* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Approved
Survey
Document related concepts
Transcript
Approved
on the conference of the Department
of Obstetrics and Gynecology with the Course
of Infant and Adolescent Gynecology
“____” _____________200 p.
protocol No
T.a.The Head of the department, Professor
O.A.Andriiets’___________
Methodological instruction
on the themes singled out for independent study
“General symptomatology of gynecologic diseases”
Subject-gynecology
For 5 year students of medical
faculty
2 academic hours
Developed by assistant, PhD
Oksana Bakun
Chernivtsi, 2008
I. Scientific and methodical grounds of the theme
Examination of gynecological patient consists of history taking, objective
(general and special) and additional methods of examination. The examination
begins with obtaining the history in accordance with a certain plan. First of all, the
passport data is required: surname, name, patronymic ,and also birth date
(woman’s age). This is done because each phenomenon in different age of women
lifecycle can have different meaning, for example, absence of menses in young
women and women in menopause.
II. Aim:
A student must know:
1. Abdominal examination.
2. Vaginal examination.
3. Rectal examination.
4. Cervical smears for exfoliative cytology.
5. Further gynecological investigations.
A student should be able:
1. To carry out an objective gynecologic examination of a patient.
1. To make up a plan of a patient’s examination.
III. Recommendations to the student
THE PHYSICIAN-PATIENT RELATIONSHIP
Patient Motivation and Comfort
Because people seek medical care for several reasons, it is important for the
physician to understand why the patient is in his or her office A failure to do so
may lead to dissatisfaction on the part of the patient For example, a patient may
come to the gynecologist's office with a stated complaint of pelvic pain and an
unstated fear that the pain is being caused by a sexually transmitted disease If the
physician focuses on evaluating the pain and provides effective analgesia but does
not uncover the underlying problem, the patient may leave the office pain-free but
dissatisfied. Therefore, the physician should make several attempts during the
course of the history and examination to determine why the patient made the
appointment and what issues the patient needs to have addressed during the office
visit In addition to understanding and meeting the pa tient's needs, the physician
must be prepared to provide a medical evaluation in a physically and emotionally
comfortable setting. A woman's initial visit to the gynecologist's office can be
fraught with anxiety, concern, and even humiliation. Whatever her age, social
background, or previous experience (all of these influence her reaction), she often
expects the encounter with the gynecologist and the examination to be
uncomfortable both emotionally and physically. Unfortunately rumor and previous
experiences may have given this anxiety a very real foundation. It is the physician's
responsibility to allay undue apprehension, dispel false impressions, and make the
visit as comfortable and informative as possible so that the patient leaves the office
calm and in an improved frame of mind. This is best achieved by an understanding
attitude and a matter-of-fact approach. Condescension and domination have no
place in the physician-patient relationship.
Even under the best of circumstances the patient is likely to find the visit
disagreeable. Soon after entering the office or clinic she is asked to discuss her
most personal problems, which she has mentioned to few, if any, others. Then,
after verbally exposing herself, she must undress, put on the most unappealing of
garments, and be examined by a stranger. No wonder the visit to the gynecologist
for an annual check up or for help with a pressing problem is seldom anticipated
with enthusiasm. Indeed, subsequent visits are usually as trying as the first.
The patient is sensitive to subtle nuances in the physician's words or facial
expression, a fact seldom appreciated by the busy practitioner. The physician's
demeanor is extremely important in allaying the patient's anxiety and establishing
rapport; the physician who appears abrupt, preoccupied, hurried, hesitant,
embarrassed, or flippant can destroy the possibility of a satisfactory physicianpatient relationship. Frivolity and lightheartedness rarely have a place in the initial
evaluation. The seriousness of the moment for the patient should be foremost in the
physician's mind. Propriety of address and composure are qualities that all patients
appreciate and respect. The physician should express sincere concern in a friendly,
direct atmosphere.
There are other rules for the relationship of an obstetrician-gynecologist with
the patient. Unless the patient gives permission to call her by her first name, the
physician should address her by her last or surname. Use of surnames also has a
practical value, for a midnight call from "Janet" may be recognized less quickly
than a call from "Janet Henderson" or "Mrs. Henderson." While conducting the
examination the physician should not think out loud, articulating possible
diagnoses, for needless and disturbing explanations may be required later.
