* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download This is the seventh of the monthly Drug and Alcohol Supplements
Survey
Document related concepts
Pharmaceutical industry wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Pharmacognosy wikipedia , lookup
Drug interaction wikipedia , lookup
Adherence (medicine) wikipedia , lookup
Electronic prescribing wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Prescription costs wikipedia , lookup
Effects of long-term benzodiazepine use wikipedia , lookup
Neuropharmacology wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Dextropropoxyphene wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Theralizumab wikipedia , lookup
Transcript
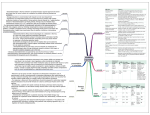
B4: 2 Benzodiazepines HO1 GP Drug & Alcohol Supplement No.9 February 1998 Benzodiazepine Dependence & Withdrawal Martin Evans & Trudy Waghorn Introduction Benzodiazepines (BZD) have become one of the most widely prescribed drugs for the management of anxiety and sleep disturbance. In recent years there has been a greater awareness that problems of abuse, dependence and associated withdrawal can occur with BZD, even when they are used in recommended therapeutic doses1. General Practitioners play an important role in helping patients to withdraw from BZD and in the prevention of dependence. Prevalence BZD are the most widely used psychotropic drugs in medical practice and accounted for 7.1 million prescriptions (private and NHS) in 19951. 20% of patients who are prescribed BZD take them for longer than 4 months1. Although still widespread, there has been a general decrease in the number of prescriptions for BZD since 1990. The most commonly prescribed BZD in Australia are diazepam, oxazepam, nitrazepam and temazepam, and account for 82% of all BZD use. BZD are used as sleeping pills twice as frequently as they are used as tranquillisers2. Who uses benzodiazepines Women are twice as likely as men to report BZD use, but men who take BZD are just as likely to take them long-term2. Use of BZD increases sharply with age. Nearly one in four people 75 years of age and over report using BZD2. 45% of all BZD prescriptions are written for people over 65 years of age3. 50-70% of patients in nursing homes are prescribed BZD over a long period of time3. Injection of BZD is a common practice among opiate users. In a recent study4 of 312 injecting drug users, 28% had injected BZD at some time and 13% had injected BZD in the last six months. The most commonly injected BZD are temazepam, diazepam and flunitrazepam. BZD are often used by patients who are alcohol-dependent to self-medicate the effects of hangover or withdrawal symptoms. Pharmacology BZD exert their pharmacological effects indirectly by occupying specific receptors in the brain; these receptors are in very close proximity to receptors for the inhibitory neurotransmitter gamma amino butryric acid (GABA). The effect of binding BZD to its receptor facilitates the effects of GABA. (GABA exerts an inhibitory effect on neuro-transmission by promoting the uptake of chloride ions across nerve membranes via chloride channels.) BZD exhibit sedative-hypnotic, anxiolytic, skeletal muscle relaxant, and anti-convulsant properties. BZD decrease the time to sleep onset, the time spent in deep slow wave sleep and awakenings, and increase total sleep time. Differences among members of the benzodiazepine class are seen in the time course of drug action, which is largely determined by the lipid solubility of an individual BZD, and the clearance of the drug and its active metabolites. Lipid solubility may override the effects of a long half-life. A highly lipid-soluble BZD such as diazepam will have a rapid hypnotic and anxiolytic action because of rapid absorption and uptake into the central nervous system. However, the effect is likely to wear off quickly because of extensive distribution into adipose tissue. Therefore, despite the long half-life of diazepam and its active metabolites, a t.d.s. dose is often used for effective anxiolytic therapy. Central Coast Area Health Service GP Drug & Alcohol Supplement No. 9 Slow elimination of a BZD which exhibits significant retention in the central nervous system is more likely to be associated with residual sedation the day after a dose, the so-called ‘hangover’ effect. BZD such as temazepam, alprazolam and lorazepam have relatively short half-lives and would be expected to be associated with less hangover effect following a hypnotic dose. However, short half-life BZD may be associated with more acute and intense withdrawal reactions upon cessation because of the relatively rapid decline in central nervous system concentrations5. Problems associated with BZD use withdrawal syndrome: psychological and somatic symptoms, perceptual disturbances, neurological complications tolerance: gradual loss of effectiveness and consequent dose increase side effects: drowsiness, lethargy, dizziness, headache, gastrointestinal problems, incoordination, ataxia, dysarthria, diplopia and paradoxical reactions, e.g. stimulation and anger cognitive impairment: subtle psychomotor deficits, memory and concentration difficulties, mental confusion, pseudo-dementia increased accident risk: falls and hip fractures