* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Uncoupling insulin signalling by serine/threonine phosphorylation: a
Survey
Document related concepts
Biochemical switches in the cell cycle wikipedia , lookup
List of types of proteins wikipedia , lookup
Protein moonlighting wikipedia , lookup
Tyrosine kinase wikipedia , lookup
Intrinsically disordered proteins wikipedia , lookup
G protein–coupled receptor wikipedia , lookup
Signal transduction wikipedia , lookup
Phosphorylation wikipedia , lookup
Transcript
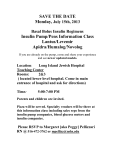
812 Biochemical Society Transactions (2004) Volume 32, part 5 Uncoupling insulin signalling by serine/threonine phosphorylation: a molecular basis for insulin resistance Y. Zick1 Department of Molecular Cell Biology, The Weizmann Institute of Science, Rehovot 76100, Israel Abstract Insulin resistance refers to a decreased capacity of circulating insulin to regulate nutrient metabolism. Recent studies reveal that agents that induce insulin resistance exploit phosphorylation-based negative feedback control mechanisms otherwise utilized by insulin itself to uncouple the insulin receptor from its downstream effectors and thereby terminate insulin signal transduction. This article focuses on the Ser/Thr protein kinases which phosphorylate insulin receptor substrates and the major Ser sites that are phosphorylated, as key elements in the uncoupling of insulin signalling and the induction of an insulin resistance state. Insulin signalling Insulin is the major anabolic hormone whose action is essential for growth, development, homoeostasis of glucose, fat and protein metabolism, and for the proper function of pancreatic beta cells [1]. At the molecular level, insulin binding to its transmembrane receptor (IR) stimulates the intrinsic tyrosine (Tyr) kinase activity of the receptor (IRK), which then phosphorylates selected Tyr residues of target proteins. IR substrates include IRS (IR substrate) proteins (IRS-1–6), Shc proteins, p60dok, Cbl, APS and Gab-1 [1–3]. The Tyr-phosphorylated IRSs function as signalling scaffolds, providing a docking interface for downstream effectors having Srchomology 2 (SH2) domains that further propagate the metabolic and growth-promoting effects of insulin. IRS proteins are considered as the major IR substrates. They contain a conserved PH (pleckstrin homology) domain, located at their N-terminus, that serves to anchor the IRS proteins to membrane phosphoinositides, which helps to localize the IRS proteins in close proximity to the IR [4]. The PH domain is flanked by a PTB (phospho-Tyr binding) domain that functions as a binding site to the NPXY motif of the juxta-membrane region of IR, IGF-IR (insulinlike growth factor-1 receptor) and other receptors [5]. The C-terminal region of IRS proteins contains multiple Tyr phosphorylation motifs that serve as docking sites for SH2domain-containing proteins, including the p85α regulatory subunit of PI3K (phosphoinositide 3-kinase), Grb2, Nck, Crk, Fyn and the SH2-domain-containing tyrosine phosphatase SHP-2, which mediate various aspects of insulin action [1–3]. IRS proteins contain over 70 potential Ser/Thr residues with homologies to consensus phosphorylation sites of different kinases. In non-treated cells, IRS-1 is heavily phosphorylated on Ser residues and weakly phosphorylated on Tyr residues, whereas following insulin stimulation, Tyr and Ser phosphorylation of IRS-1 is increased. Ser phosphorylation of IRS-1 reduces its ability to undergo Tyr phosphorylation and, in general, serves to turn off insulin signalling [2] (see below). Insulin signalling propagates through three major pathways: the PI3K, the MAPK (mitogen-activated protein kinase) and the Cbl/CAP (Cbl-associated protein) pathways, each having some unique characteristics. Insulin-mediated activation of the MAPK cascade leads to enhanced cell growth, while association of PI3K with IRS proteins following insulin stimulation results in production of phosphatidylinositol 