* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Kovacs_Files - Matthias Heyner
Survey
Document related concepts
Transcript
KOVÁCS NOTES
OF
HUMAN ANATOMY
2
UPPER LIMB
PECTORAL REGION (including Infraclavicular region)
Superior: clavicle,
Lateral: deltoidopectoral sulcus,
Inferior: inferior margin of the pectoralis major,
SKIN INNERVATION:
Medial and intermediate supraclavicular nerves (from the cervical plexus),
Anterior cutaneous branches of the intercostal nerves.
Just underneath the skin is the superficial pectoral fascia (covering the pectoralis major) which continues
in the axillary region to become the superficial axillary fascia (base-floor of the axillary fossa together with
the skin). By removing the fascia, we will find the pectoralis major muscle.
The pectoralis minor muscle lies deep to the pectoralis major. It must be cut to dissect the axillary
artery, vein, and the cords of the brachial plexus. By lying over the middle of the axillary artery, it divides
the artery into three parts (proximal to the muscle, covered by the muscle, and distal to the muscle).
Axillary artery: 1st part: Superior thoracic artery + thoracoacromial artery
2nd part: Lateral thoracic artery + subscapular artery
3rd part: Anterior and posterior circumflex humeral arteries.
The largest branch is the subscapular artery, giving the branches circumflex scapular and thoracodorsal
arteries.
The axillary vein is medial to the axillary artery which is surrounded by the cords of the brachial plexus.
Brachial plexus: It comes from the ventral rami of the spinal nerves C5-T1. The spinal nerves come out
from the vertebral canal through the intervertebral foramen. When they come out, they divide into anterior
(ventral) and posterior (dorsal) rami.
Above the clavicle, the brachial plexus forms three trunks:
Superior trunk: C5-C6
Middle trunk:
C7
Inferior trunk:
C8-T1
The lateral cord is formed by the superior and middle trunks, the medial cord by the inferior trunk, and
the posterior cord from all three.
The musculocutaneous nerve pierces through the coracobrachialis muscle, and it goes below the
brachialis muscle. At the distal end, it becomes the lateral antebrachial cutaneous nerve that comes out from
below the biceps at the lateral side of the tendon (running together with the cephalic vein).
The Median nerve arises from the medial and lateral cords (having the appearance of a V-shaped nerve),
and it runs through the medial bicipital groove on the arm together with the ulnar nerve, the medial brachial
cutaneous and medial antebrachial cutaneous nerves, and the brachial artery. Then, it goes to the cubital
fossa (at the middle), and it is the most medial structure of the cubital fossa. The middle structure is the
brachial artery, and the lateral structure is the tendon of the biceps muscle. The median nerve (after the
cubital fossa) goes to the forearm between the flexor digitorum superficialis (in its fascia) and the flexor
digitorum profundus in the midline of the forearm (that's why it's called the median nerve). Then, it goes
through the carpal canal. In the palmar region, it is covered by the palmaris longus tendon. If this muscle
3
is missing, the nerve runs between the flexor carpi radialis tendon and the flexor digitorum tendons. In the
palm, it divides into superficial and the deep branches. The deep branch innervates the thenar muscles
(except the adductor) and the 1st and 2nd lumbricals. The superficial branch innervates the skin of the palm
and the lateral 3½ fingers by seven digital branches.
The Ulnar nerve arises from the medial cord of the brachial plexus and runs though the medial bicipital
groove on the arm, but leaves the groove and pierces through the medial intermuscular septum and goes to the
sulcus nervi ulnaris. Then, it reaches the forearm between the two heads of the flexor carpi ulnaris muscle.
In the inferior 1/3 of the forearm, we can find the ulnar nerve covered by the flexor digitorum profundus
together with the ulnar artery. The ulnar artery, in the superior 1/3 of the forearm, is between the deep and
the superficial muscles, and afterward it joins the ulnar nerve.
The ulnar nerve goes into the palm in front of the flexor retinaculum (it doesn't pass through the carpal
canal) together with the ulnar artery, where it gives superficial and deep branches. The deep branch
innervates the interossei muscles, the 3rd and 4th lumbricals, the adductor pollicis, and the hypothenar
muscles. The superficial branch innervates the ulnar 1½ fingers, the ulnar 1/2 of the palm, and the palmaris
brevis.
The medial brachial and antebrachial cutaneous nerves arise from the medial cord of the brachial plexus
and are found in the medial bicipital groove. The medial antebrachial cutaneous nerve pierces the brachial
fascia through the basilic hiatus and joins the basilic vein. The medial brachial cutaneous nerve
anastomoses with the 1st, 2nd (and sometimes 3rd) intercostal nerves. This anastomosis is called the
intercostobrachial nerve (innervates the skin of the axilla).
The Radial nerve arises from the posterior cord of the brachial plexus. It is located in front of the
tendon of latissimus dorsi muscle and the teres major, runs to the superior part of the sulcus bicipitalis
medialis, and leaves the sulcus (it is not a structure of the sulcus) where it goes to the extensor muscles of the
arm between the triceps (medial and lateral head) into the sulcus nervi radialis. Then, it comes forward
again in the cubital region (not into the cubital fossa) in the lateral side between the brachialis and
brachioradialis muscles. You must move apart those two muscles to find the nerve.
There it divides into two branches (superficial and deep). The superficial branch innervates the radial
2½ fingers (by digital nerves) and skin at the dorsal side of the hand. The deep branch pierces through the
superficial muscles (supinator) and innervates the extensor muscles.
The Axillary nerve arises from the posterior cord of the brachial plexus and gives skin branches (lateral
cutaneous branches) that are not dissectable.
4
AXILLARY REGION
The region basically consists of the axillary fossa; however, it also includes the skin covering the walls of
the fossa. If described as a surface region of the anterior side of the body (as it is usually presented), the
axillary region is a triangular wedge (the most lateral portion of the Pectoral region):
Lateral: Deltopectoral sulcus
Medial: Thoracic wall, projected onto the skin
Inferior: Anterior axillary fold
The axillary fossa pyramid-shaped fossa. Its base is open, but it is defined by the anterior and posterior
axillary folds (frequently forgotten!). This pyramid has four solid walls:
Anterior: Pectoralis major and minor muscles,
Posterior: Subscapular, teres major, and latissimus dorsi,
Medial: Thoracic wall and serratus anterior,
Lateral: Humerus, flexors of the arm, and coracobrachialis.
The clavipectoral fascia continues to the superior axillary fascia which keeps the skin fixed to the axillary
fossa. In the axillary fossa, there are lymph nodes.
In the axillary region, structures (nerves, veins, arteries) are the same as in the pectoral region.
Medial rotators of the humerus: latissimus dorsi, teres major, subscapularis (all attached to the crest of
the lesser tubercle).
Lateral rotators of the humerus: teres minor, infraspinatus.
ORIGINS AND INSERTIONS:
Biceps: Supraglenoid tubercle Tuberosity of radius
Coracoid process
Coracobrachialis: Coracoid process middle of the shaft of the humerus
Brachialis: Lower half of humerus Condyloid process of ulna
ANTERIOR BRACHIAL REGION
Superior: Inferior border of the pectoralis major muscle,
Inferior: Three fingers above the cubital sulcus,
Medial: Medial margin of the arm,
Lateral: Lateral margin of the arm (lat and med defining the volar surface of the arm).