Finally, the physician should evaluate the patient's attitude and make every
effort to adjust to it. Although some patients may appreciate a casual and relaxed
style, others are more comfortable and confident when the physician is serious and
formal. Patients will not alter or adjust their personalities to conform to the wishes
of the physician; any adjusting that is needed must be done by the physician.
The physician can do several things to reduce the patient's anxiety. First, the
history should be obtained in as comfortable and private a setting as possible; the
patient should be clothed and seated at the same level as the physician, especially if
she is meeting the physician for the first time. A patient may choose to change into
an examination robe before seeing the physician if the visit is for a follow-up
examination. Under most circumstances she should be interviewed alone.
Exceptions may be made for children, adolescents, and mentally impaired women,
or if the patient specifically requests that an attendant or family member be
present. Even in these situations it is usually a good idea to give her an opportunity
to speak with the physician privately.
Second, the initial portion of the interview should be designed to put the
patient at ease. This can often be accomplished by discussing neutral and
nonmedical subjects such as recent recreational activities, employment, or family.
This should not, however, be viewed merely as a means of relaxing the patient, but
rather as an opportunity for the physician to relate to the patient's psychological
and social dimensions.
Finally, the physician should not make assumptions about the patient's
background. For example, physicians usually assume that all adult female patients
are both sexually active and heterosexual. Either or both may not be true.
Therefore, asking neutral and open-ended questions (e.g., "Are you sexually
active?" or "Are you having sex with men?") will let the patient know that you
have not made these assumptions.
In addition to these aspects of the patient-physician interaction, patient
satisfaction is also related to the time required to get an appointment, the patient
mix in the reception area, the length of waiting time in the reception or
examination room, the attitude of the office staff, and the billing procedures.
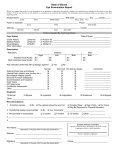
PATIENT HISTORY. When large numbers of patients are involved, as in a clinic
setting or in a very busy office, certain basic information (e.g., age, ethnic
background, marital status, obstetric history, and whatever the patient may want to
divulge about the problem for which she consults the physician) is often obtained
by interview with an office nurse or by a questionnaire the patient is asked to fill
out. Although these devices are sometimes considered essential, it is astonishing
how little time they really save; by obtaining these data personally the physician
provides a logical opening for the interview and establishes a preliminary rapport
with the patient. In addition, the manner in which she answers these mundane
questions may alert the physician to areas that should be probed more deeply.
The setting for the history taking is important. A quiet area in which
distractions (telephone calls, interruptions) can be kept to a minimum and in which
privacy is ensured promotes a comfortable dialogue between physician and patient.
The foundation for rapport in a continuing relation can be established during these
15 to 30 minutes of the initial history taking. This is perhaps the most critical time
the physician spends with most patients.
Overview
The history provides information about the total patient and is perhaps the
most important part of the gynecologic evaluation. It enables the woman to become
acquainted with the physician in a nonthreatening situation. In most cases it gives
the physician data to establish a tentative diagnosis before the physical
examination. In many respects the gynecologist who takes a history is like the
detective who keeps the various clues that are pertinent and discards those that are
deliberately or inadvertently misleading. If the gynecologic history is sufficiently
penetrating, it should in almost all cases permit the physician to narrow the likely
possibilities to one or at most two probable diagnoses. This preliminary opinion
may not always be correct, but the history-taking session should not be ended until
a tentative diagnosis has been made.
Like a hospital chart, the office history is a legal, as well as a medical, record.
As such, it is subject to subpoena, and whatever is recorded in it may at some
future date need to be defended in court. It should not contain extraneous or
casually written material, and the notes should be sufficiently complete that the
case can be readily reconstructed.
