* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Herpes simplex virus 1
Trichinosis wikipedia , lookup
Sarcocystis wikipedia , lookup
Human papillomavirus infection wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Ebola virus disease wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Hepatitis C wikipedia , lookup
West Nile fever wikipedia , lookup
Neonatal infection wikipedia , lookup
Influenza A virus wikipedia , lookup
Orthohantavirus wikipedia , lookup
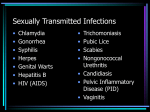
Sexually transmitted infection wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Marburg virus disease wikipedia , lookup
Herpes simplex wikipedia , lookup
Herpes simplex research wikipedia , lookup
Henipavirus wikipedia , lookup
Lymphocytic choriomeningitis wikipedia , lookup
Sidra Saeed FA08-BBS-015 • • • • • • • • • • Symptoms Classification Diagnosis Discovery of HSV Treatment Types of HSV Viral Structure Complications Hosts of HSV Mode of Replication Virus Latency Modes of Transmission Immune Response against HSV Group: (dsDNA) Family: Herpesviridae Subfamily: Alphaherpesvirinae Genus: Simplexvirus Species: Herpes simplex virus 1 (HSV-1) • HSV is an ancient disease with descriptions of orolabial herpes appearing in records from the fifth century BCE. • In the 1736 Astruc (physician to King of France) identified Herpes as a cause of genital infection. • Over the next 50 years many different strains of herpes were discovered. • In 1893 intimate human-to-human transmission was identified. • Finally neonatal HSV infection was identified in • The Type 1 virus causes cold sores. Most people get Type 1 infections during infancy or childhood. • The Type 2 virus causes genital sores. Most people get Type 2 infections following sexual contact with an infected person. Both types can be differentiated by biologic, biochemical and antigenic properties • Composed of a dsDNA (152kbp) nucleoprotein core • Core is surrounded by an icosahedral protein capsid • 100nm capsid is enclosed in an outer envelope consisting of at least 8 glycoproteins. • The tegument is present between the capsid and the envelope • Envelope spikes ~8 nm long • The virus requires a moist environment for survival. Meningitis: infection of the sheaths and membranes (meninges) covering the brain and the spinal cord. Encephalitis: acute inflammation of the brain, commonly caused by a viral infection by insect bites or food and drink Eczema herpetiform: widespread herpes across the skin) Keratoconjunctivitis: Infection of the eye Prolonged, severe infection in immunosuppressed individuals Pneumonia Infection of the trachea • Humans • Simians • Cattle • Cats • Chickens Of these, only herpes virus simiae is harmful to us. • The viral envelop becomes incorporated in the host’s membrane The nucleocapsid uncoats and releases the DNA into the nucleus. • In the nucleus the DNA circularizes, and the host’s enzymes begin to transcribe the first set of viral genes, known as early genes • The early mRNA molecules enter the cytoplasm, where they are translated into the early proteins. • The early proteins, in turn, enter the nucleus for viral DNA replication • At this point, the cell begins to transcribe late mRNA molecules • These mRNAs enter the cytoplasm for the translation of late proteins • The late proteins include the capsid structural proteins, which enter the nucleus • The late proteins also include envelop proteins, which are produced in ER. • These envelop proteins become incorporated in the nuclear membrane • The viral DNA continues to replicate. • During this later stage of replication concatemers of viral DNA form. • These copies are cut into individual genomes as they are packaged into capsids • At the nuclear membrane, capsid and the DNA bud off and become surrounded by membrane material with embedded membrane proteins • The virus passes through the ER and buds off this membrane before migrating to the plasma membrane • The virus fuses with the plasma membrane and is released from the cell. HSV is transmitted through the body on nerves or synapses to and from mucosal tissues Vaccines and antiviral medicines can’t attack latent virus Once infected, a person is infected for life. Latency in mucosal surfaces is effective way to transmit because of common mucosal contact •Direct skin-to-skin contact with the infected areas • Sexual Intercourse • Oral Sex Even though most skin on our bodies is too thick for the virus to penetrate, it can penetrate areas with mucous membranes such as the genitals, the mouth, the esophagus, the trachea, and even onto broken areas of skin anywhere The constant battle between our body and invaders… Both the cellular and humoral arms of the immune response are involved Interferon and natural killer cells are important in limiting the initial infection . Cytotoxic T cells and macrophages kill infected cells The humoral response (antibodies against surface glycoproteins) leads to neutralization. The virus can escape the immune system by coating itself with IgG via Fc receptors The virus can also spread