Changes to the Diagnosis of Childhood Disorders
... the same diagnosis, so it is unlikely that a set of intervention strategies will apply to all students Some strategies that are helpful for all students include: small groups, one to one teaching, minimise distractors such as noises, have clear and concise expectations, give advanced warning for c ...
... the same diagnosis, so it is unlikely that a set of intervention strategies will apply to all students Some strategies that are helpful for all students include: small groups, one to one teaching, minimise distractors such as noises, have clear and concise expectations, give advanced warning for c ...
Chapter 12: Social Psychology
... Mood Disorders A category of mental disorders in which significant and chronic disruption in mood is the predominant symptom, causing impaired cognitive, behavioral, and physical functioning – Major depression – Dysthymic disorder – Bipolar disorder – Cyclothymic disorder ...
... Mood Disorders A category of mental disorders in which significant and chronic disruption in mood is the predominant symptom, causing impaired cognitive, behavioral, and physical functioning – Major depression – Dysthymic disorder – Bipolar disorder – Cyclothymic disorder ...
SCHIZOPRENIA
... causes strange thinking, abnormal feelings, and unusual behavior. It is uncommon in children and hard to recognize in its early stages. Adult behavior often differs from that of teens and children. ...
... causes strange thinking, abnormal feelings, and unusual behavior. It is uncommon in children and hard to recognize in its early stages. Adult behavior often differs from that of teens and children. ...
ISSUES SURROUNDING CLASSIFICATION AND DIAGNOSIS OF
... Non-endogenous (or reactive) depression – arises from environmental stressors endogenous depression has more severe symptoms and greater suicide rates. This one responds more positively to ECT and antidepressant medications. Little conclusive evidence to support the distinction. ...
... Non-endogenous (or reactive) depression – arises from environmental stressors endogenous depression has more severe symptoms and greater suicide rates. This one responds more positively to ECT and antidepressant medications. Little conclusive evidence to support the distinction. ...
Ready for Review - Paramedic EMS Zone
... pyromania. They reflect the inability to resist temptation. ...
... pyromania. They reflect the inability to resist temptation. ...
Bipolar Disorder (manic–depressive Illness)
... Hypomania is a milder form of mania with similar yet less severe symptoms and less overall impairment. In hypomania, for example, the individual may have an elevated mood, feel better than usual, and be more productive. These episodes often feel good, and the quest for hypomania may even cause peopl ...
... Hypomania is a milder form of mania with similar yet less severe symptoms and less overall impairment. In hypomania, for example, the individual may have an elevated mood, feel better than usual, and be more productive. These episodes often feel good, and the quest for hypomania may even cause peopl ...
ppt
... DSM-V Depressive Disorders • Disruptive mood dysregulation disorder • Major Depressive disorder • Persistent depressive disorder ...
... DSM-V Depressive Disorders • Disruptive mood dysregulation disorder • Major Depressive disorder • Persistent depressive disorder ...
Abnormal Psychology - Bloomfield Central School
... Catatonic Schizophrenia • Flat effect • Waxy Flexibility • parrot like repeating of another’s speech and movements ...
... Catatonic Schizophrenia • Flat effect • Waxy Flexibility • parrot like repeating of another’s speech and movements ...
Chapter 8: Dissociative Disorders and Somatic-Symptom
... Somatic Symptom Disorder Dissociative Identity Disorder • Criteria Clarified • A. Disruption of identity characterized by two or more distinct personality states (alters) or an experience of possession, as evidenced by discontinuities in sense of self as reflected in altered cognition, behavior, af ...
... Somatic Symptom Disorder Dissociative Identity Disorder • Criteria Clarified • A. Disruption of identity characterized by two or more distinct personality states (alters) or an experience of possession, as evidenced by discontinuities in sense of self as reflected in altered cognition, behavior, af ...
DSM-IV AND IDEA - Seattle University School of Law
... determination of emotional disorder • Expert testimony may reference and discuss ...
... determination of emotional disorder • Expert testimony may reference and discuss ...
