* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download FUN2: 11:00-12:00 Scribe: Taylor Nelson Wednesday, December
Survey
Document related concepts
CCR5 receptor antagonist wikipedia , lookup
NMDA receptor wikipedia , lookup
Discovery and development of antiandrogens wikipedia , lookup
5-HT2C receptor agonist wikipedia , lookup
Toxicodynamics wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
Nicotinic agonist wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Neuropharmacology wikipedia , lookup
Norepinephrine wikipedia , lookup
Transcript
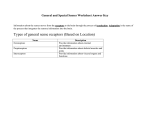
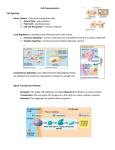
FUN2: 11:00-12:00 Scribe: Taylor Nelson Wednesday, December 03, 2008 Proof: Hunter Neill Dr. Besse Adrenergics 2 Page 1 of 4 NE – norepinephrine; AC – acetylcholine; VMAT – vesicle membrane associated transport; MAO – monoamineoxidase; COMT - Catochol o methyltransferase; BP – blood pressure; SA - sinoatrial Sympathertic postganglionic nerve terminal I. [S1] Processes involving Norepinephrine (NE) a. Synthesis, storage, release, termination of physiological activity b. We know more about the activity in these terminals than in the postsynaptic or somatic nerve terminal c. The precurser for the biosynthesis is tyrosine and enters the nerve terminal through a sodium dependent carrier mechanism i. Undergoes 3 enzymatic steps before NE 1. In the adrenal medulla there is a 4th enzymatic step which adds and methyl group to the amino group of NE and results in E (ONLY IN THE adrenal medulla) 2. In NERVE TERMINALS there is a conversion of tyrosine by tyrosine hydroxylase (the rate limiting step of the biosynthesis of NE) to for Dopa a. Significance of Dopa- Parkinsonism (L-Dopa) 3. Dopa is converted to Dopamine in the cytoplasm of the nerve terminal 4. The Dopamine enters the storage granuoles of vesicle in the sympathetic nerve terminals and then converted to NE a. Again we have an association transported mechanism VMAT (vesicle membrane associated (transport) carrier mechanism) b. VMAT – is not specific for dopamine – other compound can enter through that carrier mechanism and into the nerve terminal c. VMAT – Antihypertensive drug – one compound that has faded from a blood pressure lowering agent called Reserpine i. Blocks VMAT and sympatheric nerve terminals will eventually be depleted of NE ii. If you have less NE to act on adrenergic receptors in blood vessels (in a patient which has a lot of it and hypertension you will lower hypertension) iii. A drug used for the treatment of moderate hypertension d. Like acetylcholine (AC), NE can be stored with other compounds (ATP and other potential co-transmitters that will be released with NE from the vesicles) II. Release mechanism for NE a. Exactly like the AC b. A wave of depolarization comes down the axon c. The depolarization results in the opening of Ca channels d. Ca flows in and acts as a catalyst for the fusion of the VAMPs and the synapse e. When this occurs the vesicle and the membrane open and NE is released into the junctional space, where it will interact with adrenergic receptors i. Alpha 1 ii. Beta 1 (NOT Beta 2) III. Physiological activity a. What controls the activity of NE? Not metabolism, but rather the NE in the extra junctional space will be taken up by the carrier mechanism NET transporter b. The NE in this space has high affinity for this carrier mechanism which will take it back into the nerve terminal i. Reducing the concentration in the junction that would be free to react as an agonist on the andrenergic receptors c. Once inside of the nerve terminal i. If the NE escapes monoamineoxidase (MAO) (associated with mitochondria – oxidizes the end of the NE molecule) it will again be taken up through the VMAT and stored again in the vesicles ii. It will be subsequently released again d. That uptake process involving NET is loosely termed Uptake 1 i. This is the mechanism whereby the physiological activity of the sympathetic transmitter – NE – is regulated IV. Pre-synaptic receptors/ Auto receptors/ Hetero receptors a. The Auto receptor for NE is termed Alpha2 b. The tissue alpha receptor are Alpha1 c. NE by binding as an agonist to the Alpha2 will generate cAMP which will eventually result in some hyper polarization of the vesicle membrane and reduce the opening of Ca channels i. Subsequently reducing the release of the transmitter by the nerve impulse d. It is the control mechanism for NE on its own rate of release FUN2: 11:00-12:00 Scribe: Taylor Nelson Wednesday, December 03, 2008 Proof: Hunter Neill Dr. Besse Adrenergics 2 Page 2 of 4 e. Hetero receptors – compounds of various types can bind to the hetero receptor and either increase or decrease the release of NE from the storage vesicles in sympathetic nerve terminals i. AC is on possible example that will bind to a hetero receptor ii. Accentuated Antagonism – AC in the ventricles would bind to a hetero receptor M3 to antagonize the release of NE (NOT ON TEST) V. NET transporter system a. Any number of compounds (somewhat limited) – more than NE can penetrate including epinephrine b. There is a compound cocaine and a group of compounds – tricyclic antidepressant agents – that will block the uptake 1 or NET process of sympathetic nerve terminals i. This action of cocaine will involve cardiovascular functions ii. If it blocks uptake it