* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download The Road to a better infection control program
Microbicides for sexually transmitted diseases wikipedia , lookup
Chagas disease wikipedia , lookup
Tuberculosis wikipedia , lookup
Onchocerciasis wikipedia , lookup
Toxocariasis wikipedia , lookup
Neglected tropical diseases wikipedia , lookup
Herpes simplex virus wikipedia , lookup
Rocky Mountain spotted fever wikipedia , lookup
Henipavirus wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Toxoplasmosis wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Herpes simplex wikipedia , lookup
Cryptosporidiosis wikipedia , lookup
Hookworm infection wikipedia , lookup
West Nile fever wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Marburg virus disease wikipedia , lookup
Gastroenteritis wikipedia , lookup
Leptospirosis wikipedia , lookup
Anaerobic infection wikipedia , lookup
Hepatitis C wikipedia , lookup
Sarcocystis wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Trichinosis wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Hepatitis B wikipedia , lookup
Candidiasis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Schistosomiasis wikipedia , lookup
Lymphocytic choriomeningitis wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
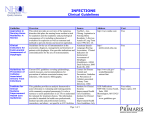
THE ROAD TO AN EFFECTIVE INFECTION PREVENTION PROGRAM PIN QI Showcase 2011 Linda Matranga, R.N. QI Director Infection Preventionist Safety Officer Asst. Dir. Public Health Clinical Information Systems Project Manager Federal LTC Survey on 2/25/2010 F441 F441 §483.65 Infection Control The facility must establish and maintain an Infection Control Program designed to provide a safe, sanitary and comfortable environment and to help prevent the development and transmission of disease and infection. §483.65(a) Infection Control Program The facility must establish an Infection Control Program under which it – (1) Investigates, controls, and prevents infections in the facility; (2) Decides what procedures, such as isolation, should be applied to an individual resident; and (3) Maintains a record of incidents and corrective actions related to infections. F441 §483.65(b) Preventing Spread of Infection (1) When the Infection Control Program determines that a resident needs isolation to prevent the spread of infection, the facility must isolate the resident. (2) The facility must prohibit employees with a communicable disease or infected skin lesions from direct contact with residents or their food, if direct contact will transmit the disease. (3) The facility must require staff to wash their hands after each direct resident contact for which hand washing is indicated by accepted professional practice. §483.65(c) Linens Personnel must handle, store, process and transport linens so as to prevent the spread of infection. WHAT THEY CITED “The facility failed to implement an infection control program through which all infections were tracked and preventative measures implemented. Additionally the facility failed to ensure that staff techniques during cares minimized the potential for cross contamination and the spread of infections.” WHAT THEY CITED Surveillance retrospective not concurrent Current tracking of infections did not show follow up or resolution Surveillance data inaccurate Surveillance data collection processes not dependable Surveillance data was incomplete WHAT THEY CITED Interventions not implemented appropriately Staff dressing change techniques Incorrect linen handling by CNA and Laundry staff Incorrect hand hygiene during feeding of residents Incorrect management of applesauce/pudding during med pass WHAT WE HAD No coordinated IC program Person responsible did not have the proper training Other departments not involved, dietary, clinic, housekeeping, etc. No IC Committee No provider involvement Only about 3 hours a month dedicated to IC specifically WHAT WE HAD Infections not followed up with appropriate interventions in a timely manner All staff did not understand isolation Isolation equipment and supplies not readily available WHAT DID WE NEED TO DO? Develop processes and policies for concurrent surveillance of infections Exam our policies and practice for infection prevention, isolation, dressing changes, pericare and others. Educate staff WHAT DID WE NEED TO DO? Involve all departments in IC Appreciate the need to invest more hours Examine the IC/IP role in our facility Infection Control Committee Provide education for IP OUR BIGGEST CHALLENGES Who would be the IP/IC? Divided the duties between the D.O.N. and the QI Director Developed processes and forms so that the DON could track infections on the floor The QI Dir. would get the education, manage the program and do the data. Work as a team. OUR BIGGEST CHALLENGES Infection Preventionist Education Joined APIC- $185, MT. APIC