from one cell to another without entering the extracellular space and coming in contact with humoral antibodies Cell-mediated responses are vital in controlling herpes infections. Mouth sores Genital lesions Blisters and/or ulcers Fever Enlargement of lymph nodes • The appearance of HSV is often so typical. • The genital herpes sores may not be visible to the naked eye • A viral PCR can be run on a swab of infected tissue. • A blood test, can show if a person has been infected with HSV but cannot distinguish between type I and II. • There is no vaccine that prevents this disease from occurring. • Oral anti-viral medications such as • acyclovir (Zovirax), • famciclovir (Famvir), • or valacyclovir (Valtrex) have been developed to effectively treat herpes infections. • To keep from spreading the infection: Keep the infected area clean and dry to prevent other infections from developing. Try and avoid touching the sores. Wash your hands after contact with the sores. Avoid sexual contact from the time you first feel any symptoms until the sores are completely healed. HUMAN PAPILLOMA VIRUS DISCOVERY • • • • Discovered by Dr Harald Zur Hausen in 1984 in German Cancer Research Centre. Was found in the tumorous cells associated with cervical cancer patients. A group of viruses containing almost 150 different types of viruses. Double stranded DNA viruses. • • BACKGROUN D Papilloma viruses are known to infect almost all mammallian and avian species having 100 types infecting humans Specific types infect human skin and mucosal epithelium to cause papillomas or warts • • Mucosal types of infection is found in persons having sexual contact with HPV infected women and homosexual males Most of the infection caused by this are mostly cleared by the immune system before showing any symptoms • • • More than 5% of cancers worldwide are caused by infection from this virus The most common sexually transmitted virus afflicting 50-80% population Of the 100 known types; 40 infect the genital tracts • • • REPLICATION HPV infection is limited to the basal cells associated with stratified epithelium These are the only tissues in which they can replicate In case of any abrasion to epithelium it comes in contact with the basement membrane cells • • • Its infection process is slow taking 12-24 hours of transcription initiation HPV virus does not show cytolytic activity Rather the virus particles are released in the form of degeneration of desquamating cells • This virus can survive for many months without a host at low temperatures , so it can be spread if an infected person walks bare-foot • VIRAL REPLICATION HPV has 6 early proteins(E1,E2,E3,E4,E5,E6) and 2 late proteins (L1,L2) • Before integrating in host genome High levels of E1 & E2 E2 repress E6/E7 expression • After integrating in host E2 function disrupted Prevents repression of E6/E7 • • • ONCOGENES Role of E6 & E7 proteins in cancer E6 inactivates p53 TSP whereas E7 inactivates pRb TSP These proteins modify the host cell cycle – – to keep differentiating the keratinocytes helps in the amplification of viral genome replication • ROLE of E6 Protein E6 forms association with E6 associated protein of host – – Ubiquitinate the p53 protein cause proteosomal degradation of p53 • ROLE OF E7 PROTEIN E7 acts as primary transforming protein – Competes for retinoloblastoma protein binding – Freeing the transcription factor E2f to transactivate its target pushing cell cycle forward • • LATE PROTEINS L1&L2 These are structural proteins that encapsidate the viral genome Once the genome is encapsidated it undergoes the assembly/maturation event • • • Stabilizes the virions Increases viral specific infectivity Virions can then be sloughed off as squames from host epithelium and viral life cycle continues • TRANSMISSIO N Prenatal – Genital HPV are usually transmitted from mother to newborn Perinatal Perinatal transmision of HPV type 6 and 11 causes onset of juvenile-onset recurrent respiratory papilllomatosis(JORRP) • Genital transmission is from infected partner during sexual contact it can not be prevented even using condoms because some of the infected region is SYMPTOMS • COMMON WARTS rough, raised bumps that usually occur on the hands, fingers or around fingernails. • Plantar Warts hard, grainy growths that usually appear on the heel or ball of your feet, areas that feel the most pressure. These warts may cause discomfort or pain • FLAT WARTS Flat-topped, slightly raised lesions darker than your regular skin color. They usually appear on your face, neck, hands, wrists, elbows or knees. • GENITAL WARTS Flat lesions, small cauliflower-like bumps or tiny stem-like protrusions. VACCINES FOR HPV • Gradasil Work against HPV 16&18 which cause 70% of cervical cancer HPV 6&11 which cause 90% of genital warts Work against HPV • CERVARIX 16&18 which cause 70% of cervical cancer • • ScienceDaily (Oct. 6, 2008); http://www.sciencedail y.com/releases/2008/1 0/081006093031.htm Ganguly, N.; Parihar, S. P. (2009). "Human papillomavirus E6 and E7 oncoproteins as risk factors for tumorigenesis".