The gynecologic history should include the following information:
I. Presenting complaint
A. The primary problem
B. Duration
C. Severity
D. Precipitating factors
E. Occurrence in relation to other functions(menstrual cycle, coital activity,
gastrointestinal activity, voiding, or other pertinent functions)
F. Any previous similar symptom and itsdiagnosis and management
G. Change in normal life-style resulting fromthe complaint
H. Outcome of previous therapies
II. Menstrual history
A. Menarche
B. Frequency of menstrual periods
C. Regularity of menstrual flow
D. Date of onset of last menstrual period
E. Precipitating factors
F. Duration of flow
G. Degree of discomfort
H. Quantity of menstrual flow (number of pads used per day)
I. Premenstrual symptoms
J. Contraception (current and past methods)
K. Obstetric history
L. Number of pregnancies
M. Number of living children
N. Number of abortions, spontaneous or induced
O. History of previous pregnancies (duration of pregnancy, antepartum
complications, duration of labor, type of delivery, anesthesia used, intrapartum
complications, postpartum complications, hospital, physician) P. Perinatal status of
fetuses (birth weights, early growth and development of children, including
feeding habits, growth, overall well-being, current status)
III. Past medical history
A. Allergies
B. Medications currently used
C. Medical problems for which care has been required
D. Hospitalization
IV. Surgical history
A. Any operative procedures: outcome, complications
V. Review of systems
A. Pulmonary symptoms
B. Cardiac symptoms
C. Gastrointestinal symptoms
D. Urinary symptoms
E. Vascular symptoms
VI. Breast symptoms
A. Masses
B. Galactorrhea
C. Pain
D. Family history
VII. Social history
A. Exercise
B. Dietary habits
C. Drug use
D. Alcohol use
E. Smoking habits
F. Marital status
G. Number of years married
H. Coital activity (libido, dyspareunia, orgasm)
I. Occupational history (exposure to environmental toxins)
VIII. Family history
A. Significant medical and surgical disorders in family members
Presenting Complaint
It is best to begin the history with an open-ended question that will elicit any
symptoms the patient may have. Then ask the patient to describe the problem in
her own words. Less information will be obtained if the interviewer asks only
focused, closed-ended questions to which the patient can answer yes or no.
However, it is necessary for the interviewer to have an outline for questions about
the gynecologic history in order to obtain all the necessary information. The
following is a list of questions that are typical of a gynecologic history.
What were the circumstances at the time the problem began {time, place,
activity, cycles)? What has been the sequence of events? Often the use of a
calendar to refer to will aid the patient. Have you had this problem before? If the
patient answers yes, then ask for the description of the previous occurrence and
what led to its disappearance. To what extent is the problem interfering with your
daily life and the life of your family? Have you had previous evaluations or
treatments? Records from previous physicians may be helpful. Why did you seek
evaluation of the problem now? What questions do you want answered today?
What do you expect and want from today's visit?
Menstrual History
The cycle interval is counted from the first day of menstrual flow of one cycle
to the first day of menstrual flow of the next cycle. Many women count their cycle
from the end of one period to the beginning of the next.
The range of normal is wide, and a recent change in usual pattern may be a
more reliable sign of a problem than the absolute interval. Although 28-day cycles
are the median, only a small percentage of women have cycles of that length. The
normal range for ovulatory cycles is between 21 and 35 days. Cycle length remains
relatively constant over the reproductive years for each woman.
Estimation of the amount of menstrual flow by history is difficult. The
average blood loss is 30 ml, with a range between 10 ml and 80 ml. Birth control
method usually affects the amount of blood loss, for oral contraceptives cause a
decrease and intrauterine devices cause an increase. An increase in the number of
tampons or pads used (> one per hour for six or more hours) and the passage of
blood clots are signs of excessive blood flow.
Dysmenorrhea is common. It usually begins just before or soon after the onset
of bleeding and usually subsides by the second or third day of flow. The
discomfort is characteristically midline and is often associated with backache and,
in the case of primary dysmenorrhea, with systemic symptoms such as lightheadedness, diarrhea, nausea, and headache.
Sexual History
Although there are many models for sexual histories, most are not appropriate
for the nonpsychiatric physician or in the setting of a brief office visit. However, a
model for office practice has been developed and detailed by Munjack and Oziel,
who describe two types of sexual histories: a screening history and a problemoriented history. The screening history is brief, and suited for inclusion in the
comprehensive medical history that is often part of a patient's first visit to her
gynecologist. The problem-oriented history is more detailed, and designed to
investigate those problems identified by the screening history.
