* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Anatomy of the female perineum, reproductive organs
Survey
Document related concepts
Transcript
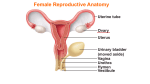
Anatomy of the female perineum, reproductive organs Dr.Munirah Batarfi MD, MSc, & PhD 1 Female Reproductive System consists of: an ovary on each side; and a uterus, vagina, and clitoris in the midline . In addition, a pair of accessory glands (the greater vestibular glands) are associated with the tract. 2 Uterus 3 inches long by 2 in. wide and 1 in. thick. Parts:• Fundus: the rounded part of the body that lies superior to the attachments of the uterine tubes. • Body : the part of the uterus between the fundus and the cervix. The vesical surface of the body of the uterus faces the vesicouterine pouch and the intestinal surface faces the rectouterine pouch. The broad ligament is attached to the lateral surface of the body of the uterus. • • Isthmus : the narrowed portion of the body that is superior to the cervix. • Cervix : the thick walled portion of the uterus that protrudes into the vaginal canal. Uterus. Anterior view. The anterior half of the uterus and vagina have been cut away. 3 Normal position of the uterus Normal position: Anteverted, Anteflexed: Anteversion refers to the angle at the external os being approximately 90 degrees, measured from the angle between the vagina and the cervical canal. Anteflexion refers to the angle at the internal os being approximately 170 degrees, measured from the angle between the uterine and cervical canal. Uterus and vagina. A. Angles of anteflexion and anteversion. B. The cervix protrudes into the vagina. 4 RVF: Retroversion, Retroflexion:• Retroversion is the widening of the angle between the vaginal and cervical axis greater than 90 degrees. If the angle of the external os increases and approaches 180 degrees, the uterus is in danger of fall into the vaginal canal (prolapse). Retroflexion is the widening of the angle between the cervical and uterine axis greater than 180 degrees. The two angles are independent of each other, and the uterus can possibly be found in any combination of anteversion, retroversion, anteflexion, or retroflexion. Variants of uterine positions 5 Blood Supply to the Uterus Uterine artery: Br. of internal iliac Ar.; crosses over the ureter at the base of the broad ligament (risk of injury at hystrectomy). Ovarian artery: Br. from abdominal aorta. Uterine vein---drains into internal iliac vein. 6 Peritoneum in the pelvis & Broad ligament • a shallow vesico-uterine pouch occurs anteriorly, between the bladder and uterus, and a deep rectouterine pouch (pouch of Douglas) occurs posteriorly, between the uterus and rectum. • large fold of peritoneum (the board ligament), with a uterine tube enclosed in its superior margin and an ovary attached posteriorly, is located on each side of the uterus and extends to the lateral pelvic walls. Rectouterine pouch (Douglas pouch):•Most dependent (PV exam.), •Accumulation of pus or blood, •Perforation by misguided, non sterile instr. (illegal abortion)---- pelvic peritonotis, may be fatal. 7 Broad Ligament of the Uterus The broad ligament of the uterus is formed by two layers of peritoneum that extend from the lateral side of the uterus to the lateral pelvic wall. The broad ligament has three parts: • Mesosalpinx: supports the uterine tube. • Mesovarium: attaches the ovary to the posterior aspect of the broad ligament • Mesometrium: the part of the broad ligament that is below the attachment of the mesovarium. At the base of the broad ligament, the uterine artery crosses the ureter. Contents of the broad ligament:• Uterine tube • Uterine artery, lymph vessels& nerves. • Ovarian artery • Round ligament • Ovarian ligament • Embryonic remenants (epoophoron& paroophoron). 8 Parts of the broad ligament (Cont’d) Uterus& Adnexa 9 Pelvic fascia in women (Ligaments supporting the uterus) Condensations of fascia form ligaments that extend from the cervix to these pelvic walls. : • anterior (pubocervical ligament), •lateral (transverse cervical or cardinal ligament or Mackenrodt ligament), and •posterior (uterosacral ligament). These ligaments, together with the perineal membrane, the levator ani muscles, and the perineal body, are thought to stabilize the uterus in the pelvic cavity. •The most important of these ligaments are the transverse cervical or cardinal ligaments, which extend laterally from each side of the cervix and vaginal vault to the related pelvic wall. 10 Ovary • Pair of organs, size of 4x2 cm, found in upper pelvic region. • Ligaments supporting:Mesovarium: attaches ovaries to broad ligament Ovarian ligament: anchors ovary to uterus