SKIN INNERVATION:
Medial brachial cutaneous Nerve (medial cord of brachial plexus)
Lateral brachial cutaneous nerve (end branch of the axillary nerve- usually not dissectible)
SUPERFICIAL STRUCTURES:
Lateral border: Cephalic vein and deltoid branch of the thoracoacromial artery (in the deltopectoral
sulcus). Know the structures of the deltopectoral sulcus.
Medial border: At the inferior part of the region, lies the basilic vein (foramen on the brachial fascia:
basilic hiatus) and the medial antebrachial cutaneous nerve
The brachial fascia covers the flexor muscles of the arm and sends two septa-- medial and lateral
intermuscular septa (separates flexors from extensors). They divide the arm into two compartments; flexor
and extensor.
Removing the fascia, we will find the flexors, namely the biceps brachii (the long head is lateral and the
short head is medial). Below the biceps are the brachialis and the coracobrachialis. Behind the biceps,
the musculocutaneous nerve pierces through the coracobrachialis and is located between the biceps and the
brachialis muscles. Its end branch is the lateral antebrachial cutaneous nerve that accompanies the cephalic
vein in the forearm.
5
Brachialis function: flexion and a little supination of the elbow joint and arm.
Coracobrachialis function: flexion and adduction of the arm.
The main structures of the brachial region are found in the medial bicipital groove: the median nerve,
ulnar nerve, medial brachial and antebrachial cutaneous nerves, and the brachial artery. Branches of the
brachial artery are found in this region: 1)Profunda brachii artery accompanies the radial nerve (and gives
middle collateral and radial arteries), 2)Superior and inferior ulnar collateral arteries.
The superior ulnar collateral artery accompanies the ulnar nerve. The Median nerve crosses the brachial
artery in the brachial region. It is the most medial structure in the cubital fossa.
ANTERIOR CUBITAL REGION
Superior: two fingers above the cubital fold (sulcus),
Inferior: two fingers below the cubital fold,
Medial and Lateral: medial and lateral margins of the arm (med & lat epicondyles).
SUPERFICIAL STRUCTURES:
Medial: the basilic vein together with the medial antebrachial cutaneous nerve.
Lateral: the cephalic vein together with the lateral antebrachial cutaneous nerve.
Between the basilic and cephalic veins, there is an anastomosis which is called the median cubital vein
(the network is "M" or "N" shaped). In clinics, blood is taken from this vein for examination. Beneath
these structures lies the cubital fascia (continuation of brachial fascia). Below this fascia lie the structures
and muscles of the cubital fossa.
The cubital fossa is made by the flexors and extensors of the forearm. It is a V-shaped fossa (triangular) that opens upward. The medial border of the fossa is formed by the pronator teres muscle and the
flexor muscles of the forearm. The lateral border is formed by the brachioradialis muscle and the extensors
of the forearm. The basefloor of the fossa is formed by the brachialis muscle and lateral side by the
supinator muscle (surrounding the radius).
Structures of the fossa:
Lateral: tendon of the biceps
Middle: brachial artery
Medial: median nerve
In the cubital fossa, the brachial artery divides into two branches: the radial artery (which later gives the
radial recurrent artery) and the ulnar artery (giving the ulnar recurrent artery- anastomosing mainly with the
inferior ulnar collateral artery).
At the lateral side of the region lies the radial nerve. It is not a structure of the cubital fossa, but is a
structure of the region. The radial nerve runs between the brachialis and the brachioradialis muscles.
In this region, the origins of the flexors (and some of the extensors) of the forearm can be seen.
Brachioradialis: Originates above the lateral epicondyle and inserts in the styloid process of the radius.
It flexes the forearm (though it is in the extensor compartment). IF the forearm is pronated, it supinates it
until the middle position and vice versa ("saluting movement").
Extensor carpi radialis longus and brevis: Originate at the lateral epicondyle of the humerus and insert at
the base of the 2nd and 3rd metacarpal bones. So, the origin of the extensors are included in this region.
6
ANTERIOR ANTEBRACHIAL REGION
Superior: three fingers below the cubital sulcus
Inferior: a line along the styloid processes of the ulna and radius OR three fingers above the carpal
eminence.
SKIN INNERVATION:
Medial and lateral antebrachial cutaneous nerves.
SUPERFICIAL STRUCTURES:
The basilic and cephalic veins. The medial and lateral antebrachial cutaneous nerves do not innervate
only the volar surface, but also the ulnar margin of the forearm and ulnar part of the dorsal surface. The
same for the lateral surface (radial).
The two veins originate from the dorsal carpal venous plexus (plexus venosus dorsalis manu). Deep to
the antebrachial fascia, we find the flexor muscles. The brachioradialis muscle is seen at the radial border
of the region.
Structures of the region:
1) Ulnar nerve and artery, covered by the flexor carpi ulnaris. To see the superior 1/3 of the ulnar
artery, cut the superficial muscles.
2) Radial artery and superficial branch of the radial nerve. They are covered by the brachioradialis
muscle. Underneath the flexor digitorum superficialis muscle, the medial nerve runs in the midline of the
region between the flexor digitorum superficialis and profundus. It is attached to the superficialis
(embedded in its fascia), so before cutting the flexor digitorum superficialis muscle, first dissect the nerve
and then cut the muscle
The median nerve innervates all the flexors except the flexor carpi ulnaris and flexor digitorum profundus
(the ulnar half). Deep to the flexor digitorum profundus, you can see the interosseous membrane and the
pronator quadratus, a quadrangular muscle between the radial margin of the radius and the ulnar margin of
the ulna. You will also see the anterior interosseous branch of the median nerve and the anterior
interosseous artery (from the common interosseous artery from the ulnar artery).
VOLAR CARPAL REGION
Superior: level of the styloid processes
Inferior: level of the pisiform bone, three fingers above the carpal eminence.
Medial and lateral: medial and lateral edges of the wrist.
SKIN INNERVATION:
End branches of the lateral and medial antebrachial cutaneous nerves and tiny cutaneous branches from
the median and ulnar nerves (not dissectable).
7
SUPERFICIAL STRUCTURES:
Basilic and cephalic veins. Removing the fascia reveals the tendon of the palmaris longus (missing 1020% of the time).
Order of structures from radial to ulnar:
1) Brachioradialis muscle (sometimes also extensor pollicis brevis and abductor pollicis longus.
2) Radial artery, together with two radial veins. We cannot see the superficial branch of the
radial nerve.
3) Flexor carpi radialis tendon.
4) Median nerve.
5) Palmaris longus (covers the median nerve, so sometimes is right above it).
6) Flexor digitorum superficialis muscle (4)
7) Ulnar artery and ulnar nerve.
8) Flexor carpi ulnaris muscle.
Carpal canal:
It is important to know the structures passing through the canal, especially the tendon sheathes. The
most superficial is the skin, then the veins and cutaneous nerves (between the fascia and the skin).
Removing the fascia reveals the arteries, nerves, and tendons. If all these are removed, we will find first the
tendons of the flexor digitorum profundus and flexor pollicis longus. Cutting them exposes the pronator
quadratus.
