* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download CHAPTER 19: HEART
Survey
Document related concepts
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Electrocardiography wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Artificial heart valve wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Transcript
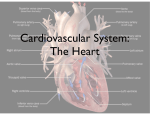
CHAPTER 19: HEART 1. OVERVIEW OF CARDIOVASCULAR SYSTEM cardiovascular system: heart and blood vessels circulatory system: heart, blood vessels, and blood cardiology : scientific study of the heart and the treatment of its disorders Major divisions of circulatory system pulmonary circuit - right side of heart o carries blood to lungs for gas exchange and back to heart systemic circuit - left side of heart o supplies oxygenated blood to all tissues of the body and returns it to the heart Cardiovascular System Circuit left side of heart o fully oxygenated blood arrives from lungs via pulmonary veins o blood sent to all organs of the body via aorta right side of heart o lesser oxygenated blood arrives from inferior and superior vena cava o blood sent to lungs via pulmonary trunk 2. GROSS ANATOMY OF THE HEART Heart Position heart located in mediastinum (middle section of chest cavity) between lungs 2/3 lies left of center Heart Size and Shape base – wide, superior portion of heart, blood vessels attach here apex - inferior end, tilts to the left, tapers to point 3.5 in. wide at base, 5 in. from base to apex and 2.5 in. anterior to posterior; weighs 10 oz. Pericardium double-walled sac that encloses the heart allows heart to beat without friction anchored to diaphragm inferiorly and sternum anteriorly Pericardial sac o Has 2 layers: fibrous and serous o pericardial cavity - space inside the pericardial sac filled with 5 - 30 mL of pericardial fluid pericarditis – inflammation of the membranes o painful friction rub with each heartbeat Heart Wall has 3 layers Epicardium o serous membrane covering heart o serous lining of sac turns inward at base of heart to cover the heart surface o adipose in thick layer in some places o coronary blood vessels travel through this layer endocardium o smooth inner lining of heart and blood vessels o covers the valve surfaces and continuous with endothelium of blood vessels myocardium o cardiac muscle proportional to work load o muscle spirals around heart to produce wringing motion o fibrous skeleton o structural support and attachment for cardiac muscle and anchor for valve tissue o electrical insulation between atria and ventricles 4 Heart Chambers Right and left atria on top o two superior chambers o receive blood returning to heart o Auricles: Each atrium has small earlike extension that increases volume Right and left ventricles on bottom o two inferior chambers o pump blood into arteries o Trabeculae carneae (“fleshy beams”) rounded or irregular muscular columns which project from inner surface of the ventricle Sulci o Boundaries of chambers marked on surface by 3 sulci o Coronary Sulcus o 2 Interventricular Sulci Heart Valves Four valves ensure a one-way flow of blood through the heart atrioventricular (AV) valves – control blood flow between atria and ventricles o chordae tendineae - connect AV valves to papillary muscles on floor of ventricles o prevent AV valves from flipping inside out or bulging into the atria when the ventricles contract; Don’t open/close valves (force of blood opens them) o right AV valve has 3 cusps (tricuspid valve) o left AV valve has 2 cusps (mitral or bicuspid valve) o You always “tri” to do the “right” thing o L.A.B. R.A.T. = Left Atrium: bicuspid Right Atrium: tricuspid Semi-lunar Valves o aortic semilunar valve in opening between left ventricle and aorta o pulmonary semilunar valve in opening between right ventricle and pulmonary artery 3. PATH OF BLOOD THROUGH THE HEART AND CORONARY CIRCULATION The path of blood through the heart Systole = contraction of ventricles o Blood is going “into the SYStem” Diastole = relaxation of ventricles o If your heart is permanently relaxed you “Die” 1. Blood enters right atrium via superior and inferior vena cavae 2. Blood in right atrium flows through right AV valve into right ventricle 3. Contraction of right ventricle forces pulmonary valve open 4. Blood flows through pulmonary valve into pulmonary trunk 5. Blood is distributed by right and left pulmonary arteries to the lungs where it exchanges CO2 for O2 6. Blood returns