The screening history is designed to determine whether there are any major
sexual difficulties that need in-depth evaluation and therapy, and whether the
physician can deal with the problem or whether it should be referred elsewhere for
more intensive evaluation. In an attempt to put the patient at ease the physician can
begin the sexual history by prefacing his questions with statements such as, "Most
people experience ..." or "Because sexual problems can develop as part of other
gynecologic problems ..." In addition, if the physician can convey a willingness to
help, the patient is more likely to discuss any problems she may have. Finally, the
screening history should begin with a discussion of topics that are unlikely to
provoke anxiety. For example, questions about the occurrence of pain during
intercourse are less likely to cause anxiety than questions about orgasmic function
or noncoital sexual practices.
The problem-oriented sexual history should include the following topics:
Onset of the problem
Course of the problem
Conditions that decrease or increase the severity of the problem
Previous evaluation of the problem and the results of such evaluation
Previous treatment of the problem and the results of such treatment
Severity of the problem
Patient's reaction to the problem
Impact of the problem on the patient's sexual relationships
Patient's sexual attitudes and upbringing
Patient's sexual practices
Quality of patient's sexual and/or marital relationship
A rational treatment or referral plan can be formulated on the basis of
discussion of these and related questions.
In addition to obtaining a history of sexual dysfunction, it is also important to
obtain a history of any sexually transmitted diseases. The physician should
question the patient about past episodes of sexually transmitted diseases, sexual
practices, number of sexual partners, sociosexual background of sexual partners,
use of barrier forms of contraception, use of intravenous drugs, previous blood
transfusions, genital lesions, persistent vaginal discharge or pelvic pain.
General Medical History
Because many gynecologic patients want to conceive sometime in the future,
a general medical history and social history should also be obtained. Women
contemplating pregnancy benefit from prepregnancy counseling, and effective
counseling can be performed only when there is knowledge and identification of
medical and social conditions that place mother and fetus at risk. The following
medical and social conditions should be evaluated during the gynecologic history.
I. Genetic disorders
A. History of birth defects
B. History of habitual abortion
C. History of stillbirth or neonatal death
D. History of infertility
E. History of environmental exposure
Infections
X-rays
Drugs (e.g., lithium, alcohol, warfarin, retin A, anesthetic gases
F. History of consanguinity
G. Genetic disease in the mother
Sickle cell anemia
Porphyria
Phenylketonuria
Von Willebrand's disease
Myotonic dystrophy
Ehlers-Danlos syndrome
Monfaris disease
Chondrodystrophies
H. History of advanced maternal age
II. Endocrine and metabolic diseases
A. Diabetes mellitus
B. Thyroid disease
C. Obesity
D. Anorexia nervosa—bulimia
E. Galactorrhea
F. Hirsutism—acne
III. Cardiovascular disorders
A. Rheumatic heart disease
B. Congenital heart disease
C. Mitral valve prolapse syndrome
D. Ischemic heart disease
E. Venous thromboses and embolism
F. Hypertension
IV. Hematologic disorders
A. Inherited coagulopathies
Hemophilia carrier
Platelet defects
B. Red blood cell defects
V. Renal disorders
A. Polycystic disease
B. Chronic pyelonephritis
C. Congenital anomalies
D. Systemic lupus erythematosus
E. Renal transplantation
VI. Neurologic disorders
A. Multiple sclerosis
B. Neural tube defects
C. Spinal cord injuries
D. Myasthenia gravis
VII. Genitourinary disorders
A. Congenital mullerian anomalies
Diethylstilbestrol exposure
Fusion defects
B. Dysuria
C. Incontinence
D. Prolapse
VIII. Gastrointestinal disorders
A. Liver disease
B. Functional bowel syndrome
IX. Social factors
A. Alcohol use
B. Tobacco use
C. Recreational drug user
D. Occupational hazards
E. Dietary practices
Finally, the perimenopausal and postmenopausal woman has gynecologic and
medical problems that are unique to her age and require special attention. In
addition to the questions discussed above, the menopausal woman should be
evaluated for the effects of estrogen deficiency, including vasomotor symptoms,
vaginal dryness and dyspareunia, ischemic heart disease, and osteoporosis.