So, the muscles are arranged in three layers, or four if you consider that the palmaris longus is alone the
most superficial muscle.
Structures passing through the carpal canal:
Median nerve
Flexor carpi radialis muscle in one tendon sheath
Flexor digitorum superficialis and profundus in another tendon sheath
Flexor pollicis longus muscle in its own tendon sheath
PALMAR REGION
Inferior: roots of the fingers.
Medial: a line from the pisiform bone to the 5th finger or the medal border of the palm.
Lateral: lateral border of the palm, (a line from the styloid process of the radius to the root of the fingers).
Superior: radial and ulnar carpal eminences.
The most superficial layer is the aponeurosis palmaris (deep to the skin). It covers arteries, nerves, and
tendons of the muscles. It covers the mesothenar space only. We don't have aponeurosis at the thenar and
hypothenar eminences-- only fascia.
THE DIFFERENCE BETWEEN A FASCIA AND AN APONEUROSIS: a fascia is just a thin sheath, an
aponeurosis is a tendon (or a continuation of a tendon). In the palm, the aponeurosis is the continuation
of the palmaris longus.
Below the aponeurosis, we have the superficial palmar arch formed by the ulnar artery and closed by
the superficial palmar branches from the radial artery. The ulnar artery passes over the carpal tunnel (and
not through) together with the ulnar nerve.
The radial artery turns around the base of the first metacarpal below the tendons of the abductor pollicis
longus and the extensor pollicis brevis, and it arises in the foveola radialis (the anatomical snuff box-- a
triangular depression on the lateral side of the wrist that is bounded medially by the tendon of the extensor
pollicis longus and laterally by the tendons of the abductor pollicis longus and extensor pollicis brevis).
Then, it pierces through the 1st interosseous space (between the 1st and 2nd metacarpal bones) and forms the
deep palmar arch in the palm. The superficial palmar arch gives the common digital palmar arteries
8
(together with the common palmar nerves: 3½ fingers from the median nerve, 1½ fingers from the ulnar
nerve).
The first and second fingers are supplied by the princeps pollicis artery (from the deep palmar arch).
The princeps pollicis gives three branches: one for the second finger (radial index artery) and two for the first
.
The deep palmar arch is closed by the deep palmar branch of the ulnar artery and gives palmar metacarpal
arteries that anastomose with the common digital palmar arteries. Together, they form the proper digital
palmar arteries. Proper palmar digital arteries are formed 2-3 cm above the root of the fingers.
You should cut all the tendons of the muscles (flexor digitorum profundus and superficialis) in order to
see interosseous muscles, the deep palmar arch, and the deep branch of the ulnar nerve. The deep
palmar arch is a tiny arch and not well visible.
One finger is supplied by two digital palmar nerves and the medical significance of this is Ober's
anesthesi: if you operate on the fingers, you should anesthetize both sides of the finger.
Tendon sheath: an outer, fibrous layer and an inner, synovial layer. The inner layer has a double layer
which is called vincula tendineum or mesotendineum. This is very important because blood vessels come
through this sheath to supply the tendons. So, you must not lift the tendons during an opera
tion because you will destroy the arteries and the finger will be necrotized.
Inflammation of the tendon sheath is called phlegmon (an obsolete term for inflammation of subcutaneous connective tissue this phlegmon can spread onto the 1st finger through this tendon sheath-- in this
sheath, we don't have tendons of the 2nd, 3rd, and 4th fingers): from 5th to 1st and opposite.
Tendons of the 2nd, 3rd, and 4th do not have tendon sheaths at the palmar region. Their tendon sheaths
begin after the metacarpals.
In the palm, there are 3 palmar and 4 dorsal interossei muscles. The palmar interossei are unipennate,
and the dorsal interossei are bipennate. Unipennate muscles arise from one metacarpal and have the tendon
at one side. Bipennate muscles arise from two metacarpals.
Origin of the palmar interossei:
1st: ulnar surface of 2nd metacarpal.
2nd: radial surface of 4th metacarpal.
3rd: radial surface of 5th metacarpal.
Origin of the dorsal interossei:
1st: from 1st and 2nd metacarpal to 2nd extensor tendon.
Paralysis of the ulnar nerve: Metacarpophalangeal joints are extended and interphalangeal joints are a
little flexed-- clawhand.
9
DELTOID REGION
(Borders are the same as the deltoid muscle)
Anterior: the deltoidopectoral sulcus
Posterior: the posterior border of the deltoid muscle.
SKIN INNERVATION:
The lateral brachial cutaneous nerve (from the axillary nerve) and the lateral supraclavicular nerves
(innervating the shoulder covering the acromion and the surrounding part of the skin).
Just below the skin, we will find the deltoid fascia covering the deltoid muscle. Removing this fascia
exposes the deltoid. The anterior border of the region is the deltoidopectoral sulcus, containing the cephalic
vein and the deltoid branch of the thoracoacromial artery. The deltoid muscle is innervated by the axillary
nerve.
By cutting the deltoid, the main structures of the region can be seen: the Axillary nerve and the Posterior
circumflex humeral artery. These two structures pass through the quadrangular space (Hiatus axillaris
lateralis).
Borders of the lateral axillary hiatus:
Superior: Teres minor
Inferior: Teres major
Medial: long head of Triceps
Lateral: Humerus
The posterior humeral circumflex artery is a branch of the third part of the axillary artery. The axillary
nerve is a branch of the posterior cord of the brachial plexus. You should know the origin and insertion of
the deltoid muscle.
To dissect, lift the muscle first to find the structures, then cut it (vertically to the fibers). There is a
bursa between the greater tubercle of the humerus and the muscle called the subdeltoid bursa.
Three muscles insert to the greater tubercle: supraspinatus, infraspinatus, and teres minor. The
common function of these three muscles is adduction and lateral rotation of the arm. The supraspinatus also
abducts the arm (because it covers the shoulder joint superiorly).
Latissimus dorsi, teres major, and subscapularis all rotate the arm medially. The latissimus dorsi is the
muscle that helps you to put your hand in your back pocket.
If you cut the deltoid muscle, you will see the lateral and medial axillary hiati and the long head of the
triceps that separates the two from each other.
Borders of the medial axillary hiatus (or triangular space):
Superior: Teres minor
Inferior: Teres major
Lateral: long head of the triceps (originating from the
infraglenoid tubercle of the scapula).
The circumflex scapular artery passes through this hiatus.
10
POSTERIOR BRACHIAL REGION
Inferior: three fingers above the olecranon
Superior: the posterior border of the deltoid region
Medial and Lateral: medial and lateral margins of the arm.
SKIN INNERVATION:
Lateral brachial cutaneous nerve (from axillary nerve), the posterior cutaneous branch of the radial nerve,
and the medial brachial cutaneous nerve.
Under the skin, we will find the brachial fascia that sends two septa. The fascia covers the triceps
muscle having three heads: medial, lateral, and long. Medial and lateral heads are found medial and lateral
to the sulcus nervi radialis.
If you cut the lateral head of the triceps, you will find the main structures of the region (located in the
sulcus nervi radialis of the humerus): the radial nerve and the profunda brachii artery (from the brachial
artery).