from lungs via pulmonary veins to the left atrium 7. Blood in left atrium flows through left AV valve into left ventricle 8. Contraction of left ventricle forces aortic valve open 9. Blood flows through aortic valve into ascending aorta 10. Blood in aorta is distributed to the whole body through the arteries, arterioles, and capillaries Then comes back to heart via the veins to start all over again Valve Mechanics ventricles relax (diastole) o pressure drops inside the ventricles o semilunar valves close as blood attempts to back up into the ventricles from the vessels o AV valves open o blood flows from atria to ventricles ventricles contract (systole) o AV valves close as blood attempts to back up into the atria o pressure rises inside of the ventricles o semilunar valves open and blood flows into great vessels Try Pulling My Aorta o (Tricuspid, Pulmonary, Mitral, Aortic) Coronary Circulation: The heart providing itself with blood 5% of body’s blood goes to heart 250 ml of blood per minute needs abundant O2 and nutrients Coronary Arteries Location of coronary blood vessels can vary from person to person left coronary artery (LCA) o branches off the ascending aorta o o Through coronary sulcus under left auricle 2 branches anterior interventricular branch circumflex branch right coronary artery (RCA) o supplies right atrium and sinoatrial node (pacemaker) o Along sulcus, under right auricle o 2 branches Coronary Blood Flow blood flow to the heart muscle during ventricular contraction (systole) is slowed, unlike the rest of the body o coronary arteries compressed o opening of the aortic valve covers openings to coronary arteries o blood flow to the myocardium increases during ventricular relaxation during ventricular diastole, blood in the aorta surges back toward the heart and into the openings of the coronary arteries Venous Drainage of Heart 5 -10% drains directly into right atrium and right ventricle by way of the small thebesian veins the rest returns to right atrium through the coronary sinus by the following routes: great cardiac vein o travels along side of anterior interventricular artery o collects blood from anterior portion of heart middle cardiac vein (posterior interventricular) o found in posterior sulcus o collects blood from posterior portion of heart left marginal vein o Travels from near apex up left margin All drain into the coronary sinus o large transverse vein in coronary sulcus on posterior side of heart o collects blood and empties into right atrium What happens when coronary blood flow is interrupted? Infarct = area of tissue death due to lack of oxygen Cardiac cells deprived of oxygen die within minutes (some protection provided by arterial anastomoses which provide alternative route of blood flow within the myocardium) Acute Coronary Syndrome (ACS) Angina (chest pain) Acute Angina (extreme chest pain) Myocardial Infarction (Heart attack) Once a rare illness, now causes half of deaths in US o 1930’s: 3,000 per year o 1950’s: 500,000 per year o 2006: 8,500,000 Heart attacks; 10,200,000 Angina Symptoms of Heart Attack o P.U.L.S.E. o Persistent chest pain o Upset stomach o Lightheadedness o Short of breath o Excessive sweating o some painless heart attacks may disrupt electrical conduction pathways, lead to fibrillation and cardiac arrest o silent heart attacks occur in diabetics & elderly Conventional Theory: Heart Attack Proposed in 1940s, quickly accepted Atherosclerosis is condition of fatty deposits blocking arteries inflammation transforms atheroma into a hardened complicated plaque called arteriosclerosis In times of stress, decreased blood flow causes pain (angina) Eventually, cardiac muscle downstream of the blockage dies blood clot can also block artery In 1950, Ansel Keys proposed cholesterol in bloodstream to be the cause Prevention and Treatment coronary bypass surgery balloon angioplasty laser angioplasty Recommended prevention: Low-fat, low cholesterol diet and exercise BUT… If plaque also builds up in all your other arteries, why is there no such thing as a “kidney attack” or a “liver attack” or a “spleen attack”? Why do many heart attack victims have little to no blockage? 