will allow greater of NE to exist in the space (synapse) 1. And more NE is available to interact with the receptors resulting in a potentiated response to NE 2. Because cocaine has blocked the NET uptake 1 mechanism iii. Same thing applies to the tricyclic antidepressant agents – they block NET transporter system VI. Nerve terminal – INDIRECT MECHANISM a. Indirect acting sympathomimetic compounds i. The use of the term indirect is the same as the use for the term Cholinergic stimulus ii. These compounds produce their effects by releasing NE from the nerve terminals iii. They do not inhibit an enzyme iv. The best example, with a major indirect mechanism of action is amphetamine and its various derivatives v. A naturally occurring substance in foods that will have the same effect by has no abuse as a drug is: 1. Tyramine – (NOT ON TEST) b. Amphetamine and tyramine are the two examples of indirect acting compounds (will not see tyramine on the exam but could see amphetamine) c. Both can get through the NET uptake process and eventually find their way into the vesicle and displace NE from the vesicles. i. If the NE escape metabolism by MAO it will go back in reverse fasion through this uptake mechanism into the junctional space and produce NE like effects VII. Story about Tyramine (already stated would not be covered on the exam) a. In the mid 80s a group of young men and women in Great Britian were being treated with a MAO inhibitor for depression b. Doing great except for enjoying cheese, ale, beer with ale like qualities and by midnight ending up in a hospital is blood pressure (BP) of 300 systolic. Why? c. The food and drinks contain high concentration of tyramine (bananas also) d. Tyramine is a good substrate for MAO – totally inactivates it e. Instead of some NE being release indirectly by tyramine, now you have tyramine in higher concentration causeing the release of overwhelming amounts of NE throughout sympathetic nerve terminals causing the BP to increase (cerebrovascular accidents) i. A good number of theses people on MAO inhibitors – died f. Investigation of this phenomenon lead to indirect acting sympathomimetics g. Same things could happen to someone taking amphetamine who is also on MAO inhibitor therapy VIII. One more enzyme that can attack another portion of NE molecule a. It attacks the hydroxyl ring b. That enzyme located mainly in the liver (also elsewhere) is named Catochol o methyltransferase (COMT) c. That also tell you where it has its action on the NE molecule IX. MAO of COMT a. Either MAO activity or COMT activity abolishes the physiological action of NE b. In terms of sympathetic nerve terminal function – it is the NET uptake process that is the major determinant c. Once the NE gets out into the circulation the activity of COMT or MAO because it too has widespread distribution d. Either one or both of the enzymes will act on the NE molecule as well as the epinephrine molecule and then activate FUN2: 11:00-12:00 Scribe: Taylor Nelson Wednesday, December 03, 2008 Proof: Hunter Neill Dr. Besse Adrenergics 2 Page 3 of 4 X. Sympathomimetic Effects [S2] a. A number of them will be illustrated in the diagram b. In general sympathomimetic agonist drugs interact with alpha of beta receptors and result in vasoconstriction, vasodilation, positive chronotropic, ionotropic, and dromotropic effects on the heart c. They promote lipolysis and glycogenolysis for the liberation of glucose from the liver d. Relaxation of smooth muscles applies to a restricted case mainly of the bronchiole smooth muscle in asthma e. In order to understand these broad effects there are two key elements – 1.) you need to know the relative major receptor affinities (listed in the following chart) of norepinephrine, epinephrine, isoproterenol, and phenylephrine (each are prototypic examples of sympahtomimetic amines) for alpha and beta receptors 1 2 1 2 Norepinephrine Epinephrine Isoproterenol Phenylephrine i. Norepinephrine combines with 1, 2, and 1(sympathetic transmitter in the heart), but does not have any measurable affinity for the 2 receptors 1. 2’s, in the lungs (bronchial smooth muscle) and in the blood vessels (primarily those supplying the skeletal muscle) are not innervated, they are just there and they will respond if the appropriate agonist binds to them 2. 1 involves the elaboration of inositol triphosphate - beta receptor stimulation involves the elaboration of cAMP ii. Epinephrine has affinity for all four types of receptors, 1, 2, 1, and 2 iii. Isoproterenol is a pure beta agonist but has no selectivity for 1, or 2 – it stimulates either variety equally iv. Phenylphrine and Methoxamine (in the drug list) are virtually pure specific agonists at 1 receptors f. The second major element in understanding the diagram is the baroceptor mechanism for the control of changes in blood pressure i. There are sensing elements/receptors located in the carotid sinus and in the arch of the aorta. Nerve fibers from these two regions travel into the medulary area within the brain and stimulate the vagal nucleus; if the stimulus traveling up these nerve impulses is strong enough they will also inhibit sympathetic outflow from the medullary area in the brain. Stimulation of the vagus nerve will ultimately result in the release of acetylcholine, and since we’re talking about control of blood pressure we’re