The branches of the profunda brachii artery are the radial and middle collateral arteries as well as some
muscular branches.
The radial nerve gives muscular branches innervating the triceps and cutaneous branches innervating the
skin at this region.
POSTERIOR CUBITAL REGION
Superior and inferior: three fingers above and below the olecranon.
Medial and lateral: along side the medial and lateral epicondyles of the humerus.
SKIN INNERVATION:
Posterior brachial cutaneous nerve (from the radial nerve), and the medial and lateral brachial and
antebrachial cutaneous nerves.
After removing the skin, find the cutaneous nerves and the fascia (continuation of the brachial and
antebrachial fascia). Deep to the fascia are the muscles (extensors and flexors) arising from the medial and
lateral epicondyles of the humerus, and the insertion of the triceps muscle (olecranon process).
At the medial side of the region, the ulnar nerve is found in the sulcus nervi ulnaris accompanied by the
superior ulnar collateral artery (from the brachial artery). You should know which muscles originate from
the lateral epicondyle.
We can say that the supinator muscle is a continuation of the triceps muscle (the lateral head).
POSTERIOR ANTEBRACHIAL REGION
Medial and lateral: a line along the medial and lateral epicondyles of the humerus or the medial and
lateral borders of the forearm.
Inferior: styloid processes of the radius and ulna.
Superior: three fingers below the olecranon.
SKIN INNERVATION:
Medial, lateral, and posterior antebrachial cutaneous nerves.
Removing the skin, we will find the posterior antebrachial fascia.
find the muscles arranged in two layers-- superficial and deep.
After removing the fascia, you will
11
Superficial: brachioradialis, extensor carpi radialis longus and brevis, extensor digitorum, extensor digiti
minimi, and extensor carpi ulnaris.
If you cut the superficial layer, the main structures of the region can be seen: Deep branch of the radial
nerve, radial interosseous artery (from the common interosseous artery). These structures pierce the
supinator muscle, forming the SUPINATOR CANAL.
Deep: supinator, abductor pollicis longus, extensor pollicis brevis and longus, and extensor indicis.
The main structures in this region are the muscles. Also be able to describe the tendon sheathes of these
muscles (see below).
DORSAL CARPAL REGION
First, find the superficial structures between the skin and the fascia.
SUPERFICIAL STRUCTURES:
Superficial branch of the radial nerve, the dorsal branch of the ulnar nerve, the basilic and cephalic veins.
Then, the extensor retinaculum and the tendon sheaths should be discussed.
Describe and know the carpal synovial sheaths (6):
1) Abductor pollicis longus and extensor pollicis brevis.
2) Extensor carpi radialis longus and brevis.
3) Extensor pollicis longus.
4) Extensor digitorum and extensor indicis.
5) Extensor digiti minimi.
6) Extensor carpi ulnaris.
FOVEOLA RADIALIS
This is located between the extensor pollicis longus (ulnar border) and the abductor pollicis longus and
extensor pollicis brevis (radial border).
SUPERFICIAL STRUCTURES:
Superficial branch of the radial nerve and the cephalic vein lie above the fascia.
find the radial artery.
Below the fascia, we
The radial artery turns around the tendons of th abductor pollicis longus and extensor pollcis brevis and
arises in the foveola radialis. Beneath these two tendons, the radial artery gives the ramus carpi dorsalis,
and from this tiny branch, we have the dorsal metacarpal arteries which anastomose with the common palmar
digital arteries and give the dorsal and volar proper digital arteries, supplying the fingers. After dissecting
the arteries, you should dissect the three tendons.
12
DORSALIS MANUS REGION
First, we have to speak about the innervation (the most important in this region)
1) Superficial branch of the radial nerve
2) Dorsal branch of the ulnar nerve
You should find the dorsal branch of the ulnar nerve and the superficial branch of the radial nerve
together with the cephalic and basilic veins. These two veins arise from the plexus venosus dorsalis manus
or the rete venosum dorsale manus (aka. the dorsal venous arch).
Below the plexus, the fascia covers the tendons of the extensors and some short muscles.
Removing the fascia, you can find the tendons of the extensor digitorum muscle and the tendons of the
muscles going to the thumb: abductor pollicis longus and extensor pollicis brevis (the radial border of the
region) and the tendon of the extensor pollicis longus.
Beneath the tendons, the dorsal interosseous muscles (four; bipennate) and the dorsal metacarpal arteries
from the ramus carpus dorsalis (coming from the radial artery) can be seen. Be prepared to speak about the
origin, insertion, and function of the interosseous muscles (dorsal). Here, there are intertendineous
connections between the extensor tendons.
Fingers do not belong to this region, but they must be known. Focus on the innervation, blood supply,
and the relationship between the tendons of the flexors and extensors.
DORSAL SCAPULAR REGION
Superior: along the side of the acromion to the 7th cervical vertebra.
Medial: the midline of the body.
Inferior: along the side of the inferior angle of the scapula (transverse line).
Lateral: a longitudinal line from the acromion.
SKIN INNERVATION:
Dorsal rami or the spinal nerves.
Removing the skin reveals a fascia covering the trapezius muscle . Know the origin and insertion of the
trapezius. Below the trapezius, the latissimus dorsi muscle is found at the inferior part of the region as well
as the teres major muscle.
Beneath the trapezius muscle, there are other muscles too, namely the supraspinatus (above), the
infraspinatus (below), and the teres minor.
At the lateral border of the region, you can see the long head of the triceps (separating the triangular and
quadrangular spaces from each other).
The main structure of the region is the suprascapular artery which comes from the subclavian artery, and
passes through the region above the superior transverse scapular ligament. The suprascapular nerve comes
together with the artery passing through the superior scapular foramen (below the superior transverse
ligament). These two structures innervate the supraspinatus and infraspinatus muscles. Both structures,
after passing through the superior scapular foramen, pass through the inferior scapular foramen to the
infraspinous fossa.
In the neck of the scapula, there is an anastomosis between the suprascapular artery and the circumflex
scapular artery (from the median axillary hiatus). So finally, this is an anastomosis between the axillary
artery and the subclavian artery because the circumflex scapular artery comes from the axillary and the
suprascapular from the subclavian.
In the superior part of the region, you can see the levator scapulae muscle coming from the nuchal region.
The dorsal scapular nerve innervates the levator scapulae (C3 & C4) and comes together with the dorsal
scapular artery.
The rhomboid muscles move the scapula backward and the levator scapulae elevates the scapula.
13
LOWER LIMB
GLUTEAL REGION
Superior: along the side of the iliac crest.
Inferior: along the side of the gluteal sulcus.
Lateral: along the side of the greater trochanter.
SKIN INNERVATION:
Superior, middle, and inferior clunial nerves.
The inferior clunial nerves come from the posterior femoral cutaneous nerve (from the sacral plexus).
The sacral plexus comes from the ventral rami of the sacral nerves. The superior and middle clunial nerves
are dorsal branches of the first three lumbar and first three sacral spinal nerves, respectively.
If you remove the skin, you will find the gluteal fascia which covers the gluteus maximus muscle and the
anterior part of the gluteus medius muscle. The gluteus medius is not covered totally by the gluteus
maximus. Gluteus medius is also the muscle for intramuscular injections. Injections are done there
because there is no artery or nerve to injure. In children, injections are made on the thigh (quadraceps
femoris).