20 year study showed that 1000s of surgeries to bypass blocked arteries did not improve the chances of patient survival Saturated fat consumption in US has decreased drastically since 1930’s Myogenic Theory of Heart Attack (Unconventional--Not in text book!) Stress, diabetes, smoking , nutritional deficiencies cause disease in the capillaries and arterioles Heart cells receive inadequate oxygen and nutrients Condition increases under stressful conditions. Heart cells revert to their backup system--anaerobic fermentation for energy generation Produces lactic acid, stimulating pain Acidosis eventually kills heart cells Inflammatory debris collects, appears as “blockage” What is in the “inflammatory debris?” Cholesterol! Could cholesterol be a “repair substance” your body sends in to help heal diseased heart tissue? To read more… www.wapf.org 4. CARDIAC CONDUCTION SYSTEM AND CARDIAC MUSCLE Structure of Cardiac Muscle cardiocytes – heart cells; striated, short, thick, branched cells, one central nucleus surrounded by light staining mass of glycogen Intercalated Discs—between cells o 3 structures not found in skeletal muscle: Interdigitating folds Mechanical junctions Two types: o Fascia adherens: Broad ribbon-like band linking cells together with proteins o Desmosomes : Like snaps—each cell has half Electrical junctions: called gap junctions Repair of damage o Skeletal: dead muscle fibers replaced o Cardiac: repair by scarring Metabolism of Cardiac Muscle cardiac muscle depends on aerobic respiration used to make ATP rich in myoglobin and glycogen huge mitochondria – fill 25% of cell adaptable to organic fuels used fatty acids (60%), glucose (35%), ketones, lactic acid and amino acids (5%) more vulnerable to oxygen deficiency than lack of a specific fuel Cardiac Conduction System coordinates the heartbeat composed of an internal pacemaker and nervelike conduction pathways through myocardium generates and conducts rhythmic electrical signals signals pass from cell to cell through gap junctions 4 main components o sinoatrial (SA) node in right atrium near base of superior vena cava generates impulses faster than other cardiac cells, thus is pacemaker for entire heart (60-100 bpm) signals spread throughout atria SA node is modified muscle cell but does not contract o atrioventricular (AV) node located near the right AV valve at lower end of interatrial septum electrical gateway to the ventricles fibrous skeleton acts as an insulator to prevent currents from getting to the ventricles from any other route o atrioventricular (AV) bundle (bundle of His) bundle forks into right and left bundle branches o 1. 2. 3. 4. 5. these branches pass through interventricular septum toward apex Purkinje fibers nervelike extensions spread throughout ventricular myocardium SA node fires Excitation spreads through atria AV node fires Excitation spreads down AV bundle Excitation spreads through ventricles via Purkinje fibers Nerve Supply to Heart Heart has its own rhythm BUT is modified by input from nervous system sympathetic nerves (raise heart rate) o Fight or Flight o Remember: “You can SYMPATHIZE with someone’s fight or flight instincts” o Nerve fibers terminate in various parts of heart o increase heart rate and contraction strength o dilate coronary arteries to increase myocardial blood flow parasympathetic nerves (slow heart rate) o o o o Rest and Digest Remember: “When you are PARAlyzed you don’t move much” reduces the heart rate Can stop heart for a few seconds Nerves from heart to CNS o Afferent fibers transmit pain signals from heart 5. ELECTRICAL AND CONTRACTILE ACTIVITY OF THE HEART Cardiac Rhythm sinus rhythm - normal heartbeat triggered by the SA node o set by SA node at 60 – 100 bpm arrhythmia – any abnormal cardiac rhythm o Multiple types, different causes Abnormal Heart Rhythms (arrhythmias) ectopic focus – o part of heart that fires before SA node o caused by hypoxia, electrolyte imbalance, or caffeine, nicotine, and other drugs nodal rhythm o if SA node is damaged, heart rate is set by AV node, o 40 – 50 bpm intrinsic ventricular rhythm o if both SA and AV nodes are not functioning o 20 – 40 bpm o requires artificial pacemaker to sustain life Fibrillation o Atrial or ventricular o ventricular fibrillation serious arrhythmia caused by electrical signals reaching different regions at widely different times heart can’t pump blood kills quickly if not stopped o defibrillation - strong electrical shock to reset SA nodes to sinus rhythm First performed in US by Claude Beck in 1947 on a 14 year old boy “Hearts are too good to die” Pacemaker (SA node) Physiology Membrane potential difference in charged particles between inside and outside of cell K+, Na+, Ca++, Cl Pacemaker does not