3,4,5-trisphosphate (PIP3 ) that activates PDK1 (PIP3 -dependent kinase 1) and its downstream effectors PKB (protein kinase B; also named Akt), mTOR (mammalian target of rapamycin), p70 S6 kinase, as well as the atypical isoforms of protein kinase C (PKC ζ /λ), all leading to enhanced glucose transport, glycogen and protein synthesis [6]. Tyr phosphorylation of Cbl by IRK mediates glucose transport in a PI3K-independent manner through activation of the GTP-binding protein TC10 and its interaction with the exocyst complex and the Cdc42-interacting protein 4/2 [7,8]. Collectively, these signalling pathways mediate the metabolic and growth-promoting functions of insulin. Inhibition of insulin signalling Key words: insulin resistance, insulin signalling, serine/threonine phosphorylation. Abbreviations used: IR, insulin receptor; IRK, IR kinase; IRS, IR substrate; SH2, Src-homology 2; PH, pleckstrin homology; PTB, phospho-Tyr binding; PI3K, phosphoinositide 3-kinase; MAPK, mitogen-activated protein kinase; PIP3 , phosphatidylinositol 3,4,5-trisphosphate; PDK1, PIP3 dependent kinase 1; PKB, protein kinase B; PKC, protein kinase C; mTOR, mammalian target of rapamycin; IGF-I(R), insulin-like growth factor-1 (receptor); IKKβ, I-kappa B kinase β; NF-κB, nuclear factor-κB; JNK, c-Jun N-terminal kinase; TNFα, tumour necrosis factor α; FFA, free fatty acid. 1 email [email protected] C 2004 Biochemical Society The duration and extent of insulin signalling is regulated at several levels. Some of the control mechanisms are set into motion immediately following insulin stimulation. They act to terminate insulin’s effects through activation of lipid or protein phosphatases and through the induction of Ser/Thr kinases that phosphorylate and uncouple various elements along the insulin signalling pathways. Other Signalling Outwards and Inwards Figure 1 The impact of Ser/Thr phosphorylation of IRS on insulin action Ser/Thr phosphorylation of IRS protein can either enhance or terminate insulin’s signal. Ser residues at the PTB domain of IRS-1, located within consensus PKB phosphorylation sites, presumably function as positive effectors of insulin signalling by protecting IRS proteins from the action of PTPs. Other insulin-stimulated Ser/Thr kinases, including mTOR, JNK, PKCζ and IKKβ, mediate phosphorylation of IRS proteins. Phosphorylation of IRS proteins by these kinases is part of a negativefeedback control mechanism, induced by insulin, that results in the termination of insulin signal. Inducers of insulin resistance take advantage of this negative-feedback control mechanism by activating either the same or other Ser/Thr kinases that phosphorylate the IRS proteins, inhibit their function, terminate insulin action and induce insulin resistance. pY, phospho-Tyr; pS, phospho-Ser. negative feedback control mechanisms operate on a longer time scale, and involve a reduction in the cellular content of the IR, its substrates and other signalling elements. Ser phosphorylation of IRS proteins: a physiological means to terminate insulin signalling Control over insulin signalling can be achieved by autoregulation, whereby downstream enzymes inhibit upstream elements (homologous desensitization). Alternatively, signals from apparently unrelated pathways can inhibit insulin signalling by heterologous desensitization. The IR, IRS and Shc proteins are subjected to such complex control. Studies in our laboratory have focused on Ser/Thr phosphorylation of IRS proteins as a key feedback control mechanism that uncouples the IRS proteins from their upstream and downstream effectors and terminates signal transduction in response to insulin [2,9,10]. We have shown that insulin-stimulated Ser/Thr phosphorylation of IRS proteins has a dual function in serving as either a positive or a negative modulator of insulin signalling (Figure 1). Phosphorylation of Ser residues within the PTB domain of IRS-1 by PKB, in response to insulin stimulation, protects IRS proteins from the rapid action of PTPs (protein Tyr