The gluteal fascia goes into the muscle fibers (very thick-- rough).
The gluteus maximus arises from the iliac bone behind the posterior gluteal line, the sacrum, the dorsal
sacroiliac ligament, sacrotuberal ligaments, and the thoracolumbar fascia. It is inserted to the gluteal
tuberosity of the femur and to the iliotibial tract. Its main function is extension of the hip joint, and it is
innervated by the inferior gluteal nerve.
If you cut the gluteus maximus, you can see the gluteus medius, piriformis, gemellis superior and inferior,
the obturator internus, and the quadratus femoris muscles.
The sacral plexus has two parts. The upper part is called the sciatic plexus, and the lower part is called
the pudendohemorrhoidal plexus. The sciatic plexus arises from the lower half of the fourth lumbar
segment (5th, sacral 1st and 2nd segments and the upper half of the 3rd segment of the spinal cord.
Branches of the sciatic plexus are: sciatic nerve, posterior femoral cutaneous nerve, superior gluteal
nerve, inferior gluteal nerve, and muscular branches innervating the piriformis, gemelli, obturator internus,
and quadratus femoris muscles.
The lower part of the sacral plexus (pudendohemorrhoidal plexus) arises from the 3rd and 4th sacral
segments, but it receives also branches from the 1st and 2nd sacral segments too.
The inferior gluteal nerve and artery supply the gluteus maximus muscle.
The sciatic nerve runs down and innervates almost the whole lower limb (except the adductors and
extensors of the thigh).
The pudendal nerve comes out from the infrapiriform hiatus and turns back through the lesser sciatic
foramen into the ischiorectal fossa (3rd semester).
The internal pudendal artery comes from the internal iliac artery.
The gluteus medius muscle arises from the outer surface of the iliac bone between the anterior and
posterior gluteal lines, and it is inserted to the fossa trochanterica.
14
The suprapiriform and infrapiriform hiatuses are the two parts of the greater sciatic foramen divided by
the piriformis muscle. Borders of the greater sciatic foramen are: superoanterior (greater sciatic notch),
posterior (sacrotuberal ligament), and inferior (sacrospinal ligament).
Structures passing through the suprapiriformis hiatus:
1) Superior gluteal artery.
2) Superior gluteal nerve.
Structures passing through the infrapiriformis hiatus:
1) Inferior gluteal artery.
2) Inferior gluteal nerve.
3) Sciatic nerve.
4) Posterior femoral cutaneous nerve.
5) Pudendal nerve.
6) Internal pudendal artery (from internal iliac).
Structures passing through the lesser sciatic foramen:
1) Obturator nerve.
2) Inferior pudendal artery.
3) Pudendal nerve.
4) Tendon of the obturator internus.
If you cut the gluteus medius muscle, you can see the gluteus minimus muscle which originates between
the anterior and inferior gluteal lines of the iliac bones. The function of the gluteus medius is abduction of
the hip joint. The movements are similar to the movements of the deltoid muscle: if the anterior fibers
act, it is a medial rotator; if the posterior fibers act, it is a lateral rotator, and if all of them act together, it is
an abductor.
If the gluteus medius acts on the pelvis, it balances the pelvis.
The gluteus minimus helps in abduction and in medial rotation.
The obturator internus arises from the inner surface of the obturator foramen. The tendon of this
muscle passes through the lesser sciatic foramen and turns around the lesser sciatic notch. From the notch,
it runs forward and lateral. Its function is lateral rotation of the thigh. The tendon of the obturator internus
is surrounded by the gemellus muscles. They arise from the lesser sciatic notch, and they are inserted to the
trochanteric fossa.
Below the gemellus muscles and obturator internus muscle, lies the quadratus femoris muscle, between
the tuber ischiadicum and greater trochanter (quadrangular shaped muscle).
Between the gluteus maximus and greater trochanter, find the trochanteric bursa.
POSTERIOR FEMORAL REGION
Superior: gluteal line.
Inferior: three fingers above the popliteal sulcus.
Lateral: along the side of the trochanter major.
Medial: from the medial end of the gluteal sulcus to the medial epicondyle of the femur.
SKIN INNERVATION:
Posterior femoral cutaneous nerve.
Beneath the skin, there is a fascia which the fascia lata. This fascia surrounds the posterior femoral
cutaneous nerve. IT IS THE ONLY PLACE WHERE A CUTANEOUS NERVE IS LOCATED INSIDE THE FASCIA.
Before removing the fascia, dissect the nerve.
15
After removing the fascia, you can find the flexor muscles of the thigh, arising from the tuber
ischiadicum, except the short head of the biceps femoris (medial lip of the linea aspera). The biceps
femoris runs to the lateral side of the femur, but the semitendinosus and semimembranosus run to the medial
side. The biceps is inserted to the head of the fibula, while the semitendinosus and semimembranosus insert
to the pes anserinus, and then to the tibia.
Some sources recognize a single pes anserinus into which the sartorius, gracilis, semitendinosus, and
semimembranosus insert. Others distinguish a pes anserinus profundus, the insertion of the semimembranosus, and a
pes anserinus superficialis, the insertion of the other three. One of the MRT questions asks about the p. a.
superficialis, so be familiar with both forms!
Between the muscles, the sciatic nerve lies exactly in the midline of the thigh. The sciatic nerve
innervates the flexors of the thigh and divides into the common peroneal (aka. fibular) nerve and the tibial
nerve. This division is usually at the end of the region, but sometimes is higher.
The most superficial structure between the muscles is the sciatic nerve. Next, are the popliteal vein and
artery (usually we have vein-artery-nerve, but here is opposite) because the vein and the artery come from the
adductor canal (through the adductor hiatus).
In the lower part of the region, the adductor hiatus is formed by the adductor magnus near the medial
epicondyle of the femur. The muscle fibers are inserted to the medial margin of the femur. The tendon
and the muscle fibers form and arch-shaped hiatus which is the outlet of the adductor canal (leading to the
popliteal fossa).
Borders of the adductor hiatus:
Superior: muscle fibers of the adductor magnus.
Lateral: Femur (medial border).
Medial: tendon of the adductor magnus.
The femoral artery gives rise to the profunda femoris artery that gives proliferating branches to supply
the flexor muscles and also the medial and lateral circumflex femoral arteries. The lateral supplies the
extensors and the medial supplies the adductors (together with the obturator artery).
POPLITEAL REGION
Superior: three fingers above the popliteal sulcus.
Inferior: three fingers below the popliteal sulcus.
Medial: along side the medial epicondyle of the femur.
Lateral: along side the lateral epicondyle of the femur.
SKIN INNERVATION:
Superior part of the region: Posterior femoral cutaneous nerve.
Inferior part of the region: Medial and Lateral sural cutaneous nerves.
SUPERFICIAL STRUCTURES:
Vena saphena parva (between the fascia and the skin).
The lateral and medial sural cutaneous nerves accompany the vena saphena parva ("small") and finally
form the sural nerve. The lateral comes from the common peroneal nerve and the medial from the tibial
nerve. The sural nerve then goes behind the lateral malleolus and enters the dorsum of the foot (giving the
lateral calcanean branch and the lateral dorsal cutaneous branch to the little toe).