in the elderly, machine operation and motor vehicle accidents adverse mood effects: depression, emotional anaesthesia adverse effects on sleep patterns: disturbed and broken sleep, nightmares, exacerbated hypoxia in respiratory patients, rebound insomnia in withdrawal risks to the developing embryo, foetus and new-born: possibility of withdrawal symptoms at birth, and transfer of the drug during breastfeeding causing drowsiness and feeding problems potential for overdose: most common drugs in Australian hospital self-poisoning patients6; particularly dangerous when taken in combination with alcohol or opiates adverse interactions with alcohol and other CNS depressants: increased problems with psychomotor and cognitive performance potential for abuse: February 1998 BZD use among intravenous drug users and alcohol users is common and is associated with higher rates of HIV risktaking behaviour and psychopathology, poorer health, poorer social functioning, and greater risk of heroin overdose. Injection of BZD has also been associated with vascular morbidity and mortality. Assessment steps7 1. Advise the patient that you wish to review their benzodiazepine medication with them. 2. Assess past history of BZD use and initial reasons for use. 3. Assess dosage and pattern of use. 4. Assess use of alcohol and other psychotropic drugs. 5. Assess current and past history of withdrawal symptoms. 6. Assess side-effects reported and observed. 7. Assess history of depression. 8. Assess other medical problems. 9. Discuss the risks of long-term use with the patient. Benzodiazepine tolerance & withdrawal Tolerance and withdrawal from BZD can occur in people who have been taking therapeutic or higher doses of BZD on a regular basis for a duration of two or more weeks. It is estimated that tolerance and withdrawal symptoms are experienced in up to 45% of patients discontinuing low therapeutic doses of BZD, and up to 100% of patients for high doses. There is a significant risk of withdrawal if BZD are discontinued abruptly, particularly in the sick and the elderly. Onset and duration of withdrawal Withdrawal from short-acting BZD generally occurs earlier than withdrawal from long-acting BZD. Withdrawal symptoms commence within 12 days after reduction in dose of a short-acting BZD, and between 1-5 days for a long-acting BZD. The duration of withdrawal is highly variable. Withdrawal symptoms may persist for 6-8 weeks after cessation of BZD with a peak in intensity in the second and third weeks. A minority of patients may experience low grade symptoms intermittently for up to six months. Symptoms of withdrawal There is a wide range of symptoms that may be experienced in BZD withdrawal and a considerable variation between individuals. The BZD withdrawal syndrome is usually characterised by some of the signs and symptoms outlined in the following table: Central Coast Area Health Service GP Drug & Alcohol Supplement No. 9 Table 1. Symptoms of BZD Withdrawal February 1998 have been using very high doses for a significant duration (>dose equivalent of 80 mg diazepam) are dependent on other drugs, particularly alcohol and opiates have a concurrent psychiatric or serious medical illness. Most Common BZD Withdrawal Symptoms Medically Serious BZD Withdrawal Symptoms Other Symptoms Experienced in BZD Withdrawal insomnia seizures muscle twitching anxiety delirium muscle pains Pharmacotherapy irritability anorexia restlessness metallic taste The following are principles of pharmacological therapy in the home setting: agitation fatigue depression tinnitus tremor hyperacusis dizziness photophobia headache perceptual disturbances derealisation depersonalisation blurred vision nausea Major manifestations such as seizures and delirium are rare. However, seizures may occur from 1-12 days after discontinuing BZD and are usually associated with high doses and abrupt cessation. Delirium may occur in the absence of signs of autonomic hyperactivity or withdrawal. estimate the average daily intake of BZD calculate an equivalent dose of diazepam (Table 2) and substitute diazepam (it has a long half-life) for the BZD. In some cases it is impossible to ascertain the average daily intake of BZD. The substitute equivalent dose of diazepam can then be established by administering incremental doses of diazepam to a point where withdrawal symptoms are relieved but the patient is not oversedated. This initial dose is then maintained for a few days; after that a slow tapering of diazepam is commenced Table 2. BZD Dose Equivalents8 Usual daily oral dose range, dose equivalents and pharmacokinetic properties of anxiolytics and hypnotics Drug Usual daily & dose range (mg) Approximate equivalent dose* (mg) to diazepam 5mg alprazolam 1-4 0.5-1 Elimination half-lives of drug and active metabolites ~ + (hours) 14 bromazepam 6-9 3-6 16 30-80 10 18, 40 clonazepam 4-8 0.5 35 diazepam 5-20 5 30, 75 flunitrazepa m 0.5-2 1-2 23, 25, 31 lorazepam 2-4 1# 12 nitrazepam 5-20 5-10 25 oxazepam 45-90 15-30 10 temazepam 10-30 10-20 15 0.125-0.25 0.25 3 buspirone 15-30 - 3 zopiclone 3.75-7.5 - 5 Treatment of benzodiazepine withdrawal Outpatient/home detoxification Most patients experiencing uncomplicated withdrawal can be effectively managed by their GP in an