* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download SMU-DDE-Assignments-Scheme of Evaluation PROGRAM Bachelor
Discovery and development of antiandrogens wikipedia , lookup
Discovery and development of beta-blockers wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Compounding wikipedia , lookup
Orphan drug wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Pharmacognosy wikipedia , lookup
Drug discovery wikipedia , lookup
Prescription costs wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Drug design wikipedia , lookup
Psychopharmacology wikipedia , lookup
Nicotinic agonist wikipedia , lookup
Drug interaction wikipedia , lookup
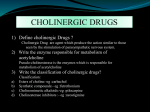
SMU-DDE-Assignments-Scheme of Evaluation PROGRAM SEMESTER SUBJECT CODE & NAME BK ID SESSION MARKS Q.No 1. A Bachelor/Diploma in Medical Imaging Technology II BMI 204– Basics of Pharmacology B1950 WINTER 2015 30 Criteria Marks Total Marks Define pharmacology. Explain pharmacodynamic and pharmacokinetic principles. (Unit 1;Section 1.2 & 1.5;Pg 2,17-19) Pharmacology is the study of drugs and their effects on life processes. It 1 10 is a fundamental science that has reached the forefront of modern medicine by demonstrating success in treating disease and saving lives. The actions of the drug on the body are termed as pharmacodynamics. The effect of a drug present at the site of action is determined by that drug’s binding with a receptor. However, at the molecular level, drug binding is only the first among a complex set of events. Types of drug – receptor interactions: Agonist drugs bind to and activate the receptor in some fashion, which directly or indirectly brings about the effect. Some receptors incorporate effector machinery in the same molecule, so that drug binding brings about the effect directly, e.g., opening of an ion channel or activation of enzyme activity. Other receptors are linked through one or more intervening coupling molecules to a separate effector molecule. "Agonists" that inhibit their binding molecules and partial agonists: Some drugs mimic agonist drugs by inhibiting the molecules responsible for terminating the action of an endogenous agonist. For example, acetylcholinesterase inhibitors, by slowing the destruction of endogenous acetylcholine, cause cholinomimetic effects that closely resemble the actions of cholinoceptor agonist molecules. Duration of drug action: Termination of drug action at the receptor level results from one of several processes. In some cases, the effect lasts only as long as the drug occupies the receptor, so that dissociation of drug from the receptor automatically terminates the effect. In many cases, however, the action may persist after the drug has been dissociated. Receptors and inert binding sites: To function as a receptor, an endogenous molecule must first be selective in choosing ligands (drug molecules) to bind; and second, it must change its function upon binding in such a way that the function of the biologic system (cell, tissue, etc) is altered. 4.5 SMU-DDE-Assignments-Scheme of Evaluation 2. A Pharmacokinetic processes govern the absorption, distribution, and elimination of drugs and are of great practical importance in the choice and administration of a particular drug for a particular patient, e.g., one with impaired renal function. In practical therapeutics, a drug should be able to reach its intended site of action after administration by some convenient route. In some cases, a chemical that is readily absorbed and distributed is administered and then converted to the active drug by biologic processes inside the body. Such a chemical is called a prodrug. In only a few situations it is possible to directly apply a drug to its target tissue E.g., Topical application of an anti-inflammatory agent to inflamed skin or mucous membrane. Most often, a drug is administered into a body compartment, like the gut, and is moved to its site of action in another compartment, say the brain. This requires that the drug be absorbed into the blood from its site of administration and distributed to its site of action, permeating through various barriers that separate these compartments. For an oral drug affecting the central nervous system, these barriers include the tissues comprising the intestinal wall, the capillary wall that perfuse the gut and the blood-brain barrier or the walls of capillary that perfuse the brain. Finally, after bringing about its effect, a drug should be eliminated at a reasonable rate by metabolic inactivation, by excretion from the body, or by a combination of these processes. 