phosphatases), and enables the IRS proteins to maintain their Tyr-phosphorylated active conformation, thus implicating PKB as a positive regulator of IRS-1 functions [11]. Indeed, mutation of Ser-302 of IRS-1, a potential PKB phosphorylation site, reduces insulin/ IGF-I-stimulated DNA synthesis, indicating that IRS-1 phosphorylation at this site promotes mitogenesis and cell growth [12]. By contrast, Ser/Thr phosphorylation of IRS proteins by other insulin-stimulated Ser/Thr kinases, such as PKCζ [10], serves as a physiological negative feedback control mechanism that inhibits further Tyr phosphorylation of IRS proteins. Ser/Thr phosphorylation can: induce the dissociation of IRS proteins from the IR [9,10]; hinder Tyr phosphorylation sites of IRS proteins [13]; release the IRS proteins from intracellular complexes that maintain them in close proximity to the receptor [14]; induce IRS protein degradation [15]; or turn IRS proteins into inhibitors of the IRK [16]. These multiple effects place the spotlight on the Ser/Thr kinases that phosphorylate the IRS protein, and on the Ser/Thr sites that are getting phosphorylated. The activity of insulin-stimulated IRS kinases is blocked by inhibitors of the PI3K pathway, implicating downstream effectors of PI3K as negative regulators of IRS protein C 2004 Biochemical Society 813 814 Biochemical Society Transactions (2004) Volume 32, part 5 function [10,11]. One potential candidate is mTOR, which enhances phosphorylation of Ser residues at the C-terminus of IRS-1. This phosphorylation inhibits insulin-stimulated Tyr phosphorylation of IRS-1 and its ability to bind PI3K [17]. Another candidate is PKCζ . PKCζ mediates phosphorylation of IRS proteins [10,18], which leads to the dissociation of the IR–IRS complexes [10,19]. This inhibits the ability of IRS proteins to undergo further insulinstimulated Tyr phosphorylation, and as a result, it terminates insulin signalling. IRS-1 serves as a substrate for PKCζ in vitro, and endogenous IRS-1 forms complexes with PKCζ in an insulin-dependent manner [18]. These findings suggest that PKCζ can function as an insulin-stimulated IRS kinase. Ser-318 is a potential target for PKCζ -mediated phosphorylation of IRS-1 [20]. Because Ser-318 is adjacent to the PTB domain of IRS-1, its phosphorylation presumably disrupts the interaction between the juxtamembrane domain of the IR and the PTB domain of IRS-1, and in such a way inhibits insulin-stimulated Tyr phosphorylation of IRS-1. Another potential IRS kinase is IKKβ (I-kappa B kinase β). IKKβ is a Ser/Thr kinase that is part of the IKK complex that phosphorylates the inhibitor of nuclear factor-κB (NF-κB), IκB. This results in the degradation of IκB, allowing for the nuclear translocation and activation of the transcription factor NF-κB [21]. IKKβ is a downstream effector of PKCζ . It can bind PKCζ both in vitro and in vivo; it serves as an in vitro substrate for PKCζ , and it is activated by a functional PKCζ [22]. IKKβ is activated by insulin in Fao rat hepatoma cells; furthermore, insulin-stimulated Ser phosphorylation of IRS-1 is inhibited by salicylates, implicating IKKβ as an insulin-stimulated IRS kinase (Y.F. Liu and Y. Zick, unpublished work). This conclusion is supported by findings indicating that IRS-1 is a direct substrate for IKKβ that phosphorylates IRS-1 on Ser-312 (the human homologue of mouse Ser-307) following cellular stress [23]. Another IRS kinase is JNK (c-Jun N-terminal kinase), a member of the MAPK family of protein kinases, which is activated by insulin by as yet unknown mechanism. Recent studies have shown that JNK associates with IRS-1 and phosphorylates it at Ser-307 in an insulin-dependent manner [24]. Insulin stimulation of JNK activity requires PI3K and Grb2 signalling, suggesting that JNK activation is mediated by a number of signalling pathways. Direct binding of JNK to IRS-1 is not required for JNK activation by insulin; however, direct interactions between JNK and IRS-1 are required for Ser-307 