Suspensory ligament: covers blood vessels to ovaries Blood supply: Ovarian artery& corresponding vein. 11 Ovaries and broad ligament • The mesovarium, a posterior extension of the broad ligament, which attaches to the ovary. • The peritoneum of the mesovarium becomes firmly attached to the ovary as the surface epithelium of the ovary. • The ovaries are positioned with their long axis in the vertical plane. The ovarian vessels, nerves, and lymphatics enter the superior pole of the ovary from a lateral position and are covered by another raised fold of peritoneum, which with the structures it contains forms the suspensory ligament of ovary (infundibulopelvic ligament). (Ovarian ligaments) • The inferior pole of the ovary is attached to a fibromuscular band of tissue (the ligament of ovary), which courses medially in the margin of the mesovarium to the uterus and then continues anterolaterally as the round ligament of uterus. 12 Uterine tubes • Narrow, 4 inch tube extends from ovary to uterus. Parts:-Fimbria are moving, finger-like processes -Infundibulum is open, funnel-shaped portion near the ovary. -Ampulla is central region of tube -Isthmus is narrowest portion, joins with uterus. Function: transport of oocytes by ciliary action and peristalsis. Ampulla is the site of fertilization. Blood supply: • • Uterine artery& corresponding vein Ovarian artery & corresponding vein 13 Vagina - It lies between the urinary bladder and rectum. - It measures about 3 inches long. – Its orifice is partially closed with membrane (hymen). – The anterior wall of the vagina is related to the base of the bladder and to the urethra; Posteriorly, the vagina is related principally to the rectum. Vaginal fornices: – Anterior – Posterior – 2 lateral fornices. Supports: Pelvic floor muscles, ligaments of the cervix & perineal body. Blood supply: Vaginal artery& vaginal br. of uterine artery. Vaginal vein---drains into Intern. Iliac vein Vagina. A. Left half of pelvis cut away. B. Vaginal fornices and cervix as viewed through a speculum. 14 15 Branches of the anterior trunk of the internal iliac artery in Female 16 The greater vestibular glands (Bartholin's glands) • • • • • The greater vestibular glands (Bartholin's glands) are small, pea-shaped mucous glands that lie posterior to the bulbs of the vestibule on each side of the vaginal opening and are the female homologues of the bulbourethral glands in men . However, the bulbourethral glands are located within the deep perineal pouch, whereas the greater vestibular glands are in the superficial perineal pouch. The duct of each greater vestibular gland opens into the vestibule of the perineum along the posterolateral margin of the vaginal opening. Like the bulbourethral glands in men, the greater vestibular glands produce secretion during sexual arousal. The ducts of the para-urethral glands (Skene's glands) open into the vestibule, one on each side of the lateral margin of the urethra. 17 Pudendal nerve In women The pudendal nerve has three major terminal branches: • Inferior rectal • Perineal nerves • Dorsal nerve of clitoris which are accompanied by branches of the internal pudendal artery 18 Female external genitalia 19 20 Cervical Carcinoma 21 Uterine Endometrial Carcinoma Endometrial carcinoma is the most common malignancy of the female reproductive tract. It often occurs between the ages of 55 and 65 years, and risk factors include the following: ● Obesity (increased estrogen synthesis from fat cells without concomitant progesterone synthesis) ● Estrogen replacement therapy without concomitant progestin ● Breast or colon cancer ● Early menarche or late menopause (prolonged estrogen stimulation) ● Chronic anovulation ● Diabetes 22 Chronic Pelvic Inflammatory Disease • Recurrent or chronic infections of the uterine tubes or other adnexa result in cystic dilation (hydrosalpinx) and can account for approximately 40% of female infertility. • The inflammation can cause scarring, causing problems with fertility, pelvic pain, or tubal (ectopic) pregnancy. • The most affected age group is 15 to 25 years of age. • Unilateral or bilateral adnexal masses are usually sausage shaped and may be palpable. 23 24 Ovarian Cancer 25 Radiograph of a hysterosalpingogram, demonstrating a uterine cavity with a rounded filling defect on one side and probable bilateral proximal tubal occlusion (blockage). Note the slightly brighter region of white dye circumscribing the filling defect, which is a characteristic of persistent defects like fibroids or endometrial polyps (rather than round air bubbles in the radiopaque dye). 26 References: • Gray's Anatomy for Students- Second edition • Netter’s Clinical Anatomy, Second edition 27