* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download (MMR) genes - Biochemical Society Transactions
Koinophilia wikipedia , lookup
History of genetic engineering wikipedia , lookup
Non-coding DNA wikipedia , lookup
Therapeutic gene modulation wikipedia , lookup
Epigenetics of neurodegenerative diseases wikipedia , lookup
Dominance (genetics) wikipedia , lookup
Artificial gene synthesis wikipedia , lookup
Neuronal ceroid lipofuscinosis wikipedia , lookup
Saethre–Chotzen syndrome wikipedia , lookup
Nutriepigenomics wikipedia , lookup
Designer baby wikipedia , lookup
Mir-92 microRNA precursor family wikipedia , lookup
Site-specific recombinase technology wikipedia , lookup
Genome evolution wikipedia , lookup
No-SCAR (Scarless Cas9 Assisted Recombineering) Genome Editing wikipedia , lookup
Genome editing wikipedia , lookup
BRCA mutation wikipedia , lookup
Genome (book) wikipedia , lookup
Cancer epigenetics wikipedia , lookup
Microevolution wikipedia , lookup
Frameshift mutation wikipedia , lookup
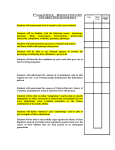
718 Biochemical Society Transactions (2005) Volume 33, part 4 Phenotype associated with recessively inherited mutations in DNA mismatch repair (MMR) genes M. de Vos*, B. Hayward*, D.T. Bonthron* and E. Sheridan†1 *Department of Molecular Medicine, University of Leeds, Leeds LS2 9JT, U.K., and †Department of Clinical Genetics, St James’s University Hospital, Leeds LS9 7TF, U.K. Abstract The MMR (DNA mismatch repair) system helps to maintain the integrity of the genome. This involves eliminating base–base mismatches and insertion/deletion loops, which can lead to microsatellite instability, as seen in tumour cells. Hereditary non-polyposis colon cancer is the result of dominant mutations in MMR genes, such as MLH1, MSH2 and MSH6. More recently there have been case reports of biallelic mutations in the MMR genes MLH1, MSH2 and PMS2. These result in a distinct autosomal recessive cancer predisposition syndrome. The syndrome is characterized by childhood haematological malignancies, brain tumours and the presence of café au lait patches. Second primaries occur frequently in this condition, and survival into adulthood is rare. The integrity of the genome is maintained by a variety of sophisticated mechanisms which repair damaged DNA. The MMR (mismatch repair) system is one of the best characterized of these. The primary function of the MMR system is to eliminate base–base mismatches and insertion/deletion loops, which arise during DNA replication [1]. Insertion/deletion loops classically result in the shortening or lengthening of repetitive sequences in microsatellites. This is termed MSI (microsatellite instability) and is seen in tumour cells, which harbour biallelic MMR mutations. MMR in humans depends on homologues of the bacterial MutS and MutL proteins, these function as heterodimers. The MutSα complex comprising a heterodimer of MSH2/MSH6 is the most abundant species, with lesser amounts of MSH2/ MSH3 (MutSβ) also being present. The MutS complex initiates DNA repair by mismatch recognition. Interaction between this recognition complex and downstream repair proteins is dependent upon MutL-like activity. An MLH1/PMS2 heterodimer (MutLα) is the major species providing MutLlike MMR activity in human cells [2]. Germline mutations in MLH1, MSH2 and MSH6 are the major cause of HNPCC (hereditary non-polyposis colon cancer), the commonest form of inherited colon cancer. HNPCC is a dominantly inherited disorder with a high penetrance. As well as CRC (colorectal cancer), HNPCC