phosphorylation [24]. PKB, mTOR, PKCζ and IKKβ are downstream effectors of PI3K along the insulin signalling pathway. This suggests that their action should be orchestrated to allow the phosphorylation of IRS proteins by PKB (their positive regulator) to take place prior to the phosphorylation of IRS proteins by mTOR, JNK or PKCζ , the negative regulators of IRS protein function. Of note, the negative-feedback control mechanism induced by PKCζ (or mTOR) includes a self-attenuation mode, whereby PI3K-mediated activation of mTOR and PKCζ inhibits IRS-1 function; thereby inhibiting further activation of mTOR and PKCζ themselves [2,10]. C 2004 Biochemical Society Ser phosphorylation of IRS proteins and insulin resistance Insulin resistance is a common pathological state in which target cells fail to respond to ordinary levels of circulating insulin [25]. Individuals with insulin resistance are predisposed to developing Type II diabetes, a 21st century epidemic. Insulin resistance is frequently associated with a number of other health disorders, including obesity, hypertension, chronic infection and cardiovascular diseases, making it the focus of interest for a large number of studies [25]. Emerging data suggest that agents such as TNFα (tumour necrosis factor α), FFAs (free fatty acids) and cellular stress that inhibit insulin signalling and induce insulin resistance activate Ser/Thr kinases that phosphorylate the IRS proteins and inhibit their function. Hence Ser/Thr phosphorylation of IRS proteins that uncouples them from their upstream and downstream effectors in response to insulin under physiological conditions could also be the underlying mode of action of inducers of insulin resistance [2]. This means that Ser phosphorylation of IRS proteins represents an important new mechanistic theme that should be considered alongside other potential mechanisms as the underlying cause of insulin resistance. Because Ser/Thr phosphorylation of IRS proteins is stimulated by insulin treatment and by inducers of insulin resistance, it suggests that the same Ser kinases might be utilized to phosphorylate the IRS proteins under both physiological and pathological conditions (Figure 1). This conclusion is based, for example, upon the fact that TNFα can induce activation of sphingomyelinase and production of ceramide, which stimulates PKCζ and its downstream target IKKβ. Indeed, the inhibitory effects of TNFα on insulinstimulated Tyr phosphorylation of IRS proteins are mimicked by sphingomyelinase and ceramide analogues [9,26]. TNFα can also induce complex formation between PKCζ , p62 and RIP proteins that serve as adaptors of the TNF receptor and link PKCζ to TNFα signalling [27]. ‘Novel’ PKC isoforms, such as PKCθ, can also act as IRS kinases. These kinases were implicated as mediators of FFA-induced insulin resistance in skeletal muscle, in a process that involves phosphorylation of IRS-1 at Ser-307 [28]. In contrast, ‘conventional’ members of the PKC family, such as PKCα, which are activated by phorbol esters or endothelin-1, utilize members of the MAPK pathway to phosphorylate IRS-1 at Ser-612 (located in a consensus MAPK phosphorylation site) and at additional sites in its C-terminal tail [29,30]. IKKβ is another potential IRS kinase, the activity of which is stimulated by FFAs, pro-inflammatory cytokines and other inducers of insulin resistance. Activation or overexpression of IKKβ attenuates insulin signalling, whereas IKKβ inhibition by high doses of salicylates or by a reduction in IKKβ gene dose reverses obesity- and diet-induced insulin resistance in animal models [31] and improves glucose metabolism in Type II diabetic subjects [32]. The mechanism by which FFAs might activate IKKβ presumably involves an increase in FFA-derived metabolites, such as diacylglycerol and ceramide, which are potent activators of PKCθ and PKCζ , both Signalling Outwards and Inwards known to activate IKKβ. At the molecular level, inhibition of IKKβ prevents Ser/Thr phosphorylation of