* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download What is your diagnosis?
Survey
Document related concepts
Fundus photography wikipedia , lookup
Contact lens wikipedia , lookup
Keratoconus wikipedia , lookup
Idiopathic intracranial hypertension wikipedia , lookup
Vision therapy wikipedia , lookup
Mitochondrial optic neuropathies wikipedia , lookup
Visual impairment wikipedia , lookup
Macular degeneration wikipedia , lookup
Blast-related ocular trauma wikipedia , lookup
Retinitis pigmentosa wikipedia , lookup
Visual impairment due to intracranial pressure wikipedia , lookup
Eyeglass prescription wikipedia , lookup
Transcript
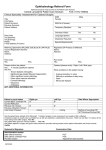
Mansukhani, Sujata To Marcial, Karmi Margarette This 30 year old male sought consult because of blurring of vision of the left eye. Visual acuity was light perception on the involved eye. This condition has been present since childhood. Outline What is your diagnosis? What diagnostic test would you do to help you decide on your management? What is your treatment plan? What will be the visual outcome of this patient after your surgical management? Question # 1 SALIENT FEATURES Patient presented with: LEUKOCORIA UNILATERAL, PAINLESS BLURRING OF VISION Condition is congenital or “present since birth” Patient Unilateral Gradual, Painless Blurring of Vision present since birth Light perception on affected eye Leukocoria Retinopathy of prematurity Retinal Detachment Coloboma occurs in premature, lowbirth-weight infants maintained on oxygen therapy risk factors: trauma and surgery, vitreous detachment, high myopia, retinal breaks or tears, retinal vascular disease, and history of detachment in the other eye flashes of light, floaters, curtainlike decrease in vision Congenital caused by incomplete closure of the fetal fissure Degree of visual loss related to area affected (iris, retina, choroid, or optic nerve head) Cataract May be: age-related childhood cataract (congenital or acquired) traumatic druginduced Unilateral or bilateral Painless leukocoria Glare or star bursts Question # 2 History and PE thorough history careful physical examination must be performed entire body habitus is checked for abnormalities that may point out systemic illnesses Ocular Examination Visual acuity for both near and far distances (Snellen’s Chart) Glare- brightly lit room Swinging Flashlight Test detects for a Marcus Gunn pupil or a relative afferent pupillary defect (RAPD) indicative of optic nerve lesions or diffuse macular involvement. RAPD + Cataract= very guarded visual prognosis after cataract extraction Ocular Motility long-standing ptosis since childhood may have occlusion amblyopia decreased visual acuity rather than the cataract Checking all directions- to rule out any other causes for the patient's visual symptoms Slit Lamp Examination should not only concentrate on evaluating the lens opacity but the other ocular structures as well (eg, conjunctiva, cornea, iris, anterior chamber) Corneal thickness and the presence of corneal opacities lens noted meticulously before and after pupillary dilation Nuclear size and Brunescence as indicators of cataract density can be determined prior to phacoemulsification surgery. lens position and integrity of the zonular fibers also should be checked lens subluxation may indicate previous eye trauma, metabolic disorders, or hypermature cataracts. Dilated fundus examination is recommended as part of the ocular examination for both unilateral cataract cases and bilateral cataract cases. Question # 3 Early cataracts may be managed with the following measures: Stronger eyeglasses or contact lenses Use of a magnifying glass during reading Strong lighting Medication that dilates the pupil. (This may help some people with capsular cataracts, although glare can be a problem with this treatment.) Indications for Surgery The Snellen eye test reports 20/40 or worse, with a cataract being responsible for vision loss that cannot be corrected by glasses. Performing everyday activities has become difficult to perform to the point that independence is threatened, or the patient is at risk for accident or injury. Three basic types of surgery Extracapsular cataract extraction Intracapsular cataract extraction Phacoemulsification Surgery to remove cataracts is generally an outpatient procedure. A local anesthetic is used and the procedure lasts about an hour. Question # 4 A comprehensive study reported in Archives of Ophthalmology (1994) 95.5 percent of healthy eyes achieved 20/40 uncorrected vision or better outcomes following cataract surgery Of the more than 17,000 eyes evaluated, fewer than 2 percent had sight-threatening complications. Sight-threatening complications • associated with individuals • Glaucoma who are much older or who already have poor underlying health affecting how their eyes heal. • cataracts are far more advanced or "hardened" at the time of surgery, making them difficult to remove • Retinal detachment • Endophthalmitis • Secondary cataract A Swedish study published in the British Journal of Ophthalmology (1999) Younger people undergoing cataract surgery reported the highest satisfaction levels. Less satisfactory outcome when other eye problems were present British Journal of Ophthalmology (2000) people in their 6Os undergoing cataract surgery were 4.6 percent more likely to achieve 20/40 uncorrected vision or better than people in their 80s