Specify dissociative fugue subtype if the amnesia is
... • Specify dissociative fugue subtype if the amnesia is associated with bewildered or apparently purposeful wandering ...
... • Specify dissociative fugue subtype if the amnesia is associated with bewildered or apparently purposeful wandering ...
The sections in the book that correspond to this quiz are modules 29
... 19. A person who is convinced that she has more than one personality and “blacks out” for hours while another personality takes over is likely to be diagnosed with which of the following? A) dissociative identity disorder B) dissociative schizophrenia C) dissociative amnesia D) dissociative fugue 20 ...
... 19. A person who is convinced that she has more than one personality and “blacks out” for hours while another personality takes over is likely to be diagnosed with which of the following? A) dissociative identity disorder B) dissociative schizophrenia C) dissociative amnesia D) dissociative fugue 20 ...
PDF - Bio-Balance Health Australia
... cent of us will suffer from depression during our lives: that’s more than four million Australians struggling daily with symptoms including insomnia, feelings of hopelessness and despair and a loss of pleasure and interest in normal activities. Around 1.3 million people will experience a major depre ...
... cent of us will suffer from depression during our lives: that’s more than four million Australians struggling daily with symptoms including insomnia, feelings of hopelessness and despair and a loss of pleasure and interest in normal activities. Around 1.3 million people will experience a major depre ...
Psychotic and somatoform disorders
... List and described the different psychotic disorders and how to differentiate between them List the most commonly used antipsychotic medications and describe the general characteristics of each Describe the ongoing health monitoring parameters associated with using these medications ...
... List and described the different psychotic disorders and how to differentiate between them List the most commonly used antipsychotic medications and describe the general characteristics of each Describe the ongoing health monitoring parameters associated with using these medications ...
Diapositiva 1 - WordPress.com
... Mood Disorders (DSM-IV) • Depressive Disorders -Major Depressive Disorder -Dysthymic Disorder -Depressive Disorder, Not otherwise specified ...
... Mood Disorders (DSM-IV) • Depressive Disorders -Major Depressive Disorder -Dysthymic Disorder -Depressive Disorder, Not otherwise specified ...
Depressed or Demoralized?
... In contrast, “demoralization” is generally defined as “persistent inability to cope, … [and] associated feelings of helplessness, hopelessness, … subjective incompetence, and diminished self-esteem”, which also involves a challenge to one’s sense of meaning or purpose, but is not more than would be ...
... In contrast, “demoralization” is generally defined as “persistent inability to cope, … [and] associated feelings of helplessness, hopelessness, … subjective incompetence, and diminished self-esteem”, which also involves a challenge to one’s sense of meaning or purpose, but is not more than would be ...
Introduction to Psychology
... Loss of appetite and/or weight loss, or conversely overeating and weight gain Insomnia, early-morning awakening, or oversleeping Restlessness or irritability Feelings of worthlessness, inappropriate guilt, ...
... Loss of appetite and/or weight loss, or conversely overeating and weight gain Insomnia, early-morning awakening, or oversleeping Restlessness or irritability Feelings of worthlessness, inappropriate guilt, ...
Somatoform, Factitious and Dissociative Disorders
... paralysis, localized weakness, visual changes ...
... paralysis, localized weakness, visual changes ...
The Somatic Symptom and Related Disorders
... • Ironically, they are very dissatisfied w/ care • So they seek new MDs, treatments, drugs • Some can’t work ...
... • Ironically, they are very dissatisfied w/ care • So they seek new MDs, treatments, drugs • Some can’t work ...
Schizophrenia - issues surrounding diagnosis L1
... Residual Type – 20% Absence of prominent delusions, hallucinations, disorganized speech, and grossly disorganized or catatonic behaviour. Plus presence of negative symptoms or two or more symptoms listed in Criterion A for Schizophrenia ...
... Residual Type – 20% Absence of prominent delusions, hallucinations, disorganized speech, and grossly disorganized or catatonic behaviour. Plus presence of negative symptoms or two or more symptoms listed in Criterion A for Schizophrenia ...