Questions about the patient's emotional status, social support system, financial
status, diet, and exercise level may also provide information that will aid in the
management of these unique menopausal problems.
THE GYNECOLOGIC EXAMINATION. It is important for the obstetriciangynecologist to know the physical condition of the patient. A complete physical
examination and appropriate laboratory tests should be performed at the first visit.
A complete physical examination may or may not be part of the subsequent office
visit of the gynecologic patient. For the woman in good health who has consulted
an internist recently or is under the care of an internist for some ongoing disorder
such as hypertension or diabetes, a complete physical examination may not be
needed. For the woman with an endocrine disorder, a complete physical
examination clearly should be part of the gynecologist's evaluation. The
designation of the obstetrician-gynecologist as a "primary physician for women" is
variously interpreted by the practitioners of this discipline. An important part of
this responsibility is referral to other physicians for such special examinations as
may be needed. Except for the breasts, which should be examined at every
gynecologic visit, the detail of the physical evaluation of gynecologic patients
varies according to the circumstances.
On entering the examining room the physician should make some brief
comment to put the patient at ease, but to expect the patient to "relax" is probably
out of the question. During the physical examination another woman participant,
usually a nurse or aide, must be present. Not only can this woman assist the
physician, but she also lends an element of psychological support to the patient.
Her presence is also of legal importance to the physician as a guard against
accusations that may be initiated by an unscrupulous or disturbed patient. The
dialogue between physician and patient should continue during the examination.
Distracting conversation with the nurse or aide tends to influence the patient
adversely and detracts from the physician-patient rapport.
Evaluation of General Appearance
Examination of the Head and Neck
Examination of the Cardiopulmonary System
Examination of the Breast
Examination of the Chest
Examination of the Abdomen
Examination of the Extremities
The Pelvic Examination
The first pelvic examination should probably take place in the neonatal
period. Certainly an examination is indicated at any time there is abnormal
bleeding, pelvic symptoms, or questions about primary or secondary sexual
development, or with the initiation of sexual activity. For the teenager the first
pelvic examination should probably occur between ages 18 and 21. Examinations
should then be repeated at yearly intervals at which time a Papanicolaou test (Pap
smear) should be performed in addition to a pelvic examination and a screening for
breast cancer and hypertension.
The pelvic examination provides the physician with an opportunity to dispel
myths and misunderstandings and to educate with respect to pelvic anatomy,
physical development, and sexual function. Often the patient is reassured if the
physician carries on a running dialogue with her describing the findings, asking
and answering questions, and, on occasion, demonstrating physical findings with
the aid of a hand-held mirror. There are several things a physician can do to
maximize the educational aspects of an examination. First, explain all procedures
in advance. Second, when possible, keep eye contact with the patient during the
examination. Third, give the patient choices when possible (e.g., whether or not to
use a drape, or the option to delay parts of the examination if discomfort is
encountered). Fourth, explain all findings clearly.
Patient Preparation
The pelvic examination is performed with the patient lying on her back with
both knees flexed. The buttocks are positioned at the edge of the examining table,
and the feet are supported by stirrups. This position allows the necessary exposure
to the pelvic organs.
Traditionally, the patient has been placed with the head and body in a
horizontal position. This position does not allow the physician to maintain eye
contact with the patient and increases the patient's sense of vulnerability. The
alternative, assuming the availability of an adjustable examination table, is to
elevate the head of the table between 30 and 90 degrees. There are no apparent
technical disadvantages to this alternate position, and many patients find it easier to
relax, actually making the bimanual part of the examination more accurate. The
patient should also empty her bladder just before the examination.
Equipment
The minimal equipment needed to perform a pelvic examination includes a
good light source, a speculum of the correct size, a nonsterile glove, and a watersoluble lubricant. Additional supplies that should be available in the examination
room include a variety of speculum sizes; materials to obtain cytologic samples,
including fixative; various culture media; large cotton-tipped swabs; pH indicator
paper; and a screening test for fecal occult blood (e.g., Hemoccult). Specialized
examinations require other specific equipment.
