B & Hepatitis D (Delta) Viruses 1 Hepatitis B Virus (HBV): Hepatitis: it is inflammation of the liver. Viral hepatitis: it is the inflammation of liver due to viral infection. Hepatitis viruses: 1- Hepatotropic viruses: There are the viruses that infect the liver specifically to cause hepatitis. Most of these hepatotropic viruses are RNA viruses that belong to different families. (Examples: Hepatitis A virus (HAV), HCV, HEV and HDV) The only hepatotropic DNA virus that specifically infects the liver is Hepatitis B virus (HBV) 2- Non-hepatotropic viruses: these mainly include Human Cytomegalovirus (CMC) and Epstein Barr Virus(EBV) which can infect various cells and tissues that may include the liver. Pathogenesis of viral hepatitis: Although viral infection of liver cells may have some cytopathic effect on these cells, most of the damage that is seen during viral hepatitis is mediated by cytotoxic T cells, which attack and destroys virally-infected hepatic cells. Hepatitis B virus (HBV): HBV belongs to the family Hepadnaviridae. This family includes several viruses that infect the liver (hepatotropic) of many animals. The only member of this family that infects humans is HBV. General features of Hepadnaviridae: Genome: ds DNA (circular but incomplete) Symmetry/morphology: Icosahedral Enveloped 2 HBV Structure: It has an enveloped icosahedral nucleocapsid It has a large envelope-associated protein that is known as Hepatitis B surface antigens (HBsAg), which can be seen in the blood of infected individuals alone or in association with the envelope of the nucleocapsid. HBV has a partially ds DNA genome that forms a non-covalently closed circle. Note: Dane particles represent the enveloped nucleocapsid in association with its surface antigen. HBV proteins: The capsid protein: which is known as hepatitis B core antigen (HBcAg) The envelope protein: which is known as hepatitis B surface antigen (HBsAg) Multifunctional reverse transcriptase/DNA polymerase enzyme: which is associated with the DNA genome within the capsid A non-structural regulatory protein known as hepatitis E antigen (HBeAg), which is found in the tegument region. 3 HBV Transmission: The presence of HBV in the blood stream in an enormous number ((108 virus /ml)), implies that the virus can be found in almost all body fluids. Accordingly, HBV can be transmitted by: Sexual contact Transplacentally Perinatally Breast feeding Blood transfusion Sticks with contaminated needled Wound and skin cuts (upon contact with blood and other body fluids of a HBV infected patient) . Epidemiology: World-wide, about 300 million people are chronically-infected with HBV (most of these cases are in Asia and Middle-East). Chronic HBV infection may result in serious complications such as liver cirrhosis, and hepatocellular carcinoma. Both complications account for about 1 million deaths each year. . Pathogenesis HBV hepatitis: Role of cytotoxic T cells: Although HBV may have some cytopathic effect on infected liver cells, however, most of pathological alterations that are seen during viral hepatitis are mediated mainly by cytotoxic T cells, which recognize and kill virally-infected hepatic cells. HBV-infected liver cells express on their surfaces MHC-I molecules that are loaded with peptide antigens derived from HBV proteins, mainly from HBcAg and HBeAg. These infected liver cells are recognized and killed by cytotoxic T cells. Role of NK cells: NK can be also involved in hepatic pathological alterations seen during HBV infection Role of anti-HBsAg antibodies (HBsAb): Anti-HBsAg antibodies (HBsAb) appear during late stages of infection and can play an important role in clearing any remaining circulating HBV in the blood stream. 4 However, in some cases and during HBV infection, the formation and deposition of immune complexes (HBsAg/HBsAb) in the liver may cause an additional liver damage (due to complement activation). This can be seen in about 10-20 % of HBV infected people. Note: these immune complexes are also responsible for arthritis that can be associated with HBV infection Course of infection: Incubation period is about 90 days (60–150 days). It is estimated that only one-third of primary HBV-infected individuals exhibit obvious clinical symptoms (acute HBV infection/Jaundice). The other two-third of HBV primary infections is asymptomatic Clinical symptoms of symptomatic acute primary HBV infection: I- Pre-icteric (pre-jaundice) phase: This phase is seen by the end of the incubation period, just few days before the appearance of Jaundice. It is characterized by fever, malaise, anorexia and myalgias. II- Acute icteric phase (Jaundice phase): (Lasts for 1-2 months) The most obvious clinical symptom of acute hepatitis is Jaundice. Jaundice develops as a result of bilirubinemia that occurs due to liver-function inefficiency due to inflammation of the liver inflammation (hepatitis). Jaundice is characterized by: 1. Yellowish coloration of mucous membranes, conjunctivae, and skin 2. Dark urine (bilirubinuria) 3. Hepatomegaly (enlarged and tender liver) 4. Elevated liver enzymes 5 Complete recovery VERSUS development of chronic infection Complete recovery Chronic infection About 90-95% 10% Children under 6 years of old 50-70% 30-50% Infants 10-20% 80-90% Adults Note: after many years, about 20–30% of adults who are chronically infected will develop cirrhosis and/or liver cancer. Fulminant hepatitis: About 1-2 % of acute hepatitis caused by HBV infection, a potentially fatal severe liver inflammation, known as fulminant may develop. Fulminant hepatitis is characterized by: Extensive liver necrosis Abdominal pain High fever and seizures Death rate of individuals that develop fulminant hepatitis: about 8 % Why some individuals with acute HBV primary infection develop fulminant hepatitis? Not-well understood, but it can