* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 4. In-Class Worksheet Answers - CIM
Survey
Document related concepts
Transcript
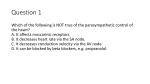
In-Class Answers Session 3 HEART PHYSIOLOGY II M.A.S.T.E.R. Learning Program, UC Davis School of Medicine Date Revised: Jan 16, 2002 Revised by: Gordon Li and Carolyn Nguyen 1. What effect will an increase in venous return have on End Diastolic Volume, strength of ventricular contraction, and stroke volume? What effect will mitral stenosis have on these things? Diagram on lengthtension and pressure-volume graphs. Venous return determines preload, and preload is determined by EDV. Therefore as VR so does EDV. We know that Starling’s Law says a muscle stretched generates more force so a in preload (stretch) forcs (contraction), and SV . It makes sense because in the normal hear blood in blood out so SV must . Less blood gets through a stenotic valve so mitral stenosis preload and has the opposite effect. 2. What are possible causes of increased afterload and what effects do they have on SV? Diagram on lengthtension and pressure-volume graphs. Afterload is the resistance which the heart must overcome to eject blood. This is determined by aortic pressure, but can be modified by changes in ventricular radius and wall thickness as dictated by the Law of LaPlace. This can be increased by hypertension or aortic stenosis, which results in a SV. The SV is because muscle can shorten less against a greater resistance. 3. Diagram the effect norepinephrine on length-tension and pressure-volume graphs. Norepinephrine contractility via interaction with -receptors, therefore SV. In class Answers --MASTERS Heart Physiology II--Session 3 1 4. What is mean systemic filling pressure? Central Venous Pressure? What happens to these when the heart is stopped? What happens to the pressure in the arterial system when the heart is stopped? MSFP is the driving pressure moving blood toward the right atrium. CVP is mean right atrial pressure. When the heart is stopped and cardiac reflexes are inhibited, CVP rises to meet MSFP and venous return stop, because the venous return is determined by MSVP – CVP. 5. Describe the autonomic control of vascular smooth muscle. What are the actions of the sympathetic and parasympathetic nervous system? What is the distribution of their receptors? (Note: the table below is somewhat simplified, but gives the overall gist of the distribution and functions of Symp and PSymp receptors). Nerve Post-ganglionic Transmitter Receptor 1 Sympathetic Parasympathetic Nerve Norepinephrine (except at sweat glands) Acetylcholine Pre-ganglionic Transmitter 1 2 muscarinic Receptor Distribution Actions Vascular smooth muscle (in all organs) Radial muscle of iris GI and GU sphincters Heart muscle cells Vascular smooth muscle in skeletal muscle Vasoconstriction and contraction of smooth muscles (weak effects on coronary and cerebral vessels) HR, contractility Vasodilation (but note that most of the vasodilation in muscle during exercise is due to metabolites!) bronchodilation Vasodilation Bronchiolar smooth muscle Cranial-sacral distribution; oral cavity, tongue, salivary glands, external genitalia; virtually no role in regulation of systemic blood pressure Heart Bronchiolar SM GI SM Secretory glands HR ( contractility, small effect) bronchoconstriction increased motility increased secretion Distribution Sympathetic Acetylcholine Nicotine Autonomic Ganglia and adrenal medulla Parasympathetic Somatic Acetylcholine Acetylcholine Nicotine Nicotine Autonomic ganglia Neuromuscular Junction Firing of post-ganglionic neurons/secretion of catecholamines Firing of post-ganglionic neurons Contraction 6. Name the short-term regulator of mean arterial pressure. Where are the sensors located? Describe the effect of increased blood pressure on this reflex. Why does it only have a short-term effect? The baroreceptor reflex is responsible for short-term BP regulation. It consists of stretch receptors in the carotid sinuses and the aortic arch. The sensory axons from the aortic baroreceptors travel in the vagus nerve; and those from the carotid baroreceptors travel in the glossopharyngeal nerve to the Cardiovascular center in the solitary tract nucleus of the medulla oblongata in the brainstem. Some of these baroreceptor afferents are tonically active at normal mean arterial pressure (MAP). Increased blood pressure leads to increased