patients have an excess of extracolonic malignancies, principally endometrial and ovarian cancers in women, and, to a lesser extent, other cancers such as renal, small bowel and ureter [3]. Key words: hereditary non-polyposis colon cancer (HNPCC), mismatch repair gene (MMR gene), recessive inheritance, supratentorial primitive neuroectodermal tumour (SPNET). Abbreviations used: CAL, café au lait patch; CML, chronic myeloid leukaemia; CRC, colorectal cancer; HNPCC, hereditary non-polyposis colon cancer; MMR, mismatch repair; MSI, microsatellite instability; NF-1, neurofibromatosis type 1; SPNET, supratentorial primitive neuroectodermal tumour. To whom correspondence should be addressed (email [email protected]). 1 C 2005 Biochemical Society Recessive mutations in the PMS2 gene Although PMS2 was originally described as a cause of classical HNPCC [4], very few families with HNPCC due to PMS2 mutations have since been described. In fact the only clear association has been with Turcot’s syndrome. This is a variant of HNPCC characterized by the presence of CRC and brain tumours. We recently reported a consanguineous U.K. family of Pakistani origin, in which two siblings developed SPNET (supratentorial primitive neuroectodermal tumours) and a further sibling developed a T-cell lymphoma. All three also manifested CALs (café au lait patches). A homozygous mutation C2482T in exon 14 of PMS2 was found in all three affected individuals [5]. In a further case originally reported with dominantly inherited Turcot’s syndrome [6], we also identified a second mutation in exon 13 (2184delTC). We have since identified another homozygous mutation in two siblings affected by SPNET, also within a consanguineous U.K. family of Pakistani origin. Recessively inherited mutations in PMS2 had been previously reported twice [7,8]; however, the association with SPNET had not been seen before. SPNETs are very rare: there are less than 10 cases in the U.K. yearly, so it is unlikely that this is a chance association. Very little is known about molecular correlates of SPNET. There had certainly been no previous evidence implicating MMR genes in SPNET. Combining the data from the families we have described with those previously published, there is evidence of a characteristic phenotype. Haematological malignancies, particularly of T-cell subtype and brain tumours, occur in childhood, with survivors developing CRC in their teenage years (Table 1). Apart from one member of our original family, those children who survived their initial cancers have gone on to develop second primaries. CMLs (chronic myeloid leukaemias) are common, often leading to an initial diagnosis of NF-1 (neurofibromatosis type 1), although none of the cases would The Molecular Biology of Colorectal Cancer Table 1 Recessive mutations reported in MMR genes ALL, acute lymphatic leukaemia; AML, acute myeloid leukaemia; NHL, non-Hodgkin’s lymphoma; PNET, primitive neuroectodermal tumour; wt, wildtype; i, first malignancy; ii, second malignancy; iii, third malignancy. Gene Tumour(s) seen in family members MLH1 CML MLH1 NHL ALL Breast cancer MLH1 MLH1 MLH1 MLH1 NHL AML Glioma Duodenal adenocarcinoma CRC Healthy boy Age of onset (years) 1 3 2 36 2 6 4 11 10 6 R226X/R226X [11] S44F/A441T [12] G67W/G67W [13] Del exon 16/del exon 16 [14] R687W/R687W [15] P648S/P648S [16] [17] [18] p.C1129 V1130 del insL [19] codon 407/codon 787 [7] 1169ins20/1169ins20 [20] 4 13 11 R134X/wt [6] 7 15 13 E705K/wt [9] R802X/R802X [5] ALL NHL Glioblastoma MSH6 Oligodendroglioma CRC i Oligodendroglioma 10 