* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download HBHeartPhys
Survey
Document related concepts
Management of acute coronary syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Coronary artery disease wikipedia , lookup
Rheumatic fever wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Jatene procedure wikipedia , lookup
Artificial heart valve wikipedia , lookup
Electrocardiography wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
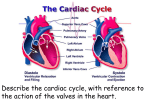
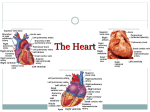
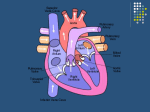
Transcript
Lecture: Cardiovascular System Includes the heart and blood vessels Brings nutrients to cells and helps get rid of wastes. Blood is refreshed in the lung, kidneys, intestine and liver. Lymphatic vessels help this system by collecting excess fluid surrounding tissues and return it to the cardiovascular system Functions: Generate blood pressure, Transport blood , Exchange of nutrients and wastes at the capillaries, Regulate blood flow as needed Main Path of Blood Flow: Heart – arteries – arterioles – capillaries - venules – veins – back to the heart… Types of Vessels: STUDY PICTURES IN TEXTBOOK. ● Arteries: Carry blood away from the heart to the capillaries. Their walls have 3 layers: (Thin inner epithelium, Thick smooth muscle layer, Outer connective tissue ● Veins: receive blood from the capillaries and return blood to the heart. Vein walls have 3 layers: (Thin inner epithelium, Thick smooth muscle layer, Outer connective tissue)Because they don't have pressure they have valves to keep blood flowing toward the heart ● Capillaries: Microscopic vessels between arterioles and venules. Made of one layer of epithelial tissue, Form beds of vessels where exchange with body cells occurs THE HEART: A large, muscular organ consisting of mostly cardiac tissue called the myocardium; It is surrounded by a sac called the pericardium (SERUS MEMBRANE); Consists of two sides, right and left, separated by a septum; Consists of 4 chambers: 2 atria and 2 ventricles; 2 sets of valves: semilunar valves and atrioventricular valves (AV valves). The valves give the resulting “lub” and “dup” sound of the heart. STUDY FIGURES IN BOOK. MAKE CERTAIN YOU CAN IDENTIFY 4 CHAMBER, VENA CAVA, PULMONARY ARTERY, PULMONARY VEIN , AORTA AND 4 VALVES. Cardiac Muscle called Myocardium. CHARACTERISTS fairly short, semi-spindle shape, branched, interconnected, connected (intercalated discs), electrical link (gap junction), 1 or 2 central nuclei, MANY mitochondria (25% space), almost all AEROBIC (oxygen) Two Circuits in System: 1. Pulmonary circuit: the right side of the body that brings blood from the body to the heart and the lungs 2. Systemic circuit: the left side of the heart that brings blood to the entire body to deliver nutrients and rid it of wastes Mechanism of Contraction of Contractile Cardiac Muscle Fibers 1. 2. Na+ influx from extracellular space, causes depolarizes (-90 to +30); Depolarization causes release of Ca++ from sarcoplasmic reticulum (as in skeletal muscle), allowing sliding actin and myosin to proceed. 3.. Gap junctions allow all cardiac muscle cells to be linked electrochemically, so that activation of a small group of cells spreads like a wave throughout the entire heart. This is essential for "synchronistic" contraction of the heart as opposed to skeletal muscle. Internal Conduction (Stimulation) System of the Heart 1. heart can beat rhythmically without nervous input. Automicity (Autorhythmicity) - some cardiac muscle cells are "self-excitable" allowing for rhythmic waves of contraction to adjacent cells throughout the heart. Skeletal muscle cells must be stimulated by independent motor neurons as part of a motor unit. 2. gap junctions - electrically couple all cardiac muscle cells so that depolarization sweeps across heart in sequential fashion from atria to ventricles 3. "Pacemaker" Features of Autorhythmic Cells "autorhythmic cells" of heart muscle create action potentials in rhythmic fashion; this is due to unstable resting potentials which slowly drift back toward threshold voltage after repolarization from a previous cycle. Theoretical Mechanism of Pacemaker Potential: begins with a ends with d returns to a a. K+ leak channels allow K+ OUT of the cell more slowly than in skeletal muscle b. Na+ slowly leaks into cell, causing membrane potential to slowly drift up to the threshold to trigger Ca ++ influx from outside (-40 mv) c. when threshold for voltage-gated Ca++ channels is reached (-40 mv), fast calcium channels open, permitting explosive entry of Ca++ from of the cell, causing sharp rise in level of depolarization d. when peak depolarization is achieved, voltage-gated K+ channels open, causing repolarization to the "unstable resting potential" Sequence of Excitation of the Heart:.