Deep to the popliteal fascia (continuation of the fascia lata), you can find the same structures seen in the
posterior femoral region: 1)common peroneal and tibial nerves, 2)popliteal vein, and 3)popliteal artery (from
lateral to medial).
16
The POPLITEAL FOSSA is a diamond-shaped fossa covered by the popliteal fascia. The base-floor of the
fossa is the popliteus muscle (below), the posterior part of the articular capsule of the knee joint (middle
part), and the femur-popliteal fossa (above):
Superior and medial: semitendinosus and semimembranosus.
Superior and lateral: biceps femoris.
Inferior and medial: medial head of the gastrocnemius.
Inferior and lateral: lateral head of the gastrocnemius.
The popliteal muscle is the deepest muscle and comes from the lateral epicondyle of the femur. It
inserts to the popliteal line of the tibia.
The tibial nerve descends into the posterior crural region and innervates the flexors of the leg.
The peroneal nerve becomes superficial and turns around the neck of the fibula, goes below the origin of
the peroneus longus muscle, and divides into the superficial and deep peroneal nerves. The superficial
remains in the peroneal compartment and the deep goes to the extensor compartment to supply the extensor
muscles.
Because of the place of the common peroneal nerve (superficial at the level of the neck of the fibula), the
injury of the nerve is very frequent; usually with the fracture of the fibula. The result of the injury of the
common peroneal nerve is the "horse foot" (patient cannot extend the foot) pes equinus + pes varus (peroneal
muscles). Together (superficial and deep) = pes equinovarus.
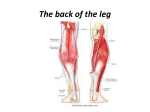
POSTERIOR CRURAL REGION
Superior: three fingers below the popliteal sulcus.
Inferior: a line connecting the medial and lateral malleoli.
Medial: a line from the medial epicondyle to the medial malleolus.
Lateral: a line from the lateral epicondyle to the lateral malleolus.
SKIN INNERVATION:
Medial and lateral sural cutaneous nerves + the sural nerve.
If you remove the skin, you will find the vena saphena parva together with the sural nerve (found in the
midline of this region and go behind from the lateral epicondyle). The vena saphena parva arises from the
plexus venosus dorsalis pedis and runs behind the lateral epicondyle to the posterior surface of the leg.
The fascia is called the posterior crural fascia, and it sends two septa to the fibula: anterior and posterior
intermuscular septa. These septa form the peroneal compartment of muscles. The crural fascia sends also
another layer to the anterior surface of the tibia: the tibial septum. Between the tibial septum and the
anterior intermuscular septum, we have the extensor compartment. The posterior intermuscular septum and
the tibial septum form the flexor compartment.
Removing the fascia reveals the muscles of the triceps surae (medial and lateral heads of the gastrocnemius muscle and the soleus muscle) in the superficial layer. The soleus muscle arises from a
tendinous arch which is between the tibia and the fibula. Below this tendinous arch, we can see the tibial
nerve and the posterior tibial artery and vein (they are covered by the soleus muscle, so you have to cut this
muscle to see the main structures of this region).
THREE DEEP MUSCLES: the most lateral is the flexor hallucis longus, the middle one is the tibialis
posterior, and the most medial is the flexor digitorum longus. The tibialis posterior arises a little below the
other two. So, in the uppermost part of the region, the flexor hallucis longus and the flexor digitorum
longus can be seen next to each other. There, the tibial nerve and the posterior tibial artery and vein, are
found between the flexor digitorum longus and the flexor hallucis longus. In the lower part of the region,
these structures can be found between the flexor hallucis longus and the tibialis posterior muscle.
The tibial nerve comes from the sciatic nerve and innervates the flexor muscles by muscular branches.
17
The posterior tibial artery gives a branch here, the peroneal artery. This artery goes below the flexor
hallucis longus muscle between it and the fibula (it supplies this muscle).
The tibial nerve and posterior tibial artery go behind the medial malleolus and run to the sole. The tibial
nerve forms the medial and lateral plantar nerves, and the posterior tibial artery forms the medial and lateral
plantar arteries.
The tibialis posterior muscle and the flexor digitorum longus cross each other approximately 3 fingers
above the medial ankle. So, after the crossing, the flexor hallucis longus remains the most lateral, the
middle becomes the flexor digitorum longus, and the most medial will be the tibialis posterior. The flexor
digitorum longus is the crosser, thus it will be the most superficial.
MEDIAL MALLEOLAR REGION
This region is located between the medial malleolus and the calcaneus. Deep to the skin, the vena
saphena magna (in front of the medial malleolus) runs in the anterior margin of the region. The VSM is
found together with the saphenous nerve, but usually the saphenous nerve doesn't go down behind the medial
ankle.
The tendons are covered by the flexor retinaculum which keeps the tendons close to the bones. The first
tendon is the tibialis posterior tendon (exactly behind the ankle). The middle one is the flexor digitorum
longus (crossing the tibialis posterior above the medial ankle). Then, we have the posterior tibial artery,
accompanied by the two psoterior tibial veins and the tibial nerve. The last structure is the tendon of the
flexor hallucis longus muscle.
Here, there are tendon sheathes surrounding the three tendons.
LATERAL MALLEOLAR REGION
SUPERFICIAL STRUCTURES:
The vena saphena parve, coming from the plexus venosus dorsalis pedis and going behind the lateral
malleolus; the sural nerve (from medial and lateral sural cutaneous nerves).
The sural nerve goes behind the lateral malleolus and gives the lateral dorsal cutaneous nerve. This
nerve innervates the skin of the lateral side of the foot and the lateral margin of the little toe.
Remove the fascia to expose the penoneus longus and brevis muscles. These are held down by the
superior and inferior peroneal retinacula (forming and "X" or "Y" shape). Beneath the peroneal retinacula,
in a common tendon sheath, are the long and short peroneus muscles. The peroneus brevis is attached to the
base of the 5th metatarsal, and the peroneus longus is attached to the base of the 1st metatarsal and to the
medial cuneiform (sulcus peronei longus). The peroneus longus is covered by the long plantar ligament in
the plantar region.
The two retinacula are connected to the lateral malleolus and to the calcaneus.
The main function of the peroneus longus is holding the foot. It makes an arch together with the tibialis
anterior muscle (inserting to the same place).
DORSAL PEDIS REGION
Superior: a line connecting the medial and lateral malleoli.
Inferior: the root of the toes.
Medial: a line from the medial malleolus to the first toe or the medial margin of the foot.
18
Lateral: a line from the lateral malleolus to the fifth toe or the lateral margin of the foot.
SKIN INNERVATION (the most important region for this!):
The superficial peroneal nerve enters the dorsal pedis region and divides into two branches: the medial
and intermediate dorsal cutaneous branches. The medial dorsal cutaneous nerve innervates the medial
border of the first toe, the lateral border of the second and the medial half of the third toe. The intermediate
dorsal cutaneous nerve innervates the lateral half of the third toe, the fourth and the medial half of the 5 th toe.
The lateral side of the fifth toe is innervated by the lateral dorsal cutaneous nerve (coming from the sural
nerve). The lateral side of the second toe and the medial side of the second toe are innervated by digital
branches of the deep peroneal nerve. So, there are four nerves innervating the dorsal side of the foot.