IRS proteins induced by a high-fat diet, TNFα or phosphatase inhibitors, whereas it improves insulin-stimulated Tyr phosphorylation of IRS proteins. Hence IKKβ might serve as a point of convergence, where Ser kinases downstream of insulin signalling and Ser kinases activated by pro-inflammatory cytokines activate IKKβ to inhibit insulin signalling both under physiological and pathological conditions. Another IRS kinase, JNK, is also activated by proinflammatory cytokines such as TNFα, and its activity is abnormally elevated in obesity. Conversely, the absence of JNK1 results in decreased adiposity, significantly improved insulin sensitivity and enhanced IR signalling capacity in two different models of mouse obesity [33]. The inhibitory effects of JNK on insulin signalling can be attributed, at least partially, to its ability to phosphorylate Ser-307 of IRS-1 that uncouples it from the IR [34]. Glycogen synthase kinase-3 (GSK3) [35], casein kinase II [36] and a novel kinase that phosphorylates IRS-1 at Ser-789 [37] are additional potential IRS kinases. The Ser-789 kinase is presumably activated under conditions of insulin resistance, because increased phosphorylation of this site is observed in livers of insulin-resistant rodent models [37]. Hence a large number of Ser/Thr kinases can phosphorylate IRS proteins as a result of a stimulus initiated by inducers of insulin resistance. In summary, current findings implicate IRS proteins as major targets for insulin-induced, phosphorylation-based, negative-feedback control mechanisms that uncouple the IR from its downstream effectors and terminate insulin signalling under physiological conditions. The kinases involved are still under investigation, with current focus on PKCζ , IKKβ, JNK and mTOR as potential candidates. A variety of agents and conditions that induce insulin resistance, such as TNFα, FFAs and stress inducers, also activate IRS kinases. At present, different PKC isoforms, IKKβ, MAPK, JNK and mTOR appear to be potential candidates, but additional kinases are likely to emerge. Another question still unresolved is whether the same or different signalling pathways are being utilized by insulin or agents that induce resistance to regulate the activity of IRS kinases. Although the same kinases (PKCζ , JNK and IKKβ) can be activated by insulin, FFAs and TNFα, there is no evidence that these kinases are being activated along the same pathways by insulin or by inducers of insulin resistance. Because each of the potential IRS kinases has a unique substrate specificity, the question remains as to which Ser/Thr sites are being modified by each kinase and what are the consequences of such phosphorylation. Recent studies indicate that negative regulatory sites are found both in close proximity to the PTB domain (e.g. Ser-307) and at the C-terminal end of IRS-1 (e.g. Ser-612), and it still remains to be determined whether phosphorylation of Ser residues distributed along the IRS molecule contributes to a given functional change (e.g. enhanced dissociation of IR–IRS complexes), or whether phosphorylation of Ser residues clustered within a confined region results in a unique functional consequence. Given the large number of stimuli, pathways, kinases and potential sites involved, it appears that Ser/Thr phosphorylation of IRS proteins represents a combinatorial consequence of several kinases, activated by different pathways, acting in concert to phosphorylate multiple sites. Still, in spite of the complexity and dynamic of the system, unravelling IRS kinases and their biological role is an exciting opportunity to provide a novel viewpoint to the molecular basis for insulin resistance. This should enable rational drug design to selectively inhibit the activity of relevant kinases and generate a novel class of therapeutic agents for treatment of insulin resistance and Type II diabetes. References 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 LeRoith, D. and Zick, Y. (2001) Diabetes Care 24, 588–597 