* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 291917
Survey
Document related concepts
Transcript
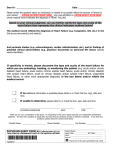
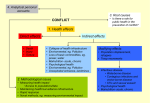
Specificity: Coding rules require precise documentation as to location, laterality, device, approach, procedure, qualifier; eg., meningitis due to Lyme Disease, malignant neoplasm of lower quadrant of right female breast, atherosclerotic heart disease of native coronary artery with unstable angina pectoris Consistency: Diagnoses are noted and then repeated throughout the patient’s stay. One time mention does not qualify as diagnosis for coding purposes. Complication: Specify type complication: (infection, inflammation, if caused by implanted device, from operation or procedure. If current visit related to previous condition, specify diagnosis and late effect if present (CVA, MI, etc) Present on Admission (POA): CMS requires all hospitals to report Present on Admission (POA) status for each diagnoses. Present at the time of inpatient admission or conditions that occur during an outpatient status (including ED) are POA Indication for (treatment, medication, radiology etc): Include indication for medications, radiology orders (MRI, CT), procedures (PICC, EGD, colonoscopy), treatments (nebs), ultrasound (echo, diagnostic, gallstones, etc) Principle Diagnosis: Is that condition established after study to be chiefly responsible for occasioning the admission of the patient to the hospital for care. Chronic Kidney Disease (CKD)/Chronic Renal Failure (>than 6 months of increased creatinine and/or decreased GFR) End Stage Renal Disease (ESRD): Chronic dialysis (>3months) Acute on Chronic Renal Failure: Established CKD (stage?) with increase in creatinine above patient’s baseline creatinine of >.0.3-0.5. CKD Staging 1 >90 GFR *Clarify Renal Insufficiency to a more specific diagnosis 2 60-89 GFR *Indicate if DM complication 3 30-59 GFR 4 15-29 GFR 5 <15 (indicate if ESRD) Reference : www.nephronline/management/ckd.html Acute Renal Failure(ARF)/Acute Kidney Injury(AKI): Creatinine increase of >0.3-0.5 or use RIFLE criteria. http://www.smjr.org/files/nephro/RIFLE.PDF *Specify cause of AKI: Sepsis, shock, drug toxicity, hypotension, obstruction (include hydronephrosis if present) *Specify type of AKI: Acute tubular necrosis (ATN), interstitial nephritis, cortical or medullary necrosis Hypertension: Specify type: Essential; Primary;Secondary; Malignant; Accelerated, include complications (CVA, etc, consider Hypertensive Heart and Kidney disease if manifestations present) Acute Respiratory Failure: Document cause, if possible (eg: exacerbation of COPD/ Bronchitis , Pneumonia, Acute pulm edema, etc) *Abnormal ABGs or Acidosis: Specify corresponding diagnosis Anemia: Document cause of anemia, if blood loss anemia, document acute or chronic, expected or unexpected, related conditions/complications. Establish cause and effect; eg., anemia secondary to acute blood loss from hemorrhagic ulcer Neuro: Dementia - specify cause/type - “Alzheimer’s” Encephalopathy (type), Acute Stroke (cerebral infarction) TIA, cerebral edema, seizure disorder, late effects of a stroke (noting if greater than six months) Altered Mental Status: Clarify to diagnosis; eg., delirium (cause), encephalopathy (type: metabolic toxic (drugs ?), hepatic); acute confusional state; psychosis Cancer: Specify if treatment directed at primary site or metastatic site, include morphology, specify if anemia caused by antineoplastic drugs or disease process, include concurrent diagnoses such as malnutrition (type?) Admission for Radiology/Chemotherapy : Include diagnosis for treatment, if metastasis, etc. Sepsis: Document if due to UTI/Wounds/Resp. etc., source? (infection?) Urosepsis codes to UTI only! Establish cause and effect; eg., UTI secondary to indwelling urinary catheter. Diabetes: Specify DM-I or DM-II Controlled or Uncontrolled (Hgb A1c >7) Link DM to complications if present (e.g. ulcer, neuropathy, nephropathy, gastroparesis, retinopathy, cellulitis, osteomyelitis). Establish cause and effect; eg., peripheral vascular disease due to diabetes Debridement: Include deepest layer