* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Self management Tools - Community Health Association of
Survey
Document related concepts
Food studies wikipedia , lookup
Cigarette smoking for weight loss wikipedia , lookup
Diet-induced obesity model wikipedia , lookup
Obesity and the environment wikipedia , lookup
Human nutrition wikipedia , lookup
Low-carbohydrate diet wikipedia , lookup
Food and drink prohibitions wikipedia , lookup
Gastric bypass surgery wikipedia , lookup
Childhood obesity in Australia wikipedia , lookup
Transcript
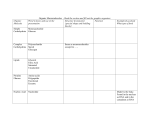
HEART HEALTH, DIABETES, WEIGHT MANAGEMENT, HYPERTENSION, STROKE AND EXERCISE MATERIALS AVAILABLE FROM Community Health Centers of Arkansas, Inc. : http://chcasvr2.chc-ar.org/Services/Services.htm Self-Management Materials Focus areas: heart health, diabetes, weight management, hypertension, stroke and exercise. These materials were developed to provide information in a low literacy format. They have colorful, multi-ethnic pictures with clear script. 5 of the handouts have a teachers guide to them Carbohydrate counting placemats: The basis for these came from the Idaho plate method. This is where a plate is divided into sections with each section that represents a certain food group. The sections have been filled in with an illustration of the appropriate food. One sector of the plate has been dedicated to the carbohydrate containing foods. This highlighted sector has also a simple list of the carbohydrate foods with portion sizes indicated for one serving. Each carbohydrate serving on the placemat is roughly equal to 15 grams of carbohydrates. This provides the patient with choice between the fruit, milk and starch groups, interchangeably. On the backside of the placemat is information on heart healthy eating and exercise. The intent is for the diabetic to be able to come to the table and not only have an example to compare his/her plate to, but to have some basic information needed to count carbohydrates which is the basic first level of diabetes diet control. Introduction to Carbohydrate counting The recommended amount of carbohydrates is 55% of calories Example: 1800 calories x .55 % of calories as carbohydrates = 990 calories from carbohydrates Each gram of carbohydrate has 4 calories 990 calories from carbohydrates 4 calories in each gram of carbohydrate =248 grams of carbohydrates Each serving of carbohydrate is = 15 grams: 248 grams of carbohydrates 15 grams of carbohydrates per serving: = 16.5 servings of carbohydrate per day subtract 1 serving from the total amount. This accounts for the carbohydrates attributed to all of the non starchy vegetables through the day. We now have 16.5 – 1= 15.5 servings for one day Spread these servings into 3 meals and some snacks: Women: approx 3-4 servings at a meal and 1-2 at a snack, Men: approx 5-6 servings at a meal and 1-2 for a snack What you end up with for 1800 calories and 240 grams of carbohydrate is something like this: Breakfast Total Carbohydrate servings: Starch Fruit Milk (4) 2 1 1 Snack Lunch Snack (4) 3 1 (1) 1 Dinner Snack Totals (4) 3 1 (15) 10 3 2 (2) 1 1 The patient as long as he stays within the total carbohydrate amount, can use the designated serving sizes interchangeably. For example, one day he wants to have pancakes. He can choose to have 3 small pancakes and 1 glass of milk, as long as all of his servings add up to the total carbohydrate number of servings for that meal. The other groups of meat, vegetables and fats are used with the following guidelines to make up the balance of the calories: MEATS: Meat portions are recommended to be no more than the size of a deck of cards, or the palm of your hand, trying to limit them to 2-3 times a day. Cottage cheese or tuna is 1/2 – ¾ cup for a serving Peanut butter is 2 tablespoons VEGETABLES: NON-STARCHY vegetables are recommended at the minimum to make up the balance of the recommended 5 servings for fruits or vegetables a day. In the table above, there are 3 fruit servings, therefore a minimum of 2 additional non starchy vegetables is recommended. Encouragement to use these more freely, especially salads: raw leafy greens, sprouts, radishes, mushrooms, cucumbers, etc., is very beneficial and should not be limited unless there is an effect on blood sugar. FATS: Fats are recommended in the liquid form or one that is very soft at room temperature Solid fats are discouraged. A serving of fat is 5 grams. This is approximately a teaspoon of oil or margarine, a tablespoon of diet margarine, or one tablespoon of salad dressing. 1-2 servings of fat per meal is recommended (including oil or fat used in cooking.) Fat free items are deceptive because in place of the fat, most of the time, starchy fillers and additional sugars are used. Check the label for total carbohydrates, not grams of fat. Fats also have a beneficial effect when combined with carbohydrates, in keeping the blood sugar lower. LABEL READING: Use labels to figure portion sizes based on 15 grams of carbohydrates per serving. If a food has 25 grams of total carbohydrate, for a serving of ½ cup, then ½ cup of this food is nearly 2 servings of carbohydrate. Do not direct your patients to look at “sugar” on the label, this is only a part of the Total carbohydrates, always calculate from the total carbohydrates amount. Having a snack or lunch during diabetes education class can be very instructive. Each person using their carbohydrate numbers can figure out how much they need to serve themselves of each food. Bring the food labels of any prepared foods you use. Use the placemat in class, and have them look up their portions on the mat. If you don’t have actual food, plan a sample lunch using the placemat to fill in appropriate foods they like. As much as you can, let