discharge, leading to reflex changes, as follows: Decreased HR (increase parasympathetic, decrease sympathetic to SA node) Decreased contractility (decrease sympathetic discharge to ventricular muscle) Increased venous compliance (decrease sympathetic discharge to the veins), hence reduced stroke volume. Lower total peripheral resistance ( decrease sympathetic discharge to the arterioles). The baroreceptor reflex is only a short-term regulator of blood pressure because the receptors adapt by raising the threshold and lowering discharge rate. 7. Explain long-term control of arterial pressure in terms of an increased and decreased pressure scenario. Include the important messenger peptides. Long-term control of arterial pressure is performed by the kidneys. An increase in blood volume is sensed by the heart as an increase in stretch in the right atrium. The heart releases Atrial Natriuretic Peptide In class Answers --MASTERS Heart Physiology II--Session 3 2 (ANP) which acts directly on the kidneys. Na+ is excreted in the urine and water follows it, dehydrating the body (natriuresis). ANP also lowers blood pressure by decreasing the responsiveness of vascular smooth muscle to vasoconstrictors, and decreasing the responsiveness of the adrenal zona glomerulosa cells to stimuli thereby decreasing aldosterone release. ANP also lowers the release of Antidiuretic Hormone (ADH) from the posterior pituitary gland. A decrease in blood volume, on the other hand, leads to a decrease in renal blood flow pressure. The kidney then secretes Renin which converts Angiotensinogen (produced by the liver) to Angiontensin I, which is consequently converted to Angiotensin II in the lungs. Angiotensin II then stimulates the adrenal cortex to release aldosterone. Aldosterone acts to retain Na+ in the kidneys, thus conserving ECF volume and reducing further loss of blood volume. ADH (aka vasopressin) is also secreted from the posterior pituitary in response to loss of blood volume (usually when the loss is significant), and causes direct vasoconstriction as well as increased reabsorption of water in the kidney. 8. Describe the reflex compensations when someone suddenly stands up from a supine position. What would happen in a patient who just had a sympathectomy? Sudden standing causes pooling of blood in the leg veins. This results in decreased venous return to the heart, which leads to decreased cardiac output (Frank-Starling mechanism), which leads to decreased MAP. This decrease in MAP is detected by the carotid sinus baroreceptors, which relay a message to the medullary cardiovascular control center, which increases sympathetic outflow and decreases parasympathetic outflow, this causes: An increase in HR and myocardial contractility, tending to restore cardiac output. Vasoconstriction in skeletal musculature, skin, kidneys and gut, reducing blood flow to these organs and increasing TPR. Venoconstriction decreasing capacitance and increasing venous return A patient with a sympathectomy would experience what's referred to as orthostatic hypotension (which might lead to syncope). Orthostatic hypotension is a decrease in arterial pressure when going from supine to a standing position. A person with a normal baroreceptor mechanism will try to restore MAP. In a person who had a sympathectomy, the sympathetic component of the baroreceptor mechanism is absent. 9. Will the capillary pressure increase or decrease in the following situations? a) Arteriolar vasodilation: increase b) Venodilation: decrease (however, Dr. Gray points out that capillary beds of lower extremities will experience an increase in pressure due to back pressure exerted by the column of blood in the dilated veins!) 10. Describe the compensatory mechanisms following a hemorrhage. Following a hemorrhage, three main parameters are decreased: i) Stroke volume (SV) ii) Cardiac output (CO) iii) Mean arterial pressure (MAP) Carotid Sinus baroreceptors will immediately kick in; fast neural responses are the same as those which follow a change from the supine to the standing posture, but are of greater magnitude. Don't forget, chemoreceptors in the carotid and aortic bodies will supplement the baroreceptor mechanism by increasing sympathetic outflow. To make up for the deficit in blood volume, interstitial fluid will be transferred into the capillaries. Why? Because of reduced capillary pressure resulting from hypotension and vasoconstriction. Also