talking about acetylcholine being released at the SA node (as well as other parasympathetic innervations) of the heart. For purposes of [S2] we’ll be talking about enhanced or diminished vagal activity at the SA node. ii. Stretch on the vascular smooth muscle stimulates these sensing elements in the aortic arch and carotid sinus (translates into increased vascular resistance) iii. When this occurs, the mechanism involving the efferent nerves into the brain and the afferent impulses down the vagus, activity in this system is increased when peripheral resistance increases – blood pressure goes up and the body wants to bring it down, this mechanisms actually operates from breath to breath for a relatively precise control of systemic blood pressure g. So we have the affinities for these prototypical compounds (from chart) for the major (not all) adrenergic juncti onal receptors, of course in the case of 2 we have the pre-synaptic receptors h. [S2] i. Top line on slide – measuring heart rate (beats per minute); middle section – measuring pulse pressure (systolic/diastolic); bottom line – qualitative measure in peripheral resistance (line up = resistance increased, line down = resistance decreased) ii. The doses are as low as we can get away with, i.e. physiological amounts as opposed to pharmacological amounts (less than a microgram per kilogram – physiological rather than pharmacological amounts) iii. Norepinephrine 1. Extremely potent agonist at 1 receptors (recall 1 receptor stimulation increases chronotropy, ionotrophy, and dromotropy) 2. All 1, 2, 1 3. Considering the responses: a. Increase in peripheral resistance – there are many more 1 receptors in blood vessels than ’s b. Pulse pressure changes – rise in resistance is reflected by the increase in diastolic pressure, the rise in systolic pressure is due to the activity of the heart (positive ionotropic affect of norepinephrine on the ventricles) FUN2: 11:00-12:00 Scribe: Taylor Nelson Wednesday, December 03, 2008 Proof: Hunter Neill Dr. Besse Adrenergics 2 Page 4 of 4 c. Decrease in heart rate – rise in resistance activates the baroceptor mechanism causing an increase in the release of acetylcholine at the SA node overcoming the direct effect of norepinephrine at the SA node leading to a net effect of bradycardia – remember two autonomic systems working here, in this circumstance the parasympathetic system dominates the sympathetic system, so there is said to be a reflex bradycardia to the administration of norepinephrine iv. Epinephrine 1. Combines with all four of the major adrenergic receptors 2. Considering the responses: a. Causes a drop in peripheral resistance – skeletal muscles need oxygen, glucose (energy supply), and blood flow so we have a compound that will achieve two of the above that are of pharmacological interest, epinephrine will increase blood flow to the skeletal muscles by dilating blood vessels. What about the 1’s? Epinephrine has a greater affinity for 2 than 1 when “given the choice.” Physiological amounts will cause vasodilation in the blood vessels supplying the skeletal beds, but everywhere else epinephrine will be an 1 agonist ( receptors are highly concentrated in the blood vessels supplying the skeletal beds). b. Pulse pressure changes – diastolic pressure remains more or less the same, systolic pressure increases. Epinephrine has affinity for 1, improves the contractile activity of the heart c. Increase in heart rate - 1 effect clearly evident because we haven’t increased the activity of the baroceptor mechanism nor have we enhanced the release of acetylcholine at the SA node v. Isoproterenol 1. Non-selective agonist at both 1 and 2 2. Considering the responses: a. Causes a big drop in peripheral resistance – no affinity for 1, its only effect in blood vessels will be vasodilation b. Pulse pressure changes – diastolic pressure drops due to the drop in resistance, systolic pressure still rises because isoproterenol is the most potent stimulant of 1 receptors c. Rather large increase in heart rate (tachycardia) – due to the direct 1 effect on the ventricle and a reduction in the activity of the baroceptor system i. The baroceptor mechanism operates in a blood pressure range from 60mmHg to 180mmHg, we get lower in the diastolic pressure reflecting peripheral resistance so the activity of the reflex diminishes – resulting in the direct effect of isoproterenol on the 1 receptors as well as the “indirect effect” of reduced baroceptor input vi. Phenylephrine 1. Derivative of norepinephrine 2. Specificity for the alpha receptors and a high degree of selectivity for the 1 none on the 2 3. In effect it is a pure vasoconstrictor, will have no direct effect on the heart because it’s all betas in the heart 4. Considering the responses: a. Rise in peripheral resistance b. Pulse pressure changes – rise in diastolic pressure, no change in systolic pressure c. Reflex bradycardia – the only input on the SA node (other than resting) is enhanced baroceptor receptor activity and enhanced release of acetylcholine which results in decreased heart rate vii. If you keep in mind the general effects of sympathomimetic amines, the receptor affinities for sympathomimetic amines, and keep in the back of your head how the baroceptor mechanism may modify things such as blood pressure you will do well on the next exam. [End at 43:30]