debrided *Specify if excisional or non-excisional: Excisional: Definite, sharp, cutting away of tissue using scissors, blades, nippers, “surgical debridement” Non-Excisional: Mechanical debridement using scrubbing, brushing, ultrasonic curettes, Versajet™, irrigation Congestive Heart Failure (CHF): Acuity and Type Acuity: Acute / Chronic / Acute on Chronic (exacerbation) Type: - Systolic (EF < 40) or Diastolic (on echo), combined *Document any CHF complications, ie arrhythmia, Resp failure, Acute pulmonary edema. Cardiomyopathy: Document separately from CHF and specify type (ischemic/non, hypertensive, sarcoid, primary) Compression Fracture: Clarify if traumatic or pathologic (degenerative), include osteopenia if present. Establish cause and effect; eg., fracture due to osteoporosis Alcoholism: Include acuity (intoxication?), indication for CIWA scale, course of illness (episodic, continuous, in remission), complications (cirrhosis, gastritis, hepatitis, etc) CLINICAL DOCUMENTATION EXCELLENCE General Documentation Principles [email protected] Phone 202.660.6782 Fax 202.537.4477 Please answer CDE queries within 24 hours SIRS: Meets sepsis criteria (WBC, tachycardia, tachypnea, fever) without infection. Caused by - trauma, CHF, acute COPD, burns, arthritis, MI, drug abuse BMI: both <19 or >40 typically require additional resources: Morbid Obesity: BMI >40 Document both the BMI and the diagnosis (obesity, morbid) Underweight/Cachexia: BMI <19 Document BMI, diagnosis and malnutrition if present Malnutrition: Specify degree Normal Mild Moderate Severe Malnutrition Malnutrition Malnutrition Pre-Albumin >17 12-17 7-11 <7 Albumin 3.5-5.0 3.1-1-.4 2.4-3.0 2.4 Trans-ferrin 220-400 201-219 150-200 <150 BMI 19-24 Additionally, clarify type: protein-calorie, protein malnutrition, calorie malnutrition Also, document a diagnosis for a dietary consult Pneumonia: Clarify type of pneumonia when possible eg: bacterial (organism?); aspiration, ventilator-assoc, post-op. Also document if POA and include any related conditions (Acute Respiratory Failure, Sepsis) Skin Ulcer: indicate if: decubitus (note location and stage), diabetic, veno/arteriostasis, presence of infection Chronic Kidney Disease (CKD)/Chronic Renal Failure (>than 6 months of increased creatinine and/or decreased GFR) End Stage Renal Disease (ESRD): Chronic dialysis (>3months) Acute on Chronic Renal Failure: Established CKD (stage?) with increase in creatinine above patient’s baseline creatinine of >.0.3-0.5. CKD Staging 1 >90 GFR *Clarify Renal Insufficiency to a more specific diagnosis 2 60-89 GFR *Indicate if DM complication 3 30-59 GFR 4 15-29 GFR 5 <15 (indicate if ESRD) Reference : www.nephronline/management/ckd.html Acute Renal Failure(ARF)/Acute Kidney Injury(AKI): Creatinine increase of >0.3-0.5 or use RIFLE criteria. http://www.smjr.org/files/nephro/RIFLE.PDF *Specify cause of AKI: Sepsis, shock, drug toxicity, hypotension, obstruction (include hydronephrosis if present) *Specify type of AKI: Acute tubular necrosis (ATN), interstitial nephritis, cortical or medullary necrosis Hypertension: Specify type: Essential; Primary;Secondary; Malignant; Accelerated, include complications (CVA, etc, consider Hypertensive Heart and Kidney disease if manifestations present) Specificity: Coding rules require precise documentation as to location, laterality, device, approach, procedure, qualifier; eg., meningitis due to Lyme Disease, malignant neoplasm of lower quadrant of right female breast, atherosclerotic heart disease of native coronary artery with unstable angina pectoris Consistency: Diagnoses are noted and then repeated throughout the patient’s stay. One time mention does not qualify as diagnosis for coding purposes. Complication: Specify type complication: (infection, inflammation, if caused by implanted device, from operation or procedure. If current visit related to previous condition, specify diagnosis and late effect if present (CVA, MI, etc) Present on Admission (POA): CMS requires all hospitals to report Present on Admission (POA) status for each diagnoses. Present at the time of inpatient admission or conditions that occur during an outpatient status (including