Zick, Y. (2001) Trends Cell Biol. 11, 437–441 Khan, A.H. and Pessin, J.E. (2002) Diabetologia 45, 1475–1483 Voliovitch, H., Schindler, D., Hadari, Y.R., Taylor, S.I., Accili, D. and Zick, Y. (1995) J. Biol. Chem. 270, 18083–18087 Wolf, G., Trüb, T., Ottinger, E., Groninga, L., Lynch, A., White, M.F., Miyazaki, M., Lee, J. and Shoelson, S.E. (1995) J. Biol. Chem. 270, 27407–27410 Cantley, L.C. (2002) Science 296, 1655–1657 Chiang, S.H., Baumann, C.A., Kanzaki, M., Thurmond, D.C., Watson, R.T., Neudauer, C.L., Macara, I.G., Pessin, J.E. and Saltiel, A.R. (2001) Nature (London) 410, 944–948 Inoue, M., Chang, L., Hwang, J., Chiang, S.H. and Saltiel, A.R. (2003) Nature (London) 422, 629–633 Paz, K., Hemi, R., LeRoith, R., Karasik, A., Elhanany, E., Kanety, H. and Zick, Y. (1997) J. Biol. Chem. 272, 29911–29918 Liu, Y.F., Paz, K., Herschkovitz, A., Alt, A., Tennenbaum, T., Sampson, S.R., Ohba, M., Kuroki, T., LeRoith, D. and Zick, Y. (2001) J. Biol. Chem. 276, 14459–14465 Paz, K., Yan-Fang, L., Shorer, H., Hemi, R., LeRoith, D., Quon, M., Kanety, H., Seger, R. and Zick, Y. (1999) J. Biol. Chem. 274, 28816–28822 Giraud, J., Leshan, R., Lee, Y.H. and White, M.F. (2004) J. Biol. Chem. 279, 3447–3454 Mothe, I. and Van Obberghen, E. (1996) J. Biol. Chem. 271, 11222–11227 Tirosh, A., Potashnik, R., Bashan, N. and Rudich, A. (1999) J. Biol. Chem. 274, 10595–10602 Pederson, T.M., Kramer, D.L. and Rondinone, C.M. (2001) Diabetes 50, 24–31 Hotamisligil, G.S., Peraldi, P., Budavari, A., Ellis, R., White, M.F. and Spiegelman, B.M. (1996) Science 271, 665–668 Li, J., DeFea, K. and Roth, R.A. (1999) J. Biol. Chem. 274, 9351–9356 Ravichandran, L.V., Esposito, D.L., Chen, J. and Quon, M.J. (2001) J. Biol. Chem. 276, 3543–3549 Neid, M., Datta, K., Stephan, S., Khanna, I., Pal, S., Shaw, L, White, M. and Mukhopadhyay, D. (2004) J. Biol. Chem. 279, 3941–3948 Moeschel, K., Beck, A., Weigert, C., Lammers, R., Kalbacher, H., Voelter, W., Schleicher, E.D., Haring, H.U. and Lehmann, R. (2004) J. Biol. Chem. 279, 25157–25163 Karin, M. (1999) J. Biol. Chem. 274, 27339–27342 Lallena, M.-J., Diaz-Meco, M.T., Bren, G., Paya, C.V. and Moscat, J. (1999) Mol. Cell. Biol. 19, 2180–2188 Gao, Z., Hwang, D., Bataille, F., Lefevre, M., York, D., Quon, M. and Ye, J. (2002) J. Biol. Chem. 277, 48115–48121 Lee, Y.-H., Giraud, J., Davis, R.J. and White, M.F. (2003) J. Biol. Chem. 278, 2896–2902 Kahn, B.B. and Flier, J.S. (2000) J. Clin. Invest. 106, 473–481 Kanety, H., Hemi, R., Papa, M.Z. and Karasik, A. (1996) J. Biol. Chem. 271, 9895–9897 Sanz, L., Sanchez, P., Lallena, M.J., Diaz, M.M. and Moscat, J. (1999) EMBO J. 18, 3044–3053 Yu, C., Chen, Y., Zong, H., Wang, Y., Bergeron, R., Kim, J.K., Cline, G.W., Cushman, S.W., Cooney, G.J., Atcheson, B. et al. (2002) J. Biol. Chem. 277, 50230–50236 De Fea, K. and Roth, R.A. (1997) J. Biol. Chem. 272, 31400–31406 C 2004 Biochemical Society 815 816 Biochemical Society Transactions (2004) Volume 32, part 5 30 Bouzakri, K., Roques, M., Gual, P., Espinosa, S., Guebre-Egziabher, F., Riou, J.P., Laville, M., Le Marchand-Brustel, Y., Tanti, J.F. and Vidal, H. (2003) Diabetes 52, 1319–1325 31 Yuan, M., Konstantopoulos, N., Lee, J., Hansen, L., Li, Z.-W., Karin, M. and Shoelson, S.E. (2001) Science 293, 1673–1677 32 Hundal, R.S., Petersen, K.F., Mayerson, A.B., Randhawa, P.S., Inzucchi, S., Shoelson, S.E. and Shulman, G.I. (2002) J. Clin. Invest. 109, 1321–1326 33 Hirosumi, J., Tuncman, G., Chang, L., Gorgun, C.Z., Uysal, K.T., Maeda, K., Karin, M. and Hotamisligil, G.S. (2002) Nature (London) 420, 333–336 C 2004 Biochemical Society 34 Aguirre, V., Uchida, T., Yenush, L., Davis, R. and White, M.F. (2000) J. Biol. Chem. 275, 9047–9054 35 Eldar-Finkelman, H. and Krebs, E.G. (1997) Proc. Natl. Acad. Sci. U.S.A. 94, 9660–9664 36 Tanasijevic, M.J., Myers, M.J., Thoma, R.S., Crimmins, D.L., White, M.F. and Sacks, D.B. (1993) J. Biol. Chem. 268, 18157–18166 37 Qiao, L.Y., Zhande, R., Jetton, T.L., Zhou, G. and Sun, X.J. (2002) J. Biol. Chem. 277, 26530–26539 Received 15 June 2004