Chapter Dues $30-awesome price for what you get. Utilized the APIC website- huge resource for information and education Attended MT APIC Conference Attended the EPI 101 course in S.F. MT APIC Listserv- excellent networking with IPs around the state OUR BIGGEST CHALLENGES How can the IP know what infections are in the facility? Worked with lab staff to develop process to receive C&S and other reports. Worked with unit secretary to develop a process to get all antibiotic orders. Worked with nurses to notify IP of infections. Attachment A, Infection Control Program Policy Infection Control Program Data Sources and Surveillance Activities Staff nurses, clinical managers, employees & providers report residents and patients and employees of concern. Concurrent tracking and interventions documentation is maintained using the worksheet tool. Lab provides copies of positive cultures, unusual organisms, reportable diseases & other isolates of clinical significance. Staff nurses, clinical managers, employees & providers report employee illness of concern. Infection Control Preventionist (ICP) uses referred patient data to identify chart review needed to achieve surveillance strategies. Patients are placed in appropriate isolation and education provided to health care workers During surveillance rounds the ICP reviews each chart to determine whether the infection is healthcare associated or was acquired in the community using standard CDC/NHSN case definitions. Reportable Diseases as defined by MT State law are reported to Public Health in compliance with state law and HIPAA regulations (LTC, CAH, Hospice, ALF & Clinic staff report diseases within their department) Data is collected on healthcare-associated cases, as is appropriate depending on the type of infection identified Data is collected, trended, analyzed and reported for each specific area (LTC, CAH) using surveillance tools. The Infection Control Committee oversees the surveillance, investigation, reporting, control and prevention of infections; occupational exposures to blood, body fluids, or other potentially infectious materials; and monitoring for proper implementation of and adherence to infection control policies and procedures. Quarterly summary reports are given to Board of Directors, Medical Staff, QIC/QAA Committees, Clinical Managers and Directors. Infection Control Program Results to be sent to the Infection Preventionist, Linda Matranga, R.N. Who All patients and residents seen or cared for at the PMC W hat Microbiology Lab Results Smear, stain results (gram stain, AFB smear) Bacterial culture and sensitivity, parasitology AFB culture and sensitivity Virology Lab Results Immunology/titer results (hepatitis, HIV, chickenpox) Rapid tests (influenza, RSV, etc.) Viral cultures Where Please place copies in the “Confidential” folder in Linda Matranga’s mailbox in front office Note: Please notify the Charge Nurse or Infection Preventionist of any results indicating that an MDRO (MRSA, VRE, ESBLs) is present. Infection Control Worksheet CAH PO Box 1228, Big Timber, MT. 406-932-4603 Fax: 406-932-5468 (Acute, OBS, Swing Skilled, Swing Intermediate) Site Onset Date_________ Name:______________________________ Acute OBS Sw. Skilled Sw. Int. Age______ M F Room #________ Signs/Symptoms EENT GI Upper RT Lower RT Skin/ Soft tissue Urinary Tract Other: Provider Diagnosis UTI Conjunctivitis Site Name:______________________________ Acute OBS Sw. Skilled Sw. Int. Age______ M F Room #________ Signs/Symptoms EENT GI Upper RT Lower RT Skin/ Soft tissue Urinary Tract Other: Bronchitis Other: Site Name:______________________________ Acute OBS Sw. Skilled Sw. Int. Age______ M F Room #________ Signs/Symptoms EENT GI Upper RT Lower RT Skin/ Soft tissue Urinary Tract Other: Treatment Plan (include dates) HAI (Hospital Acquired) Community Acquired Outcome Provider Diagnosis UTI Culture Date__________ Pneumonia Conjunctivitis Culture Results: Cellulitis Bronchitis Other: Treatment Plan (include dates) Onset Date_________ Culture Results: Cellulitis Treatment Plan (include dates) Onset Date_________ Culture Date__________ Pneumonia HAI (Hospital Acquired) Community Acquired Outcome Provider Diagnosis UTI Culture Date__________ Pneumonia Conjunctivitis Culture Results: Cellulitis Bronchitis Other: HAI (Hospital Acquired) Community Acquired Outcome OUR BIGGEST CHALLENGES Staff Education and Involvement New policies Basic IC education for all nursing staff Increased “teaching moments” Emphasized importance and involvement You have a wound that starts to drain. It looks purulent. You expect an order for C&S and probably antibiotics. Or You have a resident/patient with new onset, frequent uncontrolled and uncontained diarrhea. You suspect C. Diff Or You suspect some other type of infection Make sure that infectious material is contained