outpatient setting. Criteria for home detoxification are as follows: a patient currently using BZD who wishes to or agrees to withdraw from them patient is expected to experience only a mild to moderate withdrawal a GP is available to provide regular monitoring of the patient’s progress home supervision (e.g. a reliable relative or friend) should be available for patients withdrawing from high doses (>dose equivalent of 60 mg diazepam). Inpatient detoxification Admission for detoxification is required for a minority of patients who: have been repeatedly unsuccessful in previous attempts at outpatient detoxification present already exhibiting severe symptoms of withdrawal or have a history of major withdrawal complications clobazam triazolam Others * the widely varying half-lives and receptor binding characteristics of these agents make exact dose equivalents difficult to establish ~ the stated half-lives are generally in the middle of the range of reported values; there is considerable individual variation Central Coast Area Health Service GP Drug & Alcohol Supplement No. 9 + where clinically significant # lorazepam may be relatively more potent at higher doses Therapeutic Guidelines: Psychotropic Version 4, 2000 give diazepam in 3-4 divided doses per day at fixed times reduce dose by between 10-20% at weekly intervals. Reduction may need to be slower when the dose is down to 15 mg daily regularly review and titrate dose to the severity of withdrawal symptoms. In general practice a reducing regime will generally take 6-8 weeks, but may take 3-4 months or even a year sometimes, even when the dose is reduced by only a small amount, withdrawal symptoms re-emerge. In this case, the dose may be held at a plateau for 1-2 weeks or even increased for a few days before the reduction regime is resumed. Supportive Care Frequent monitoring, reassurance, provision of information and a suitable environment are important to reduce the severity of withdrawal symptoms. Advice and written information should be provided about: management of acute stress-related anxiety management of insomnia structured problem solving diet dealing with cravings relapse prevention. Special cases The reluctant patient A number of patients who have been taking BZD for long periods of time may be reluctant to consider coming off their drugs or even resistant to the idea. This poses a problem for the GP. Explanation of the drug’s effects and limitations and encouragement of the patient’s ability to cope without them will often be sufficient to enable the patient to give it a try. Extra resources may be useful, e.g. counselling, stress management. The patient should not feel pressured but rather supported and encouraged9. February 1998 Almost all GPs come across habitual drug users or patients who are obtaining prescriptions from several doctors (‘doctor shopping’). The following points may assist in dealing more effectively with these patients1: do not prescribe BZD on the first visit there is rarely a valid indication for BZD in young people say “no” from the start to the patient’s requests for BZD, whilst offering your help as a doctor take the opportunity to discuss risks associated with drug use, and refer to a specialist agency. Prevention of dependence - guidelines for prescribing benzodiazepines Problems of dependence will be minimised if the following guidelines are followed5: where possible use non-pharmacological alternatives to BZD (e.g. counselling, relaxation techniques) use BZD only for appropriate indications warn of possibility of dependency when use of BZD is prolonged BZD are contraindicated in patients known to be substance abusers in chronic conditions, intermittent brief use of BZD may be appropriate explain the use of the medication and the context of its use use the lowest dose of BZD necessary review regularly assess BZD efficacy at one week limit prescription of BZD to 2 weeks discontinue gradually if the patient has been taking BZD for a prolonged period. General Practitioners who require further information or assistance regarding patients who are using or wish to withdraw from benzodiazepines can contact the GP Drug & Alcohol Local Consultancy Service on 0413 276 177 The habitual drug user (‘Doctor shopping’) References: 1. Mant, A., de Burgh, S., Yeo, G., Letton, T. & Shaw, J. (1997) Anxiety & insomnia - think twice before prescribing. The Royal Australian College of General Practitioners. 2. Benzodiazepines: some prescription guidelines (1994) Connexions 14(1): 17. 3. Tranx National Conference on Benzodiazepine Use Proceedings, Melbourne (1991). 4. Ross, J., Darke, S. & Hall, W. (1997) Benzodiazepine injecting among heroin users: why they do it, how they do it and the associated factors. Tenth NDARC Annual Symposium. 5. Mant, A., Wodak, A. & Day, R. (1987) Benzodiazepine dependence: strategies for prevention and withdrawal. Current Therapeutics February: 59-79. 6. National Drug Abuse Data System (1988). 7. Mant, A. & Walsh, R. (1997) Reducing benzodiazepine use. Drug and Alcohol Review 16: 77-84. 8. Goodman, A. & Gilman, L. (1991) The Pharmacological Basis of Therapeutics. Macmillan, New York. p. 357. 9. Benzodiazepine reduction guidelines for doctors (1990) Tranx Inc. Central Coast Area Health Service