ED) are POA Indication for (treatment, medication, radiology etc): Include indication for medications, radiology orders (MRI, CT), procedures (PICC, EGD, colonoscopy), treatments (nebs), ultrasound (echo, diagnostic, gallstones, etc) Principle Diagnosis: Is that condition established after study to be chiefly responsible for occasioning the admission of the patient to the hospital for care. Diabetes: Specify DM-I or DM-II Controlled or Uncontrolled (Hgb A1c >7) Link DM to complications if present (e.g. ulcer, neuropathy, nephropathy, gastroparesis, retinopathy, cellulitis, osteomyelitis). Establish cause and effect; eg., peripheral vascular disease due to diabetes Debridement: Include deepest layer debrided *Specify if excisional or non-excisional: Excisional: Definite, sharp, cutting away of tissue using scissors, blades, nippers, “surgical debridement” Non-Excisional: Mechanical debridement using scrubbing, brushing, ultrasonic curettes, Versajet™, irrigation Congestive Heart Failure (CHF): Acuity and Type Acuity: Acute / Chronic / Acute on Chronic (exacerbation) Type: - Systolic (EF < 40) or Diastolic (on echo), combined *Document any CHF complications, ie arrhythmia, Resp failure, Acute pulmonary edema. Cardiomyopathy: Document separately from CHF and specify type (ischemic/non, hypertensive, sarcoid, primary) Compression Fracture: Clarify if traumatic or pathologic (degenerative), include osteopenia if present. Establish cause and effect; eg., fracture due to osteoporosis Alcoholism: Include acuity (intoxication?), indication for CIWA scale, course of illness (episodic, continuous, in remission), complications (cirrhosis, gastritis, hepatitis, etc) Acute Respiratory Failure: Document cause, if possible (eg: exacerbation of COPD/ Bronchitis , Pneumonia, Acute pulm edema, etc) *Abnormal ABGs or Acidosis: Specify corresponding diagnosis Anemia: Document cause of anemia, if blood loss anemia, document acute or chronic, expected or unexpected, related conditions/complications. Establish cause and effect; eg., anemia secondary to acute blood loss from hemorrhagic ulcer Neuro: Dementia - specify cause/type - “Alzheimer’s” Encephalopathy (type), Acute Stroke (cerebral infarction) TIA, cerebral edema, seizure disorder, late effects of a stroke (noting if greater than six months) Altered Mental Status: Clarify to diagnosis; eg., delirium (cause), encephalopathy (type: metabolic toxic (drugs ?), hepatic); acute confusional state; psychosis Cancer: Specify if treatment directed at primary site or metastatic site, include morphology, specify if anemia caused by antineoplastic drugs or disease process, include concurrent diagnoses such as malnutrition (type?) Admission for Radiology/Chemotherapy : Include diagnosis for treatment, if metastasis, etc. Sepsis: Document if due to UTI/Wounds/Resp. etc., source? (infection?) Urosepsis codes to UTI only! Establish cause and effect; eg., UTI secondary to indwelling urinary catheter. SIRS: Meets sepsis criteria (WBC, tachycardia, tachypnea, fever) without infection. Caused by - trauma, CHF, acute COPD, burns, arthritis, MI, drug abuse BMI: both <19 or >40 typically require additional resources: Morbid Obesity: BMI >40 Document both the BMI and the diagnosis (obesity, morbid) Underweight/Cachexia: BMI <19 Document BMI, diagnosis and malnutrition if present Malnutrition: Specify degree Normal Mild Moderate Severe Malnutrition Malnutrition Malnutrition Pre-Albumin >17 12-17 7-11 <7 Albumin 3.5-5.0 3.1-1-.4 2.4-3.0 2.4 Trans-ferrin 220-400 201-219 150-200 <150 BMI 19-24 Additionally, clarify type: protein-calorie, protein malnutrition, calorie malnutrition Also, document a diagnosis for a dietary consult Pneumonia: Clarify type of pneumonia when possible eg: bacterial (organism?); aspiration, ventilator-assoc, post-op. Also document if POA and include any related conditions (Acute Respiratory Failure, Sepsis) Skin Ulcer: indicate if: decubitus (note location and stage), diabetic, veno/arteriostasis, presence of infection CLINICAL DOCUMENTATION EXCELLENCE General Documentation Principle [email protected] Phone 202.660.6782 Fax 202.537.4477 Please answer CDE queries within 24 hours