External Genitalia
The pelvic examination begins with inspection of the vulva. The physician
should note and record any evidence of developmental abnormalities as well as the
general state of cleanliness, discharge, hair growth and distribution, and any
abnormalities of the skin, including tumors, ulcerations, scratch marks, rashes, and
minor lacerations or bruises Any vulvar varicosities or hemorrhoids should also be
noted A careful inspection of the skin folds and the pelvic hair may also reveal
occult disease or infection The vulva should also be palpated for subcutaneous
lesions
The labia are then spread, and the condition of the hymen, size of the clitoris,
and condition of the vulvovaginal skin noted. The area of the Bartholin's, the
periurethral, and Skene's glands should be palpated, and the urethra should be
palpated along its length for a caruncle, diverticulum, or infection. After asking the
patient to contract the muscles of the vaginal opening to assess the tone of the
levator muscles and the degree of perineal support, the patient is asked to strain,
and the presence of a urethrocele, cystocele, rectocele, enterocele, or prolapse of
the vagina or cervix is noted.
Vaginal Examination. The vagina should first be inspected with the use of a
speculum Specula come in a variety of sizes, and an appropriate size should be
selected for the individual patient. Usually the largest size that is comfortable
provides the best visualization.
Painless insertion of the speculum may be aided by a number of techniques.
First, the muscles at the opening of the vagina may be relaxed by gentle downward
pressure with one or two fingers. The speculum may be moistened with warm
water before insertion, but other kinds of lubrication should be avoided if either
cultures or cytology is to be obtained. The speculum blades should be inserted
obliquely (but not vertically) through the introitus, immediately rotated to the
horizontal plane, and then slowly opened after reaching the vaginal apex The
vaginal walls and cervix should be inspected for lesions The vaginal discharge
should be assessed for volume, color, consistency, and odor. The endocervical
discharge should also be examined Samples for cervical or vaginal cytology,
cultures, and direct microscopic examination of the vaginal or cervical discharge
should be obtained as indicated. Before removal of the speculum the cervix should
be evaluated for ectropion, erosion, infection, discharge, laceration, polyps,
ulcerations, and tumors. As the speculum is removed and with the patient bearing
down, the degree of vaginal wall relaxation and uterine prolapse can be assessed.
With the speculum removed but with the patient still bearing down, one can
observe if the patient exhibits stress incontinence.
Generally, the physician should acquire proficiency with the index and middle
fingers of one hand and then always use that hand for the vaginal examination.
After the speculum has been withdrawn the physician should gently insert the
index and middle fingers along the posterior wall of the vagina. It is helpful to
place a stool at the base of the examining table and support the examining arm and
elbow during the examination. This support of the elbow allows greater sensitivity
m the examining fingers At the same time a second dimension is added by pressing
on the patient's abdomen with the other hand The first palpable structure is the
cervix. Next is the anteriorly placed uterine fundus The bimanual technique can
outline its position, size, shape, consistency, and degree of mobility. Uterine or
cervical mobility can be further assessed by placing the fingers on one side of the
structure and moving it to the contralateral side. This can be done on both right and
left sides to detect chronic or acute inflammatory changes and fixation. The
abdominal hand is then placed on one lower quadrant and slowly worked menorly
and medially to meet the examining fingers of the vaginal hand In this way adnexal
structures on that side can be appreciated The degree of adherence of an adnexal
structure to the uterus can be ascertained. Enlargement, consistency, and position
of ovaries and tubes can be noted. The ovary is a sensitive structure, and patients
differ in tolerance to palpation. The contralateral side should be similarly
examined. The glove of the examining hand is then replaced with a clean glove for
the rectovaginal examination.
Rectovaginal Examination. A pelvic examination is not complete without a
rectovaginal examination. Although the rectal examination is generally
uncomfortable, it can be less so if the physician places a finger gently into the anal
opening and waits for the anal sphincter to relax before proceeding. The middle
finger is inserted into the rectum and the index finger into the vagina. The
parametrial tissue is palpated between the index finger in the vagina and middle
finger in the rectum. Then the posterior uterine surface, the adnexal areas, the
uterosacral ligaments, and the pouch of Douglas, along with the anorectal area, are
palpated. The rectovaginal examination enhances the evaluation of the cul-de-sac
or ovarian pathology. Particles of hard fecal material may interfere with an
accurate examination.
