* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Testing for Group A Streptococcal Pharyngitis
Survey
Document related concepts
Traveler's diarrhea wikipedia , lookup
Behçet's disease wikipedia , lookup
Infection control wikipedia , lookup
Kawasaki disease wikipedia , lookup
Germ theory of disease wikipedia , lookup
Signs and symptoms of Graves' disease wikipedia , lookup
Schistosomiasis wikipedia , lookup
Globalization and disease wikipedia , lookup
Management of multiple sclerosis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Childhood immunizations in the United States wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Multiple sclerosis research wikipedia , lookup
Multiple sclerosis signs and symptoms wikipedia , lookup
Transcript
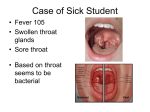
Testing for Group A Streptococcal Pharyngitis Sore throat is one of the most common complaints seen in any primary care setting. It is primarily a disease of school age children in the winter and spring. Most of these sore throats are viral but of those that are bacterial, group A streptococcus is the most common cause. [1] Strep can account for 15-30% of cases in pediatric patients but only 5-10% of cases in adults. [2] The rate is slightly higher in adults whose occupation brings them into frequent contact with children or those who are parents of school aged children. The most common complication of a strep infection is rheumatic fever. The rate of rheumatic fever in adults is extremely low. Other complications such as glomerulonephritis, or chorea are even rarer still. It is also clear that therapy can be postponed for up to 9 days after onset of symptoms and still be able to prevent sequela such as rheumatic fever. [3] Because of these facts, it is much less worrisome to miss a strep infection in an adult on the first presentation. The current rapid strep tests have a specificity of 95% which means the false positive rate is only 5%. [4] So any positive test should be treated and no further testing is needed. The sensitivity of the rapid tests ranges from 80% to 90% which means the false negative rate ranges from 10-20%. Given the above incidence of disease and complications and the long window of treatment opportunity in adults, it is sufficient to routinely only do a rapid test without a backup culture on patients who are symptomatic. © 2012 HealthPartners Our lab testing process for strep throat is changing. This particular testing procedure was looked at because sore throat is one of the most common complaints seen in all primary care settings and therefore generates many tests. Not even experts can distinguish a bacterial sore throat from a viral sore throat, especially in adults, based solely on history, symptoms and exam. National data also states that approximately 70% of patients presenting with sore throat receive antibiotics which means we are treating patients with unneeded antibiotics. [5] A laboratory confirmation of infection provides a way of determining who really needs the antibiotics without doing an extensive amount of testing. Proposed changes are based on national recommendations, accuracy of the rapid test, incidence of disease in different age groups, incidence of complications of disease in different age groups, and the cost of care. Our new testing protocol will be as follows: For all patients less than 21 years of age a back up culture will routinely continue to be done on anyone that has a rapid test done, whether ordered by a nurse or provider. There is no change in procedure for this age group. For those 21 years of age and over 21 years of age only rapid tests will be done unless there is a clinical reason to do a culture such as previous history of strep complications, symptoms with a known exposure, or an immunocompromised patient. These criteria will be clearly spelled out in the standing order for nurses to use. However this means that when a throat culture is indicated, it will need to be ordered separately for these patients. There are a few other things to keep in mind. Anyone who has been treated with antibiotics for strep within the past 2-3 weeks should only receive a throat culture because a rapid test is not accurate in those circumstances. Also a positive test does not distinguish those who are carriers from those who are infected. It is important to only test those that have symptoms to avoid treating those that are carriers and not infected. If someone has a negative rapid test and is symptomatic you may wish to retest them if symptoms such as fever (>101) persist for more than 3 days, or inability to swallow liquids, rash, swollen joints, or cola colored urine appear. These precautions are also spelled out in the standing orders the nurses use and in the patient education materials. With the new procedure we will be able to eliminate unnecessary testing and treat only those who have symptoms and positive tests and really need the antibiotics. This increases patient safety, reduces the chances of developing antibiotic resistance, and lowers the cost of care. References: 1. Practice Guidelines for the Diagnosis and Management of Group A Streptococcal Pharyngitis, Alan L Bisno, Michael A Gerber, Jack M. Gwaltnery, et al. Clinical Infectious Disease (2002) 35 (2): 113-125 http://cid.oxfordjournals.org/content/35/2/113.full © 2012 HealthPartners 2. Linder JA, Stafford RS, Antibiotic treatment of adults with sore throat by community primary care physicians. JAMA 2001;286:1181-6 3. Nyquist AC, Gonzales R, Steiner JF, Sane MA. Antibiotic prescribing for children with colds, upper respiratory tract infections, and bronchitis. JAMA 1998;279:875 4. Bisno AL. Acute Pharyngitis: etiology and diagnosis. Pediatrics 1996; 97:949-54 5. Poses RM, Cebul RD, Collins M, Fager SS. The accuracy of experienced physicians’ probability estimates for patients with sore throats: implications for decision making. JAMA 1985:254:925-9 6. Komaroff AL, Pass TM, Aronso MD et al. The prediction of streptococcal phyngitis in adults. J Gen Internal Medicine 1986:1:1-7 7. Bisno AL. Acute pharyngitis. New England Journal Medicine 2001;344:205-11 8. Cantazaro FJ, Stetson CA Morris AJ et al. the role of streptococcus in the pathogenesis of rheumatic fever. Am J Med 1954;17:749-56 9. Gerber MA. Comparison of throat cultures and rapid strep tests for diagnosis of streptococcal pharyngitis. Pediatric Infectious Disease Journal 1989; 8:820-4 Questions: Please reply to this e-mail, and your questions(s) will be directed to the author of this Pearl, R.L. Mitchell, M.D. Pearls of Knowledge Archive All Pearl recommendations are consistent with professional society guidelines, and reviewed by HealthPartners Physician Leadership. © 2012 HealthPartners