12 14 CRC ii Neuroblastoma 18 13 i CRC PNET Endometrial cancer 14 21 23 Brain tumour ii Astrocytoma iii ALL 24 2 4 PMS2 i Glioblastoma CRC ii CRC PMS2 Astrocytoma NHL CRC PMS2 Reference 1662-1 splice acceptor/1662-1 splice acceptor Del exon 1-6/exon3 del-1 153 MSH2 MSH2 PMS2 Recessive mutations 2 1 3 PMS2 actually fulfil the NIH (National Institutes of Health) consensus criteria for NF-1. Importantly, the phenotype is only seen in sibships in these families, and there is no evidence in any of these families for a dominantly inherited HNPCC phenotype. In fact, there is little evidence in the literature for a dominant phenotype associated with mutations in PMS2. The only remaining case with a reported dominant mutation is that of Miyaki et al. [9]. They reported a boy with an astrocytoma at age 7 years, a lymphoma at 15 and CRC at 16. A single mutation at codon 705 of the PMS2 gene was identified, inherited from the boy’s unaffected mother. The phenotype is reminiscent of that seen in recessive PMS2 families; its presence in his mother suggests that another unidentified mutation in the PMS2 gene was present in this case. Recessive MMR gene mutations Recessive mutations have now been reported in MLH1, MSH2 and MSH6 (Table 1). A consistent phenotype asso- ciated with recessive MMR mutations emerges. This is similar to that seen with mutations in PMS2. Haematological malignancies and brain tumours in childhood, with CRC in adolescence or early adult life, occur frequently. The association with SPNET has so far only been seen with PMS2 in patients of Pakistani origin. In the case of MLH1, MSH2 and MSH6, the recessive phenotype occurs in the context of a family history consistent with HNPCC. In the PMS2 families, there is no history of HNPCC. A further key distinction between dominant HNPCC and those cases with recessive MMR mutations concerns MSI. This is observed in the tumour tissue of patients with dominant MMR mutations. However, in patients with recessive MMR mutations, germline MSI in normal tissue is also observed at high frequency (Table 1). Structure of the PMS2 gene The existence of pseudogenes corresponding to the first five exons of PMS2 has long been recognized. In the analysis of our original family, we demonstrated homozygosity by C 2005 Biochemical Society 719 720 Biochemical Society Transactions (2005) Volume 33, part 4 descent at the PMS2 locus in the affected children. We were therefore surprised when we identified heterozygous changes in exons 3, 4, 5, 13 and 14. These were consistently present in both affected and unaffected individuals. A detailed search of the genome revealed 14 pseudogenes, many corresponding to exons 1–5 and previously described [21]. However, in addition, we identified a novel 100 kb genomic duplicon, containing copies of exons 9 and 11–15. All of these pseudogenes are located on chromosome 7. Mutations in PMS2 have been reported only rarely; however, this could in part be owing to the confounding effect of the pseudogenes. We have published details of the reagents which distinguish gene from pseudogene in our original manuscript [5]. Conclusions Recessive mutations in MMR genes result in a phenotype characterized by the development of haematological malignancies and brain tumours in childhood. Survivors have a high risk of second primaries and often go on to develop CRCs in adolesence or early adult life. The normal tissue of these individuals show evidence of MSI. Recessive mutations in PMS2 seem to be particularly common in the U.K. Pakistani population, where they