Rectal Examination. Rectal examination is also useful when a vaginal
examination is impossible, such as in infants and children. The rectal wall is
palpated throughout its circumference and as far as the finger permits. Almost half
' of all rectosigmoid cancers can be detected by this palpation. The finger can also
explore the surface of each pelvic wall, feeling for enlarged nodes or other
abnormalities. The patient should be instructed to slide up on the table while the
lower third of the table is replaced. The examiner then carefully washes his hands
and advises the patient to get dressed. The physician should then step out of the
room to allow the patient to get dressed.
Postexamination Discussion. When the patient rejoins the physician in the
consultation room, diagnosis and findings should be explained in terms she can
understand. The implications of the findings should be carefully detailed. It is
occasionally helpful to have the patient paraphrase what the physician has said to
make certain she understands. This is especially relevant when surgery is
contemplated, for the nuances of an operation and its results may be unclear to the
patient. At this rime the use of medications and the duration of their use must be
explained. The physician should also carefully explain the symptoms that may be
expected after any treatment given during the office visit (e.g., heavy leukorrhea
after cryosurgery or bleeding after cervical biopsy). Advice against coitus should
be given when appropriate, and the duration of abstinence should be made clear.
The importance of a follow-up examination should be stressed. Prescriptions for
hormones should be adequately detailed and restrictions on refills explicitly stated.
DIAGNOSTIC PROCEDURES Pap Smear
The early diagnosis of cervical carcinoma is based on periodic cytologic
examination of the cervix. Despite extensive debates regarding the optimum
frequency and accuracy of the Pap smear, it has become the standard method of
screening for cervical carcinoma. In addition to detecting early cervical cancer, the
Pap smear can also assess hormonal status and identify sexually transmitted
pathogens such as Chlamydia trachomatis and Trichomonas vaginalis.
Pap smears should be obtained at periodic intervals in all sexually active
women. Thereafter, they should probably be obtained yearly, especially in women
who have had coitus with more than one sexual partner, who began to have coitus
as an adolescent, or who has a history of a sexually transmitted disease. They
should be performed annually in women who have had a hysterectomy for pelvic
cancer or in situ disease, but are not necessary in women who have had a
hysterectomy for benign disease.
Colposcopy. Colposcopy aids the physician in the examination of the visible
portion of the female reproductive tract (i.e., vulva, vagina, and cervix). This
technique complements cytologic evaluation and can often localize the source of
abnormal cells seen on cytology. Vulvar diseases amenable to colposcopic
evaluation include human papillomavirus infections (HPV), herpes genitalis, and
preinvasive malignancies. The magnification afforded by the colposcope may aid
the surgeon in selecting areas to biopsy. The application of 3% acetic acid for three
to five minutes may also help to define abnormal areas that often turn white and
display sharp borders (so-called acetowhite epithelium).
The colposcope may also aid in the recognition of clinically inapparent
vaginal intraepithelial neoplasia or HPV infection. These lesions are also
characterized by acetowhite epithelium.
Endometrial Sampling. The recent introduction of new devices for endometrial
sampling has simplified the evaluation of abnormal uterine bleeding. As a result,
the use of dilatation and curettage under general or regional anesthesia has been
replaced in many situations by outpatient endometrial biopsies. The result has been
a savings of money, time, and morbidity.
Before obtaining an endometrial biopsy the physician should obtain an
informed verbal or written consent from the patient. He should then rule out an
intrauterine pregnancy, cervical or endometrial infection, and cervical stenosis.
Patients with valvular heart disease should probably be given antibiotic
prophylaxis.
The size and position of the uterus are determined by a pelvic or ultrasound
examination, and a speculum is placed into the vagina. If the patient is sensitive to
cervical manipulation, a paracervical block can be administered. When endometrial
cancer is suspected an endocervical biopsy should be obtained before the
endometrial sampling. The cervix and upper vagina is then cleansed with an
antiseptic such as povidone-iodine (Betadine).