as much as possible. Place the resident/patient in the appropriate precautions. Get the signs out of the Infection Control Book. Get the right equipment up from the basement. Don’t wait for the culture or the results. The bug could be infecting others while you wait. “Isolation precautions” is a nursing decision. You can get that order later. Isolation precautions can be discontinued if not indicated by the culture results. It is better to be safe than sorry If you have questions, call Linda at ext #257 or her cell. 80% of PMC staff were immunized. Sheriff Matranga will be signing up the posse on Payday from 1300-1500 this Friday, 10/1. The Sheriff will also be making rounds at different times in October to rustle up any stragglers. Any posse hand that takes a “shot” at the villain will get their name put in the hat for a reward. There are three rewards, Wine and Cheese Picnic Backpack $40.00 PMC Grub ticket $25.00 Starbucks Card Nursing Guidelines for Symptomatic UTI Assessment and Intervention (LTC and Swing) Follow these guidelines in determining when to implement interventions for a suspected urinary tract infection. One of the following criteria must be met: 1. The resident has at least one of the following signs and symptoms: a. Fever (≥ 100.4) or chills, b. New or increased burning pain on urination, frequency or urgency, c. New flank or suprapubic pain or tenderness, d. Worsening of mental or functional status, (may be new or increased incontinence). Note: A change in the character of the urine alone does not meet the criteria. The resident must have at least one of the above symptoms also. 2. If the resident has at least one of the above symptoms; a) Document the findings and vital signs, b) Send a UA, and then a C&S as indicated by standing orders, c) Monitor VS and resident status Q Shift and document, d) Notify the provider of UA and C&S results, e) Obtain order for treatment as indicated. KEY IMPROVEMENTS An infection control program was implemented for all patients and residents which; investigates, controls, and prevents infections; decides what procedures, such as isolation should be applied to an individual resident; and maintains a record of incidents and corrective actions related to infections. Redefined the IP role and expanded hours for infection control and prevention Involved all departments in the IC Program KEY IMPROVEMENTS Provided IP with educational opportunities and support Implemented new processes with lab for notification of results Implemented improved Public Health Communication processes Involved medical staff via the IC committee and at Med Staff Meetings Updated all policies OTHER IMPROVEMENTS Provided staff with resources, guidelines, books, reference materials Improved “Sharps Injury” processes, policy, manager and staff education, forms and documentation Initiated process changes R/T Single use tourniquets Improved endoscopy cleaning procedures OTHER IMPROVEMENTS Initiated process changes R/T specimen transport Initiated process changes R/T how housekeepers refill disinfectant bottles Worked with providers to establish criteria for urine C&S orders OTHER IMPROVEMENTS Implemented new policy for Blood and Body Fluids Exposure and Follow Up Provided info, forms and process guidance for providers, managers and staff in the ER for any exposures. Implemented an aggressive but fun immunization program for staff Implemented employee illness tracking, new process and forms THE BOTTOM LINE Education Staff Involvement Teamwork Administrative Support MARCH 2011 LTC SURVEY Complimentary of the work we had done. Cited two issues, use of “Definitions of Infection for Surveillance” and Antibiotic Use Review. Definitions of Infection for Surveillance in Long-term Care Facilities Reference: Definitions of Infection for Surveillance in Long-term Care Facilities; Allison McGeer, Beverly Campbell, T. Grace Emori, Walter J. Hierholzer, Marguerite M. Jackson, Lindsay E. Nicolle, Carla Peppler, Amersolo Rivera, Debra G. Schollenberger, Andrew E. Simor, Philip W. Smith, and Elaine E-L. Wang Copyright 1996, APIC RESPIRATORY INFECTIONS Common cold syndromes/ pharyngitis The resident must have at least two of the following signs or symptoms: 1. runny nose or sneezing, 2. stuffy nose (i.e., congestion), 3. sore throat or hoarseness or difficulty in swallowing, 4. dry cough, 5. swollen or tender glands in the neck (cervical lymphadenopathy). Comment. Fever may or may not be present. Symptoms must be new, and care must be taken to ensure that they are not caused by allergies. Influenza-like illness Both of the following criteria must be met: 1. Fever (>100.4° F)* *A single temperature of .100.4°, taken at any site. 2. The resident must have at least three of the following signs or symptoms: a. chills, b. new headache or eye pain, c. myalgias, d. malaise or loss of appetite, e. sore throat, f. new or increased dry cough. Comment. This diagnosis can be made only during influenza season. If criteria for influenza-like illness and another upper or lower respiratory tract infection are met at the same time, only the diagnosis of influenza-like illness should be recorded. Pneumonia Both of the following criteria must be met: 1. Interpretation of a chest radiograph as demonstrating pneumonia, probable pneumonia, or the presence of an infiltrate. If a previous radiograph exists for comparison, the infiltrate should be new. 2. The resident must have at least two of the signs and symptoms described under ‘‘other lower respiratory tract infections.’’ Comment. Noninfectious causes of symptoms must be ruled out. In particular, congestive heart failure may produce symptoms and signs similar to those of respiratory infections. Other lower respiratory tract infection (bronchitis, tracheobronchitis) The resident must have at least three of the following signs or symptoms: 1. new or increased cough, 2. new or increased sputum production, (c) fever (>100.4), 3. pleuritic chest pain, 4. new or increased physical findings on chest examination (rales, rhonchi, wheezes, bronchial breathing), 5. one of the following indications of change in status or breathing difficulty: new/increased shortness of breath or respiratory rate .25 per minute or worsening mental or functional status.* (*Significant deterioration in the resident’s ability to carry out the activities of daily living or in the resident’s cognitive status, respectively.) Comment. This diagnosis can be made only if no chest film was obtained or if a radiograph failed to confirm the presence of pneumonia. URINARY TRACT INFECTIONS Urinary tract infection Urinary tract infection includes only symptomatic urinary tract infections. Surveillance for asymptomatic bacteriuria (defined as the presence of a positive urine culture in the absence of new signs and symptoms of urinary tract infection) is not recommended, as this represents baseline status for many residents. Symptomatic urinary tract infection One of the following criteria must be met: 1. The resident does not have an indwelling urinary catheter and has at least three of the following signs and symptoms: a. fever (>100.4° F) or chills, b. new or increased burning pain on urination, frequency or urgency, c. new flank or suprapubic pain or tenderness, d. change in character of urine, e. worsening of mental or functional status (may be new or increased incontinence). 2. The resident has an indwelling catheter and has at least two of the following signs or symptoms: a. fever (>100.4° F) or chills, b. new flank or suprapubic pain or tenderness, c. change in character of urine, d. worsening of mental or functional status. Comment. It should be noted that urine culture results are not included in the criteria. However, if an appropriately collected and processed urine specimen was sent and if the resident was not taking antibiotics at the time, then the culture must be reported as either positive or contaminated. Because the most common occult infectious source of fever in catheterized residents is the urinary tract, the combination of fever and worsening mental or functional status in such residents meets the criteria for a urinary tract infection. However, particular care should be taken to rule out other causes of these symptoms. If a catheterized resident with only fever and worsening mental or functional Change in character may be clinical (e.g., new bloody urine, foul smell, or amount of sediment) or as reported by the laboratory (new pyuria or microscopic hematuria). For laboratory changes, this means that a previous urinalysis must have been negative. McGeer Definitions of Infection for LTC EYE, EAR, NOSE, AND MOUTH INFECTION Conjunctivitis One of the following criteria must be met: 1. Pus appearing from one or both eyes, present for at least 24 hours. 2. New or increased conjunctival redness, with or without itching or pain, present for at least 24 hours (also known as ‘‘pink eye’’). Comment. Symptoms must not be due to allergy or trauma to the conjunctiva. Ear infection One of the following criteria must be met: 1. Diagnosis by a provider* of any ear infection. 2. New drainage from one or both ears. (Non-purulent drainage must be accompanied by additional symptoms, such as ear pain or redness.) *Requires a written note or a verbal report from a provider specifying the diagnosis. usually implies direct assessment of the resident by a provider. An antibiotic order alone does not fulfill this criterion. Mouth and perioral infection Oral and perioral infections, including oral candidiasis, must be diagnosed by a provider or a dentist. Sinusitis The diagnosis of sinusitis must be made by a pprovider. SKIN INFECTION Cellulitis/soft tissue/wound infection One of the following criteria must be met: 1. Pus present at a wound, skin, or soft tissue site. 2. The resident must have four or more of the following signs or symptoms: a. fever (>100.4) or worsening mental/functional status; and/or, at the affected site, the presence of new or increasing b. heat, c. redness, d. swelling, e. tenderness or pain, serous drainage. Fungal skin infection The resident must have both 1. a maculopapular rash and 2. either provider diagnosis or laboratory confirmation.