be: 1- Due to co-infection with HDV or another hepatitis virus (for example, HCV) 2- Due to an uncontrolled immune response that causes massive liver damage 6 Monitoring the course of primary HBV infection…..Recovery versus Development of chronic infection Indications of active HBV infection: During the incubation period and before the appearance of complete viral particles in the blood stream, HBsAg and HBeAg along with elevated levels of liver enzymes are detected. After that, HBV genome, HBV DNA polymerase and eventually complete HBV particles are detected in the blood stream. Monitoring the appearance of anti-HBV antibodies and clearance of viral antigens: Initially, anti-HBc-antibodies (HBcAbs) are detected. Detection of these antibodies cannot tell whether the patient is going to recover or is going to become chronically infected Anti-HBeAg antibodies (HBeAbs) and anti-HBsAg antibodies (HBsAb) appear during late stages of infection. The detection of these antibodies, in association with the clearance of their corresponding antigens (HBeAg and HBsAg) indicates that the patient is recovering from HBV infection (convalescence stage). What indicates that HBV-infected individual is becoming chronically-infected? Persistence of of HBsAg in the blood stream for more than six months and absence of anti-HBsAg indicates that the infection has become chronically (chronic carrier). Primary HBV Infection Chronic infection (Symptomatic or Asymptomatic) Adults 10% Children under 6 years of old 30-50% Infants 80-90% Chronic HBV infection may result in the development of liver cancer or liver cirrhosis Chronic HBV infection is characterized by chronic inflammation that is associated with chronic liver cell injury Continuous re-generation (division) of liver cells so as replace injured cells 7 Chronic inflammation generates free radicals that cause DNA damage In addition, it has been found that the genome of HBV may integrate with host cell genome resulting in insertional mutations that may affect genes involved in cell cycle regulation. This may lead to liver cirrhosis and/or liver cancer Laboratory identification: Detection of viral antigens, antibodies and nucleic acids Testing the serum level of liver enzymes and bilirubin Assessment of prothrombin time Treatment: α-interferon Prolonged treatment with α-interferon suppresses HBV replication in about one third of the patients; however, in some of these patients, HBV replication becomes active again after discontinuance of the therapy. Antiviral drugs: Lamivudine (reverse transcriptase inhibitor) 8 Prevention: Subunit vaccine: by sing HBsAg, which can be given both prior exposure as and post exposure. Note: Post-exposure vaccination is possible because HBV infection has a long incubation period. Passive immunization: Can be achieved by using Hepatitis B Immunoglobulin (HBIG), which is prepared from the blood of donors having a high titer of anti-HBs antibody. HBIG can be given in association with the vaccine in an attempt to interfere with the establishment of infection in individuals exposed (or suspected to be exposed) to HBV. Fortunate neonates that are born uninfected to mothers that are infected with HBV, must also be given HBIG in association with the vaccine in an attempt to interfere with the establishment of infection (bearing in our minds that the neonate may have been exposed to the virus during birth or or the baby may get infected while being breast-fed by the infected mother) 9 Hepatitis D Virus (Delta Agent): Hepatitis D virus (HDV) is a defective virus that requires HBV as its helper virus It infects only humans that have been already infected by HBV or infect humans along with HBV simultaneously Its significant can be seen in the in more severe acute hepatitis that may happen, in association with a greater risk of fulminant hepatitis. If a chronic infection as established (HBV and HBV), it can be associated with a very high risk for the future development of liver cirrhosis and liver cancer. Structure and replication: HDV does not fall into any known group of the human viruses It has a circular, single-stranded RNA genome with negative-polarity. HDV genome codes for one protein, known as the delta antigen The delta antigen is usually found associated with the viral genome. Together, they form what is called the nucleoprotein, which is enclosed within an envelope. The envelope of HDV contains one protein that is not encoded by HDV genome. This protein is HBsAg, which is obtained from a co-existing HBV (helper virus). This explains that HDV infects only humans that previously infected with HBV or infects human along along with HBV (both together). 10 Transmission: Same as HBV (however, transmission by sexual contact may not be as frequent as HBV) Pathogenesis: as in other hepatitis viruses Simultaneous primary co-infection with both HBV and HDV: Co-infection with both HBV and HDV may result: Two episodes of jaundice may be seen More extensive liver damage (higher rate of fulminant hepatitis) Higher risk for the development of chronic infection Higher risk for the developing HCC and liver cirrhosis Primary HDV infection of a (previously-infected) chronically HBV-infected individual: This can lead to: An episode of severe acute hepatitis, with increased of fulminant hepatitis as well as increased risk of developing chronic HDV infection (along with chronic HBV infection) Increase risk of developing HCC and liver cirrhosis later on during life-time Laboratory identification: Detection of the delta (D) antigen of HDV and anti-Delta antigen antibodies Detection of HDV nucleic acid Treatment and Prevention: No specific treatment for HDV infection is available. Because HDV depends on co-infection with HBV, HBV vaccine, which can confer protection from HBV infection can also confer protection from HDV 11