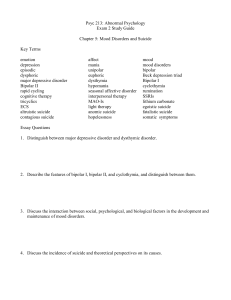
Psyc 213: Abnormal Psychology
... 4. Discuss the connection between psychological trauma and fugue, amnesia, and dissociative identity disorder. ...
... 4. Discuss the connection between psychological trauma and fugue, amnesia, and dissociative identity disorder. ...
What is bipolar disorder - Centre for Clinical Interventions
... form of elevated mood. It can be managed often without the need for hospitalisation as the person remains in contact with reality. However, it is very easy to move rapidly from hypomania into a manic episode. Symptoms of mania include: Irritability: Irritability as described in the Oxford dictionary ...
... form of elevated mood. It can be managed often without the need for hospitalisation as the person remains in contact with reality. However, it is very easy to move rapidly from hypomania into a manic episode. Symptoms of mania include: Irritability: Irritability as described in the Oxford dictionary ...
Schizoaffective disorder

Schizoaffective disorder (abbreviated as SZA or SAD) is a mental disorder characterized by abnormal thought processes and deregulated emotions. The diagnosis is made when the patient has features of both schizophrenia and a mood disorder—either bipolar disorder or depression—but does not strictly meet diagnostic criteria for either alone. The bipolar type is distinguished by symptoms of mania, hypomania, or mixed episode; the depressive type by symptoms of depression only. Common symptoms of the disorder include hallucinations, paranoid delusions, and disorganized speech and thinking. The onset of symptoms usually begins in young adulthood, currently with an uncertain lifetime prevalence because the disorder was redefined, but DSM-IV prevalence estimates were less than 1 percent of the population, in the range of 0.5 to 0.8 percent. Diagnosis is based on observed behavior and the patient's reported experiences.Genetics, neurobiology, early and current environment, behavioral, social, and experiential components appear to be important contributory factors; some recreational and prescription drugs may cause or worsen symptoms. No single isolated organic cause has been found, but extensive evidence exists for abnormalities in the metabolism of tetrahydrobiopterin (BH4), dopamine, and glutamic acid in people with schizophrenia, psychotic mood disorders, and schizoaffective disorder. People with schizoaffective disorder are likely to have co-occurring conditions, including anxiety disorders and substance use disorder. Social problems such as long-term unemployment, poverty and homelessness are common. The average life expectancy of people with the disorder is shorter than those without it, due to increased physical health problems from an absence of health promoting behaviors including a sedentary lifestyle, and a higher suicide rate.The mainstay of current treatment is antipsychotic medication combined with mood stabilizer medication or antidepressant medication, or both. There is growing concern by some researchers that antidepressants may increase psychosis, mania, and long-term mood episode cycling in the disorder. When there is risk to self or others, usually early in treatment, brief hospitalization may be necessary. Psychiatric rehabilitation, psychotherapy, and vocational rehabilitation are very important for recovery of higher psychosocial function. As a group, people with schizoaffective disorder diagnosed using DSM-IV and ICD-10 criteria have a better outcome than people with schizophrenia, but have variable individual psychosocial functional outcomes compared to people with mood disorders, from worse to the same. Outcomes for people with DSM-5 diagnosed schizoaffective disorder depend on data from prospective cohort studies, which haven't been completed yet.In DSM-5 and ICD-9 (which is being revised to ICD-10, to be published in 2015), schizoaffective disorder is in the same diagnostic class as schizophrenia, but not in the same class as mood disorders. The diagnosis was introduced in 1933, and its definition was slightly changed in the DSM-5, published in May 2013, because the DSM-IV schizoaffective disorder definition leads to excessive misdiagnosis. The changes made to the schizoaffective disorder definition were intended to make the DSM-5 diagnosis more consistent (or reliable), and to substantially reduce the use of the diagnosis. Additionally, the DSM-5 schizoaffective disorder diagnosis can no longer be used for first episode psychosis.