have stable membrane potential, because Na+ always slowing coming in when reaches threshold of -40 mV, voltage-gated fast channels open, let in Ca2+ and more Na+ faster depolarization occurs, peaking at 0 mV Depolarization change in a cell's membrane potential, making it more positive Negative ions going out or positive ions coming in gradual depolarization of SA node is called pacemaker potential After depolarization, K+ channels then open and K+ leaves the cell causing repolarization (SA node is negative again) once K+ channels close, pacemaker potential starts over Electrical Signal Through Heart signal from SA node stimulates two atria to contract almost simultaneously signal slows down through AV node thin cardiocytes have fewer gap junctions; delays signal 100 msec which allows the ventricles to fill signals travel very quickly through AV bundle and Purkinje fibers Ventricles contract in near unison papillary muscles contract an instant earlier than the rest, tightening slack in chordae tendineae ventricular systole progresses up from the apex of the heart spiral arrangement of cardiocytes twists ventricles slightly, like someone wringing out a towel Electrical Behavior of Myocardium cardiocytes (heart cells) have a stable resting potential of -90 mV depolarize only when stimulated depolarization phase (very brief) o voltage regulated Na+ gates open, Na+ rushes in o action potential peaks at +30 mV o Na+ gates close quickly plateau phase o hold and squeeze for 200 - 250 msec, o Ca2+ channels open and close slowly repolarization phase o Ca2+ channels close, K+ channels open, rapid diffusion of K+ out of cell returns it to resting potential Electrocardiogram (ECG or EKG) composite of all action potentials of nodal and myocardial cells detected, amplified and recorded by electrodes on arms, legs and chest diagnoses o abnormalities in conduction pathways o myocardial infarction o nodal damage o heart enlargement o electrolyte and hormone imbalances Cardiac Cycle: one complete contraction and relaxation of all four chambers of the heart atrial systole (contraction) occurs while ventricles are in diastole (relaxation) atrial diastole occurs while ventricles in systole quiescent period all four chambers relaxed at same time Auscultation—listening to sounds made by the body 4 Phases of Cardiac Cycle o all the events in the cardiac cycle are completed in less than one second! o ventricular filling during diastole, ventricles expand pressure drops, AV valves open, blood enters Filling the ventricles occurs in three phases: rapid ventricular filling o blood enters very quickly Diastasis o slower filling atrial systole o atria contract o isovolumetric contraction S1 at beginning of phase Tensing of ventricles, blood against AV valves, heart against chest? atria repolarize, relax for rest of cycle ventricles depolarize, begin to contract AV valves close ‘isovolumetric’ because ventricles contract but do not eject blood because pressure in the aorta and pulmonary trunk still greater than in the ventricles all four valves closed, blood cannot go anywhere o o ventricular ejection semilunar valves open blood spurts out of each ventricle rapidly at first – rapid ejection then more slowly under reduced pressure – reduced ejection lasts about 200 – 250 msec corresponds to the plateau phase of the cardiac action potential isovolumetric relaxation S2 during this phase blood rebounds from the closed semilunar valves, ventricles expand, relax Ventricles begin to relax (diastole) blood from the aorta and pulmonary briefly flows backwards filling the semilunar valves and closing the cusps ‘isovolumetric’ because semilunar valves are closed and AV valves have not yet opened ventricles are therefore taking in no blood Timing of Cardiac Cycle in a resting person atrial systole = 0.1 sec ventricular systole = 0.3 sec quiescent period = 0.4 sec total = 0.8 sec in a heart beating 75 bpm 6. CARDIAC OUTPUT Heart Rate pulse – surge of pressure produced by each heart beat that can be felt by palpating a superficial artery with the fingertips o infants: 120 bpm or more o young adult females 72 - 80 bpm o young adult males 64 to 72 bpm o heart rate rises again in the elderly tachycardia - resting adult heart rate above 100 bpm o stress, anxiety, drugs, heart disease, fever o loss of blood or damage to myocardium bradycardia - resting adult heart rate less than 60 bpm o in sleep, hypothermia, and endurance trained athletes