them apply their knowledge in real life situations with the labels, serving food, or handling food models to estimate portion sizes. Because the table is abstract, practical experiences help to make it more real before they get home and try to make sense of it. This is diabetes diet information that nurses, pharmacists, and other health professionals working on getting their Diabetes Educator certification (CDE) would learn. It falls under first level management of diabetics. ANY patients with multiple medical problems including: renal or pulmonary insufficiency, large fluid shifts, or those whose blood sugars, weight, hypertension, or other labs specifically related to intake are continually abnormal, should be sent to a dietitian for further counseling. For non-dietitians counseling on diet related matters, charting should state that general principles of carbohydrate counting were covered. The following is a sample of one of the teacher’s guides for the weight loss handout. The handout is a page with 6 sections on it. See web site for actual handout. Each sector has an illustration and the following captions: 1. How can I lose weight? 2. Eat only when you are hungry 3. Stop before you are too full 4. Eat slowly, take a minimum of 20 minutes to eat a meal 5. Always eat at the table, not in the car and not in front of the T.V. 6. Write down all you eat and drink for 3 days. Teacher’s guide for You CAN Lose Weight (This is not a patient hand out). Weight loss is a very difficult thing to do, especially if you are going about it in an “unnatural” way. Eating a very limited diet, restricting or skipping meals and ignoring hunger is counterproductive. Restrictive diets lead to overeating. The information in this hand out is based on the idea called intuitive eating. It emphasizes the whole concept of eating appropriately, eliminating overeating and avoiding a “restrictive” mentality to weight management. Along with these ideas is the fundamentally healthy eating approach, but the ideas of “good” and “bad” foods are not stressed. Becoming aware of when you are hungry and not overeating is a part of respecting your body and taking care of yourself. It is the ultimate self-management. The patient needs to become aware of his/her life practices that affect his/her weight. Much of the eating people do is NOT related to hunger. Non-hunger related eating can be a result of stressful life situations, boredom, anger, depression, feeling out of control, feeling isolated, eating to reward oneself, or just plain habits of eating in certain situations like in front of the television, or eating by the clock, instead of by your hunger cues. 1. Eating only when hungry requires a certain amount of attentiveness and reducing distractions. Also skipping meals habitually or NOT eating when hungry can contribute to overeating later. Having a FOOD LOG is a very important tool to assess when and where eating is taking place. 2. Stopping before you are too full. There are 4 stages of hunger satiation: 1. hungry 2. not hungry 3. satisfied 4. full (overly) The patient should practice” tuning in” to these stages. Eating past satisfied can be a habit. 3. Eat slowly. Each meal should take at least 20 minutes. Only in eating slowly can the message of being satisfied make it from the stomach to the brain before overeating takes place. Eating slowly also gives more time to enjoy the food. 4. Eat while at the table, not in the car or in front of the television. Eating at the table promotes normal weight in children as well as supports all of the above mentioned ideas about “tuning in” to the cues for hunger and satiety. It makes eating a more conscious act 5. Write down everything you eat or drink for 3 days. The FOOD LOG fulfills several functions: 1. It makes the patient more aware of what he/she is eating 2. It records the times and patterns of eating 3. It gives a record of what the patient eats for further counseling aimed at improving quality of diet. 4. It helps the patient to identify if emotions are involved in the decision to eat. These 5 steps of intuitive eating can be worked on one at a time. The patient may already be doing some of them. It is important to ask the patient,” Are there any of these steps you feel could help you in eating? What do you think you would like to work on first? Page 2 of the handout is important because it conveys that losing weight is not just what you eat or when or why, but it is part of a bigger health picture. Eating nutritiously is part of being healthy. Exercising is vital to everyone’s health and dieting without exercising is not healthy because living without exercising is not healthy! Exercise promotes increased metabolism and supports muscle development which maintains the high basal metabolic rate. Trying to lose weight is really not the goal--- learning to be healthy IS the permanent goal. The habits we are working on are life long changes for the better. Weight loss can be discouraging when the body is viewed as “the enemy”. Help your patient to see their body as a tool, a friend, and a gift that he/she is in charge of. Our patients are just like us—whole persons! So remember that weight loss is not a product, it’s a process of learning to care for self and balance life. The goal is not pounds off, that is the side effect of the true goal: healthy living and better self-management in all areas of life. OTHER MATERIALS AVAILABLE: Eat Heart Healthy You can lower your blood pressure You can lose weight Don’t gain while you are quitting Exercise- what you need to know (1 page) 6 common signs of a stroke All of these are in English and Spanish except 6 signs of a stroke and don’t gain while you quit. To view all these materials see our website: http://chcasvr2.chcar.org/Services/Services.htm