* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Tracheal extubation was accomplished when the
Survey
Document related concepts
Transcript
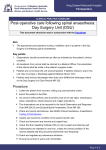
Web Supplement: Criteria for Tracheal Extubation, ICU Discharge, Hospital Discharge, and Postoperative Complications A. Tracheal extubation: 1. Hemodynamic stability 2. Absence of uncontrolled arrhythmias 3. Core temperature > 36°C 4. Chest tube drainage < 100 mL in the past 2 hours 5. Arterial oxygen saturation (SpO2) >90% on a FIO2 < 0.5 6. An arterial pH > 7.3 7. Responsiveness to simple commands. B. ICU discharge: 1. Absence of significant arrhythmias 2. No need for inotropic support 3. SpO2 > 90% on an FIO2 < 0.5 4. Chest tube drainage < 50 mL in the past 2 hours 5. Urine output > 0.5 mL·kg-1·hr-1 6. Patient alert and cooperative. C. Hospital discharge: 1. Hemodynamically stable without arrhythmias 2. Afebrile without signs of infection 3. Able to eat, void, and defecate normally 4. Adequately controlling pain on oral analgesics 5. Ambulating independently with little or no assistance. D. Postoperative complications (according to the previously established definitions): 24 1. Respiratory: mechanical ventilation for > 24 hours or postoperative pneumonia (pulmonary infiltrate with positive microbial cultures) 2. Cardiac: atrial fibrillation detected on 12-lead standard EKG; arrhythmia requiring treatment with electrical cardioversion or antiarrhythmic medications; myocardial infarction defined by new Q waves on the EKG or elevation of cardiac troponin values; heart failure requiring two or more inotropic medications or use of an intra-aortic balloon pump for > 24 hours. 3. Neurologic: stroke, defined as a new central neurological deficit; or postoperative confusion, defined as disorientation to time and/or place and inability to cooperate with simple commands. 4. Renal: acute increase in serum creatinine > 50% or the need for dialysis. 5. Infection: wound infection requiring surgical debridement or antibiotics. ICU=intensive care unit; FI02=fraction of inspired oxygen concentration