† Herpes simplex and herpes zoster infection. For a diagnosis of cold sores or shingles, the resident must have both 1. a vesicular rash and 2. either provider diagnosis or laboratory confirmation. †For Candida or other yeast, laboratory confirmation includes positive smear for yeast or culture for Candida spp.; for herpetic infections, positive electron microscopy or culture of scraping or swab; for scabies, positive microscopic examination of scrapings. Scabies The resident must have both 1. a maculopapular and/or itching rash and 2. either provider diagnosis or laboratory confirmation. Comment. Care must be taken to ensure that a rash is not allergic or secondary to skin irritation. SYSTEMIC INFECTIOJN GI TRACT INFECTIONS Primary bloodstream infection One of the following criteria must be met: 1. Two or more blood cultures positive for the same organism. 2. A single blood culture documented with an organism thought not to be a contaminant and at least one of the following: a. fever (>/= 100.4), b. new hypothermia (<94.1° F, or does not register on the thermometer being used), c. a drop in systolic blood pressure of > 30 mm Hg from baseline, or d. worsening mental or functional status. Gastroenteritis One of the following criteria must be met: 1. Two or more loose or watery stools above what is normal for the resident within a 24-hour period. 2. Two or more episodes of vomiting in a 24-hour period. 3. Both of the following: a. a stool culture positive for a pathogen (Salmonella, Shigella, E. coli O157:H7, Campylobacter) or a toxin assay positive for C. difficile toxin and b. at least one symptom or sign compatible with gastrointestinal tract infection (nausea, vomiting, abdominal pain or tenderness, diarrhea). Comment. Bloodstream infections related to infection at another site are reported as secondary bloodstream infections and are not included as separate infections. Unexplained febrile episode The resident must have documentation in the medical record of fever (>/=100.4° F) on two or more occasions at least 12 hours apart in any 3-day period, with no known infectious or noninfectious cause. Comment. Care must be taken to rule out noninfectious causes of symptoms. For instance, new medications may cause both diarrhea and vomiting; vomiting may be associated with gallbladder disease. McGeer Definitions of Infection for LTC Principles: The definitions presented here are not all-inclusive. They focus on infections for which surveillance is expected to be useful (i.e., infections that are common and can be acquired and detected in the facility). Three important conditions apply to all of the definitions: 1. All symptoms must be new or acutely worse. Many residents have chronic symptoms, such as cough or urinary urgency, that are not associated with infection. However, a change in the resident’s status is an important indication that an infection may be developing. 2. Noninfectious causes of signs and symptoms should always be considered before a diagnosis of infection is made. 3. Identification of infection should not be based on a single piece of evidence. Microbiologic and radiologic findings should be used only to confirm clinical evidence of infection. Similarly, provider diagnosis should be accompanied by compatible signs and symptoms of infection. ANTIBIOTIC REVIEW Implement processes for antibiotic use review Opportunity for medical staff involvement Another learning moment THE ROAD AHEAD Growing emphasis nationally on the importance of infection prevention. PPS hospitals currently required to report certain infections. Trend toward mandatory reporting in other states. Will this be the future for CAH too? The Right Thing To Do. COLLABORATION BETWEEN AGENCIES MTDPHHS MHA MPQH Standardization of surveillance activities through use of NHSN and existing information systems Encourage use of NHSN for surveillance Enrolled all IPPS facilities into NHSN Evidence-Based Standardization of Practices isolation practices CUSP CAH MRSA Project Surgical Care Improvement Project MRSA Coaching All infection prevention and control activities CUSP Surgical Care Improvement Project MRSA Communication & Education Web Site IP Training HCW Training IP Listserv Mgmt PIN Liaison to CEO/CFO Advocacy IP Training Sharepoint site IP Listserv Hosting Surveillance THANK YOU QUESTIONS?