4.5 Discuss the classification, pharmacological actions, uses and adverse effects of cholinergic agonists. (Unit 2;Section 2.3;Pg 30-32) Cholinergic agonists are also known as parasympathomimetics or 1 10 cholinomimetics. These are the drugs that produce the action similar to that of parasympathetic simulations. They basically act either by directly interacting with cholinergic receptors (cholinergic agonists) or by increasing availability of Ach at these sites (anticholinesterases). 2 Classification 1. Choline esters: ACh, Methacholine, Carbochol, Bethanechol. 2.Natural alkaloids a) Muscarinic: Muscarine, Pilocarpine, Arecholine. b) Nicotinic: Nicotine, Lobeline, Dimethylphenylpiperazinium (DMPP) 3. Synthetic alkaloids: Areclinidine, Oxotremorine. 4 Pharmacological actions Depending on which receptors Ach is binding to, peripheral actions can be either muscarinic or nicotinic. a) Cardiovascular system: i) ACh hyperpolarizes SA nodal cells: ↓ rate of diastolic depolarization therefore, ↓ rate of impulse generation. Therefore it causes bradycardia or even cardiac arrest. ii) At AV node and His-Purkinje fibres: ↑ refractory period and ↓ conduction which causes partial AV blockade leading to ↓ force of atrial contraction thereby reducing ventricular contractility. SMU-DDE-Assignments-Scheme of Evaluation 3. b) Blood vessels: Decrease in blood pressure due to NO-mediated vasodilatation. c) Gastrointestinal tract: The G.I. tract is contracted. There is increased tone, motility and peristalsis. The sphincters are relaxed, thus there is rapid propulsion of food. Detrusor muscle is contracted. d) Respiratory system: Bronchial muscle are contracted to produce bronchospasm. This may cause apnea (temporary absence or cessation of breathing). Hence, cholinergic drugs are contraindicated in asthmatic condition. e) Glands: Increase secretions from all glands. f) Eye: Cholinergic drugs cause contraction of circular muscles of iris. Hence, they produce miosis. It even contracts ciliary muscles which causes spasm of accommodation and reduction in intraoccular tension. g) Skeletal muscles: Parasympathomimetics contract the skeletal muscles through nicotinic effect. Anticholinesterases in particular increase the strength of muscle contraction and may produce fibrillation and fasciculations. Some Anticholinesterases are useful in myasthenia gravis. 2 Uses: Bethanechol is used in post-operative or post-partum urinary retention, neurogenic bladder atony, congenital megacolon, gastroesophageal reflux. Carbachol is rarely used therapeutically except in the eye as a miotic agent to treat glaucoma to decrease the intraocular pressure. Pilocarpine is used only in the eyes as 0.5-4% drops in open angle glaucoma. Pilocarpine and cevimeline, a newer muscarinic receptor agonist increases salivary secretions. They are used to treat Sjogren’s syndrome (a systemic autoimmune disease in which immune cells attack and destroy the exocrine glands that produce tears and saliva.) Methacholine is occasionally used to diagnose bronchial hypersensitivity and asthmatic conditions. 1 Adverse effects: Belching, colic, involuntary urination, defecation, flushing, sweating, fall in blood pressure, bronchospasm. Discuss the drugs used for peptic ulcers. (Unit 5;Section 5.2;Pg 85-89) SMU-DDE-Assignments-Scheme of Evaluation A 2+2+2+2+2 Explanation of the following 10 1. Reduction of gastric acid secretion a) H2-antihistamines: Cimetidine, Roxatidine, Loxatidine Ranitidine, b) Proton pump inhibitors: Omeprazole, Pantoprazole, Rabeprazole, Esomeprazole Famotidine, Lansoprazole, c) Anticholinergics: Pirenzepine, Propantheline, Oxyphenonium d) Prostaglandin analogues: Misoprostol, Enprostil, Rioprostil 2. Neutralizing of gastric acid (Antacids) a) Systemic: Sodium bicarbonate, Sodium Citrate b) Non-systemic: Magnesium hydroxide, Magnesium trisilicate, Aluminium hydroxide gel, Magaldrate, Calcium carbonate 3. Ulcer protectives: Sucralfate, Colloidal bismuth subcitrate (CBS) 4. Ulcer healing drugs: Carbonoxolone sodium 5. Anti-H. pylori drugs: Amoxicillin, Clarithromycin, Metronidazole, Tinidazole, Tetracycline *A-Answer Note –Please provide keywords, short answer, specific terms, specific examples (wherever necessary) ***********