are associated with a specific phenotype of SPNET. Their contribution to the overall incidence of childhood cancer in this community remains unclear. The genomic architecture of PMS2 is complex. Analysis at this locus in the past has not taken this complexity into account, so the precise role of this gene in carcinogenesis remains poorly defined. Two reports document the occurrence of CRC in PMS heterozygotes [4,10]. In the case of recessive mutations, a distinctive phenotype is becoming apparent; however, there are no simple markers for the disorder, which must be recognized by careful clinical history and examination. 3 Peltomaki, P. and Vasen, H. (2004) Dis. Markers 20, 269–276 4 Nicolaides, N.C., Papadopoulos, N., Liu, B., Wei, Y.F., Carter, K.C., Ruben, S.M., Rosen, C.A., Haseltine, W.A., Fleischmann, R.D. and Fraser, C.M. (1994) Nature (London) 371, 75–80 5 De Vos, M., Hayward, B.E., Picton, S., Sheridan, E. and Bonthron, D.T. (2004) Am. J. Hum. Genet. 74, 954–964 6 Hamilton, S.R., Liu, B., Parsons, R.E., Papadopoulos, N., Jen, J., Powell, S.M., Krush, A.J., Berk, T., Cohen, Z. and Tetu, B. (1995) N. Engl. J. Med. 332, 839–847 7 De Rosa, M., Fasano, C., Panariello, L., Scarano, M.I., Belli, G., Iannelli, A., Ciciliano, F. and Izzo, P. (2000) Oncogene 19, 1719–1723 8 Wang, Q., Lasset, C., Desseigne, F., Frappaz, D., Bergeron, C., Navarro, C., Ruano, E. and Puisieux, A. (1999) Cancer Res. 59, 294–297 9 Miyaki, M., Konishi, M., Tanaka, K., Kikuchi-Yanoshita, R., Muraoka, M., Yasuno, M., Igari, T., Koike, M., Chiba, M. and Mori, T. (1997) Nat. Genet. 17, 271–272 10 Nakagawa, H., Lockman, J.C., Frankel, W.L., Hampel, H., Steenblock, K., Burgart, L.J., Thibodeau, S.N. and de la Chapelle, A. (2004) Cancer Res. 64, 4721–4727 11 Ricciardone, M.D., Ozcelik, T., Cevher, B., Ozdag, H., Tuncer, M., Gurgey, A., Uzunalimoglu, O., Cetinkaya, H., Tanyeli, A., Erken, E. and Ozturk, M. (1999) Cancer Res. 59, 290–293 12 Hackman, P., Tannergard, P., Osei-Mensa, S., Chen, J., Kane, M.F., Kolodner, R., Lambert, B., Hellgren, D. and Lindblom, A. (1997) Nat. Genet. 17, 135–136 13 Wang, Q., Montmain, G., Ruano, E., Upadhyaya, M., Dudley, S., Liskay, R.M., Thibodeau, S.N. and Puisieux, A. (2003) Hum. Genet. 112, 117–123 14 Vilkki, S., Tsao, J.L., Loukola, A., Poyhonen, M., Vierimaa, O., Herva, R., Aaltonen, L.A. and Shibata, D. (2001) Cancer Res. 61, 4541–4544 15 Gallinger, S., Aronson, M., Shayan, K., Ratcliffe, E.M., Gerstle, J.T., Parkin, P.C., Rothenmund, H., Croitoru, M., Baumann, E., Durie, P.R. et al. (2004) Gastroenterology 126, 576–585 16 Raevaara, T.E., Gerdes, A.M., Lonnqvist, K.E., Tybjaerg-Hansen, A., Abdel-Rahman, W.M., Kariola, R., Peltomaki, P. and Nystrom-Lahti, M. (2004) Genes Chromosomes Cancer 40, 261–265 17 Whiteside, D., McLeod, R., Graham, G., Steckley, J.L., Booth, K., Somerville, M.J. and Andrew, S.E. (2002) Cancer Res. 62, 359–362 18 Bougeard, G., Charbonnier, F., Moerman, A., Martin, C., Ruchoux, M.M., Drouot, N. and Frebourg, T. (2003) Am. J. Hum. Genet. 72, 213–216 19 Menko, F.H., Kaspers, G.L., Meijer, G.A., Claes, K., Van Hagen, J.M. and Gille, J.J. (2004) Fam. Cancer 3, 123–127 20 Trimbath, J.D., Petersen, G.M., Erdman, S.H., Ferre, M., Luce, M.C. and and Giardiello, F.M. (2001) Fam. Cancer 1, 101–105 21 Nicolaides, N.C., Carter, K.C., Shell, B.K., Papadopoulos, N. and Kinzler, K.W. (1995) Genomics 30, 195–206 References 1 Peltomaki, P. (2001) Hum. Mol. Genet. 10, 735–740 2 Harfe, B.D. and Jinks-Robertson, S. (2000) Annu. Rev. Genet. 34, 359–399 C 2005 Biochemical Society Received 22 March 2005