Vulvar Biopsy. In the past the toluidine blue test was used to direct vulvar
biopsies. The vulva was first washed with 1% acetic acid, dried and treated with
toluidine blue dye. After two to three minutes the dye was washed away with 1%
acetic acid. Areas of possible vulvar intraepithelial neoplasia retained the dye, and
thus guided the physician to suspicious areas for biopsy. Because of the high rate
of false positives and false negatives, the toluidine blue test has been largely
replaced by colposcopy.
The only definitive way to exclude invasion is to biopsy and microscopically
examine any suspicious area of the vulva. Fortunately vulvar biopsies are usually
simple to obtain in the office. The area under suspicion is first cleansed with an
antiseptic solution and infiltrated with 1% lidocaine (Xylocaine) and a 25-gauge
needle. Then a 3- to 4-mm Keyes punch is used to obtain a biopsy specimen. Any
bleeding that occurs can be controlled with silver nitrate sticks or Monsel's solution
and gentle pressure. For larger biopsy areas a single interrupted suture obtains hemostasis.
Ovulation Detection. The confirmation of ovulation is often an important part of
the evaluation of patients with infertility or abnormal uterine bleeding. It is also
useful in timing donor and homologous artificial insemination.
Until recently the methods used to detect ovulation reflected progesterone
secretion by the ovary. Most popular among these was the determination of a
biphasic temperature pattern by recording the basal body temperature (BBT). The
BBT is the patient's temperature taken immediately on awakening and before any
activity. A shift and persistent elevation in the BBT of 0.5°F to 1.0°F in response
to the secretion of progesterone reflects ovulation. However, it reflects ovulation
after it has occurred and does not allow the patient to predict in advance when
ovulation is going to occur.
Others have used measures of serum progesterone or the presence of secretory
endometrium to confirm the occurrence of ovulation. These methods also provide
confirmation of ovulation but do not make it possible for the infertile patient to
predict the day of ovulation for the timing of coitus or insemination.
Serial ultrasound studies of follicular growth and disappearance and
subsequent formation of a corpus luteum is another method of detecting and timing
ovulation. The sonographic changes associated with ovulation include a
preovulatory follicle of 20 mm or more, a change in the shape of the follicle,
thickening of the follicular wall, disappearance of the follicle, and the appearance
of fluid in the cul-de-sac. However, these changes can occur without actual
ovulation, and ovulation can occur without these characteristic changes.
Unfortunately only direct observation of ovulation at laparoscopy, or pregnancy
provides definite evidence of actual ovulation.
Office Hysteroscopy. The development of small hysteroscopes that use carbon
dioxide as a distention medicine has made it possible to determine the cause of
abnormal uterine bleeding, the size and shape of the uterine cavity, the presence of
urogenital anomalies of the uterus, the location of a misplaced intrauterine device,
and the presence of intrauterine adhesions in the office setting, often without
anesthesia. As a result, dilatation and curettage and hysterosalpingography are no
longer always the primary procedure for the evaluation of abnormal bleeding or
intrauterine abnormalities associated with infertility.
The procedure is safe, simple, and quick. The procedure is performed early in
the menstrual cycle to avoid any intrauterine pregnancy or a thick endometrium.
After the patient signs an informed consent, the cervix is cleansed with an
antiseptic solution and a 4-mm hysteroscope sheath and a C02 hysteroscope is
inserted through the cervix, which is secured with a single-toothed tenaculum. The
insertion of the hysteroscope is facilitated by judging the size, shape, and flexion of
the uterus by performing a bimanual examination before the hysteroscopy.
IV. Control questions and tasks
1. What methods are used for special (gynecological) examination?
2. What woman’s position used for gynecological examination?
3. What tests are considered functional diagnostic tests?
4. What are endoscopic methods?
5. What are cytologic methods?
V. List of recommended literature
1. Danforth’s Obstetric and gynaecology.-Seventh edition.-1994.-P.691-708
2. Gynecology.-Stephan Khmil, Zina Kuchma, Lesya Romanchuk.-2003.P.13-25
3. Gynaecology illustrated. David McKay Hart, Jane Norman.-Fifth Edition.2000.-P.72-85
Approved on Session of Department of Obstetrics and Gynecology with course
of Infant and Adolescent Gynecology_________________ protocol No________
T.a.The Head of Department:_______________ O.A.Andriiets’