& Order of Impulses Sinoatrial node (SA) is located in the right atrium -> (right AV valve) atrioventricular node (AV) -> (bundle of His) ->right & left bundle of His branches -> Purkinje fibers of ventricular walls . Special Considerations of Wave of Excitation 1. initial SA node excitation causes contraction of both the R and L atria 2. contraction of R and L ventricles begins at APEX of heart (inferior point), ejecting blood superiorly to aorta and pulmonary artery 3. arrhythmias - uncoordinated heart contractions 4. fibrillation - rapid and irregular contractions of the heart chambers; reduces efficiency of heart Electrocardiography: Electrical Activity of the Heart :Deflection Waves of ECG 1. P wave - initial wave, demonstrates the depolarization from SA Node through both ATRIA; the ATRIA contract about 0.1 s after start of P Wave 2. QRS complex - next series of deflections, demonstrates the depolarization of AV node through both ventricles; the ventricles contract throughout the period of the QRS complex, with a short delay after the end of atrial contraction; repolarization of atria also obscured 3. T Wave - repolarization of the ventricles (0.16 s) The Normal Cardiac Cycle 1. systole - period of ventricular contraction 2. diastole - period of ventricular relaxation Events of Cardiac Cycle: Remember that the 2 Atria contract together and the two ventricles contract together TOTAL CARDIAC CYCLE TIME = 0.8 second PULSE: (normal 70 beats/minute) * blood flows from vena cavas/pulmonary vein INTO atria * blood flows through AV valves INTO ventricles * atrial contraction propels blood to ventricles * filled ventricles begin to contract, AV valves CLOSE * contraction of closed ventricles increases pressure * ventricular contraction - blood forced out * semilunar valves open, blood exits aorta & pulmonary trunk Heart Sounds: Stethoscope Listening 1. 2. 3. lub-dub, - , lub,dub, lub - closure of AV valves, onset of ventricular systole dub- closure of SL valves tricuspid and bicuspid valve rt and lt AV valves respectively mitral valve (lub) - LT 5th intercostal, lateral Heart Murmurs - sounds other than the typical "lub-dub"; typically caused leaking valves Cardiac Output - Blood Pumping of the Heart A. General Variables of Cardiac Output 1. Cardiac Output (CO) - blood amount pumped per minute 2. Stroke Volume (SV) - ventricle blood pumped per min. 3. Heart Rate (HR) - cardiac cycles per minute CO (ml/min) = HR (beats/min) X SV (ml/beat) normal CO = 75 beats/min X 70 ml/beat = 5.25 L/min Critical factor for stroke volume is "degree of stretch of cardiac muscle cells"; more stretch = more contraction force a) slow heart rate = more time to fill b) exercise = more venous blood return Regulation of Heart Rate (Autonomic, Chemical, Other) a. sympathetic - NOREPINEPHRINE (NE) increases heart rate (maintains Stroke Volume) b. parasympathetic - ACETYLCHOLINE (ACh) decreases heart rate c. vagal tone - parasympathetic inhibition of inherent rate of SA node, allowing normal HR d. baroreceptors, pressoreceptors - monitor changes in blood pressure and allow reflex activity with the autonomic nervous system Hormonal and Chemical Regulation of Heart Rate (HR) a. epinephrine - hormone released by adrenal medulla during stress; increases heart rate b. thyroxine - hormone released by thryroid; increases heart rate in large quantities; amplifies effect of epinephrine c. Ca++, K+, and Na+ levels very important; HIGH Na+ or increased K+ level; can block Na+ transport & muscle contraction. KCl used to stop heart on lethal injection LOW Ca - depresses heart function TACHYCARDIA - HIGHER than normal resting heart rate (over 100); may lead to fibrillation BRADYCARDIA - LOWER than normal resting heart rate (below 60); parasympathetic drug side effects; physical conditioning; sign of pathology in non-healthy patient Other Factors Effecting Heart Rate (HR) a. Age and gender normal heart rate - fetus 140-160 beats/minute; female 72- 80 beats/minute; male 64- 72 beats/minute b. exercise - lowers resting heart rate (40-60) c. heat - increases heart rate significantly d. cold - decreases heart rate significantly Imbalance of Cardiac Output & Heart Pathologies 1. 2. 3. 4. 5. 6. 7. congestive heart failure - heart cannot pump sufficiently to meet needs of the body Atherosclerosis - lOcclusion of heart vessels with plaque (fatty (LDL) and salts, reducing oxygen and nutrient supply to cardiac muscle cells; (fat & salt diet, smoking, stress) Hypertensionhigh blood pressure - when aortic pressure gets to large, left ventricle cannot pump properly, increasing ESV, and lowering SV myocardial infarct (MI) - "heart cell death" due to numerous factors, including coronary artery occlusion congenital heart defects - heart problems that are present at the time of birth sclerosis of AV valves - fatty deposits on valves; particularly the mitral valve of LEFT side; leads to heart murmur arrhythmias: abnormal rhythms tachycardia, bradycardia, fibrillation