short-term is the adrenal medulla's release of epinephrine and norepinephrine, which supplement the action of the sympathetic nervous system. In the next few hours, the kidneys will increase water and sodium retention. Remember how? Decrease in renal perfusion pressure activates the renin-angiotensin-aldosterone system. Angiotensin II is a potent vasoconstrictor, aldosterone increases salt and water reabsorption in the kidney. ADH is also released when atrial receptors detect the decrease in blood volume. ADH causes vasoconstriction by acting both locally as well as centrally, and increased water reabsorption in the In class Answers --MASTERS Heart Physiology II--Session 3 3 kidney. ADH also stimulates the thirst response; if this is quenched, it will lead to further restoration of blood volume. Finally, because of reduced hydrostatic pressure in capillaries, fluid will redistribute from interstitial space into the capillaries over a period of hours to days. (This will be covered next week). Optional Questions 11. How does the skeletal muscle venous pump work? What is another important "pump" that works similarly? Skeletal muscle venous pump relies on the presence of venous valves. During activities such as exercise or walking, the alternating contraction and relaxation of the skeletal musculature help return blood to the right atrium. Contraction propels blood towards the heart; retrograde flow is prevented by venous valves. When the musculature relaxes, inflow dilates the vein. The cycle repeats. Another similar pump is the respiratory venous pump which also relies on the venous valves and alternating contraction and relaxation that accompany breathing. The descent of the diaphragm increases abdominal pressure and decreases intrathoracic pressure, thereby increasing the pressure difference between the periphery and the right atrium. 12. What is vasomotor tone? Is there venomotor tone? There is, normally, a sympathetic tonic discharge to arteriolar smooth muscle which gives a "background " of vasoconstriction. This is vasomotor tone. This varies from organ to organ and contributes to the differing amounts of blood flow each organ receives. Similarly, smooth muscle in the venous system also has alpha-l adrenoreceptors which are innervated by the sympathetic nervous system. This is venomotor tone. A decrease in sympathetic activity, therefore, leads to venodilation and increasing venous capacity (and decreasing venous return). 13. What is the mechanism by which calcium affects vascular smooth muscle contraction? Four Calcium ions bind to four sites on Calmodulin forming a Calcium-Calmodulin Complex, which then binds to an inactive myosin light chain kinase. The whole thing becomes an active holoenzyme. This activated enzyme catalyzes the phosphorylation of myosin. Myosin-P interacts with actin and causes contraction. 14. What is the effect of vascular radius and blood viscosity on arteriolar resistance? Explain in terms of the Poiseuille equation. R 8L r 4 An increase in blood viscosity is directly proportional to the resistance so that a doubling of the viscosity will cause a doubling of the arteriolar resistance. The resistance is inversely proportional to the fourth power of the radius so that halving the radius results in a 16-fold increase in resistance. 15. Knowing what you know about sympathetic innervation to the heart and blood vessels, and about cardiovascular reflexes, can you explain how alpha-blockers, beta-blockers, and ACE (Angiotensin Converting Enzyme) inhibitors work in treating essential hypertension (HTN)? Beta-blockers block the 1 adrenoreceptors on the heart and reduce cardiac output (CO). They also reduce sympathetic outflow from the CNS, inhibit the release of Renin from the kidneys (therefore reducing Angiotensin II. Recall Angiotensin II’s effect on the TPR and blood volume) Alpha-blockers competitively block 1 adrenoreceptors. They decrease peripheral vascular resistance and lower arterial blood pressure by causing the relaxation of peripheral vessels. Reflex tachycardia is a common side effect due to activation of the baroreceptor reflex. ACE inhibitors: Remember that Angiotensin II is also a potent vasoconstrictor. By blocking its production, one gets a lower degree of vasoconstriction as well as decrease secretion of aldosterone, resulting in decreased Na+ and water retention. In class Answers --MASTERS Heart Physiology II--Session 3 4