The deep peroneal nerve becomes superficial from below the tendons of the extensor hallucis longus and
brevis.
Together with the cutaneous nerves, we have the plexus venosus dorsalis pedis from which the vena
saphena magna + parva drain blood.
Beneath the superficial structures, lie the retinaculum extensorum superior and inferior. The superior
extensor retinaculum is at the superior border of the region. The two retinacula hold down the extensor
tendons. The extensor tendons are the extensor hallucis longus muscle, the extensor digitorum muscle, and
the tendon of the peroneus tertius (inserting to the base of the fifth metatarsal).
This region also includes the extensor digitorum brevis and the extensor hallucis brevis. The tendons of
the extensor digitorum brevis are inserted to the middle phalanges of the lateral four toes. The extensor
digitorum longus tendons are inserted to the distal phalanges of the lateral four toes.
An important structure in this region is the dorsalis pedis artery. It comes from the midpoint of the line
connecting the medial and lateral ankle toward the first interosseal space. You can palpate the artery
because it is on the cuneiform bone (you can palpate the pulse in the limbs from the radial artery, the
posterior tibial artery, and the dorsalis pedis artery).
The dorsalis pedis artery will form the arcuate artery beneath the tendons which is closed by the lateral
tarsal artery (from the anterior tibia). The dorsalis pedis artery pierces through the first interosseal space
and closes the plantar arch. From the anterior tibial artery, we have several malleolar branches to supply the
ankle joint:
Anterior: Medial and lateral malleolar arteries.
Posterior: Medial and lateral malleolar arteries.
From the arcuate artery, the dorsal metatarsal arteries arise and will give the proper plantar digital
arteries.
19
SUBINGUINAL REGION
Superior: a line along the inguinal ligament.
Inferior: a line along the sulcus gluteus (anterior).
Lateral: a line from the anterior superior iliac spine.
Medial: a vertical line from the pubic tubercle.
SKIN INNERVATION:
Anterior femoral cutaneous nerve, Lateral femoral cutaneous nerve (coming from the lumbar plexus
approximately one cm below the anterior superior iliac spine), Femoral branch of the genitofemoral nerve,
and Ilioinguinal nerve.
The genitofemoral nerve arises from the lumbar plexus and divides into two branches: a)Genital, and
Femoral. The genital branch passes through the inguinal canal, and the femoral branch passes through the
lacuna vascerum of the subinguinal hiatus, pierces through the fascia lata, and becomes superficial to
innervate a small part of the skin below the inguinal ligament.
The medial part of the region is innervated by the ilioinguinal nerve (passing through the inguinal canal).
Mainly, it belongs to the inguinal region, but a small part belongs to the subinguinal region.
b)
SUPERFICIAL STRUCTURES:
Vena saphena magna (piercing through the fascia lata through the cribiform lamina which is called the
hiatus saphenous). Together with the vena saphena magna, we have the superficial nerves at the same level.
Tiny arteries come out from the hiatus saphenous (superficial epigastric artery, superficial circumflex iliac
artery, and external pudendal artery).
The main part of the superficial epigastric artery is in the inguinal region, and the circumflex is between
the two regions.
Right beneath the skin, we have inguinal lymph nodes located into two lines: one parallel to the inguinal
ligament (superficial) and one parallel to the vena saphena magna (and deep, parallel to the femoral vein and
artery). So, the vertical line of the lymph nodes is in two layers, one superficial and one deep. Both lines
form a letter "T".
The lymph nodes parallel to the inguinal ligament collect lymph from: Anterior abdominal wall
(below the umbilicus), Gluteal region, Perineal region, External genitalia, Anal opening,
Vestibulum vaginae, and Fundus of the uterus.
The lymph nodes parallel to the veins and artery (the vertical line) collect lymph from the lower limb.
The fascia lata ensheathes three muscles: a)Sartorius, b)Gracilis, and c)Tensor fascia latae. On the fascia,
there is a hiatus called the hiatus saphenous. Below the fascia, you will see the extensor muscles and the
adductors: the sartorius, and quadriceps femoris (only the rectus femoris arises from the anterior inferior iliac
spine; all the vastus heads arise from the femur).
At the medial side of the region, you can see the first part of the adductor muscles: Adductor longus,
gracilis, and the pectineus.
The main structure of this region is the femoral canal. Below the inguinal ligament, there is an opening
called the subinguinal hiatus. It is formed by the inguinal ligament and by the iliac bone below the anterior
superior iliac spine, and the superior ramus of the pubic bone.
Borders: Superior and anterior (inguinal ligament-- fascia lata), Posterior (superior ramus of pubis and the
anterior superior iliac spine.
The iliopsoas muscle passes through this hiatus to the thigh, together with the femoral nerve. This
lateral compartment of the subinguinal hiatus is called lacuna musculonervosum and is separated from the
lacuna vasorum (middle compartment) by the arcuate ligament or arcus iliopectineus. This is a tendinous
arch that comes from the inguinal ligament and goes to the pecten ossis pubis.
The middle part is the lacuna vasorum having the femoral vein and artery inside. It is surrounded by a
fibrous sheath (a connective tissue sheath).
20
The most medial part is called the lacuna lymphatica (inlet of the femoral canal). Medially, it is
bordered by the lacunar ligament that rounds the sharp angle (Tájanatómia p. 60). Inside this annulus
femoralis (femoral ring), there is a lymph node called the lymphatic node of Rosenmüller. This ring is not
exactly a foramen. It is covered by a septum: the FEMORAL SEPTUM, which is pierced by the lymph vessels
passing through the canal going to the abdominal cavity.
Walls of the femoral canal:
Lateral: Femoral vein.
Medial: Pectineus muscle and pectineal fascia (covering the muscle).
Anterior: Fascia lata.
Inlet: Femoral ring (covered by the femoral septum).
Outlet: Hiatus saphenous.
The femoral canal is a short canal, 3cm only, and it extends from the femoral ring (at the level of the
inguinal ligament) to the hiatus saphenous. The femoral canal is not a real canal. It is called a canal only
if a hernia occurs (the small intestine or something from the abdominal cavity passing though the canal).
The femoral canal is filled with loose connective tissue and lymphatic vessels.
If you describe the femoral canal as an anatomical structure, you should say that it includes the femoral
artery and vein and the hernial canal. So, in this case, the femoral canal contains the femoral blood vessels
and lymph vessels inside. The borders are:
Medial: Pectineus muscle.
Lateral: Iliopsoas muscle.
Both of them are covered by a fascia which continues with each other, becoming a fossa called the
iliopectineal fossa (triangular shaped fossa) containing the femoral vein and artery and the hernial canal itself
(at the medial part).
The FEMORAL TRIANGLE is made by the sartorius muscle (lateral), the adductor muscles, and the inguinal
ligament. It contains the iliopectineal fossa (with the blood vessels and the hernia canal). The femoral
artery gives a branch here; the deep femoral artery (profunda femoris artery), that gives three branches:
Medial circumflex femoral artery (together with the obturator artery, supplying the adductors),
Lateral circumflex femoral artery (supplying the extensors of the thigh),
Perforating branches (supplying the flexors of the thigh).
The medial circumflex femoral artery anastomoses with the obturator artery and the lateral circumflex
femoral artery, with the superior and inferior gluteal arteries.
The femoral nerve has anterior cutaneous branches that pierce the fascia lata and supply the skin. It also
has a long branch that goes inside the adductor canal called the saphenous nerve.
The adductor brevis is covered by the pectineus and the adductor canal.
21
ANTERIOR FEMORAL REGION
Superior: an anterior line from the gluteal sulcus,
Inferior: 2-3 fingers above the patella,
Medial: a line from the gluteal sulcus to the medial epicondyle of the femur,
Lateral: a line from the greater trochanter to the lateral epicondyle.
SKIN INNERVATION:
Anterior femoral cutaneous nerves, Lateral femoral cutaneous nerves (lateral part of the region, and
Obturator nerve (lower-medial part of the region)(LUMBAR).
Deep to the skin, you can find the fascia lata. Between the skin and the fascia, run the vena saphena
magna, cutaneous branches of the femoral nerve, and the lateral femoral cutaneous nerves. The vena
saphena magna runs in the medial side of the region and ascends to the subinguinal region.
The lateral femoral cutaneous nerve comes about 1 cm below the anterior superior iliac spine, coming
from the sacral plexus.
If you remove the fascia lata, be aware that the sartorius muscle is ensheathed by the fascia together with
the gracilis and the tensor fasciae latae.
At the lateral side of the region is the iliotibial tract, the thickened lateral part of the fascia lata. It is
inserted to the tibia from the iliac crest.
Removing the fascia, we will see the extensor muscles: QUADRACEPS FEMORIS (rectus femoris, vastus
lateralis, vastus intermedius, vastus medialis). The adductor group is medial to the extensor muscles. The
adductor longus, together with the sartorius and the inguinal ligament, form the femoral or subinguinal
triangle (previously discussed).
The main part of the pectineus is in the subinguinal region, so you will see only the inferior part of this
muscle. The adductor magnus is beneath the adductor longus and gracilis muscles.
Between the adductor muscles and the extensor muscles, we will see the adductor canal:
Walls:
Medial: adductor longus and magnus,
Lateral: vastus medialis,
Anterior: lamina vastoadductoria (connects the adductor longus and
magnus with the vastus medialis.
The adductor canal goes to the popliteal fossa and has the femoral vein and artery inside as well as the
saphenous nerve. The saphenous nerve pierces through the anterior wall through the lamina
vastoadductoria and joins the vena saphenous magna. The descending genicular artery also pierces through
the lamina vastoadductoria and supplies the knee joint.
The outlet of the adductor canal is located in the popliteal fossa and is called the adductor hiatus.
The femoral artery has a branch here coming from the subinguinal region and is called the profunda
femoris artery (see above).
The main structure here is the adductor canal.
22
ANTERIOR GENICULAR REGION
Inferior: three fingers below the patella,
Superior: three fingers above the patella,
Medial: the line along the medial epicondyle,
Lateral: the line along the lateral epicondyle.
SKIN INNERVATION:
Anterior femoral cutaneous nerves (superior part), Obturator nerve (medial part), Saphenous nerve
(inferior part), and Lateral femoral cutaneous nerve (lateral part).
There are three groups of bursae: a) suprapatellar bursae, b) prepatellar bursae, and c) infrapatellar
bursae. In the prepatellar group, there is a bursa right beneath the skin called the subcutaneous prepatellar
bursa (between the skin and the fascia). The next bursa is between the fascia and the tendon and is called
the subfascial prepatellar bursa. The third one is between the tendon and the patella and is called the
subtendineal prepatellar bursa.
To see the suprapatellar bursa, you must open the joint (so it won't be seen in a regional study).
Beneath the skin, you will find the quadriceps femoris muscle (the common tendon). The continuation
of the tendons of the four heads of the quadriceps femoris form the patellar ligament and the medial and
lateral patellar retinacula. The patellar ligament is inserted to the tuberosity of the tibia and the medial and
lateral retinacula, to the medial and lateral condyles of the tibia.
The adductor magnus is inserted to the medial epicondyle, so at the medial part of the region, you will see
its tendon.
So, we will also see the descending genicular artery (from the genicular artery) coming from the anterior
femoral region, the vena saphena magna, and the saphenous nerve.
The pes anserinus is located at the medial part of the region (medial is the ligamentum patellae) and is a
triangular shaped tendon formed by the insertion of the sartorius, gracilis, and semitendinosus muscles.
The common function of these three muscles is medial rotation of the knee joint.
ANTERIOR CRURAL REGION
Superior: three fingers below the patella,
Inferior: the line connecting the medial and lateral malleoli,
Medial: a line connecting the medial epicondyle and the medial malleolus,
Lateral: a line connecting the lateral epicondyle and the lateral malleolus.
SKIN INNERVATION:
Saphenous nerve (in front), Lateral sural cutaneous nerve (lateral part), Obturator nerve (upper and
medial parts), and Superficial peroneal nerve.
Removing the skin, we will find the fascia cruris. It gives a septum between the extensors and peroneus
muscles (at the anterior margin of the fibula) and it also gives a septum at the posterior margin of the fibula.
These two are called the anterior and posterior intermuscular septa.
SUPERFICIAL STRUCTURES:
The vena saphenous magnus (at the medial part of the region) coming from the plexus venous dorsalis
pedis if front of the medial ankle; Superficial peroneal nerve, coming out from the peroneal compartment
between the middle and inferior third of the region and divides into medial and intermediate dorsal cutaneous
nerves.
Below the fascia, you will see the extensor muscles and the peroneus muscles.
23
Extensors: Extensor digitorum (most lateral), tibialis anterior, and (deep to and between the first two)
extensor hallucis muscles. The tibialis anterior arises from the tibia and the interosseous membrane, but the
extensor hallucis longus muscle arises a little deeper than the extensor digitorum longus and tibialis anterior.
So, at the superior part of the region, only the tibialis anterior and the extensor digitorum longus will be seen.
The deep peroneal nerve and the anterior tibial artery (with the two veins) between these two muscles.
The deep peroneal nerve comes from the common peroneal nerve and pierces through the anterior
intermuscular septum (between peroneal muscles and extensor digitorum longus) to enter the anterior
compartment. In the inferior part of the region, the nerve, veins, and artery are located between the extensor
hallucis longus and the tibialis anterior muscles.
The anterior tibial artery gives muscular branches and also recurrent branches to supply the knee joint.
Peroneus muscles: Both originate from the lateral surface of the shaft of the fibula. The peroneus
longus is superficial, has a shorter muscle body (but longer tendon), and inserts to the base of the first
metatarsal and the medial cuneiform. The peroneus brevis is deep, has a broader, thicker muscle belly, and
inserts to the base of the fifth metatarsal. They are innervated by the other division of the common
peroneal nerve the superficial peroneal nerve, which runs between the peronei and the extensor digitorum
longus.
PLANTAR REGION
Superior: calcaneus,
Inferior: roots of the toes,
Medial: medial border of the sole,
Lateral: lateral border of the sole.
You should use a knife to remove the skin (~1 cm) in this region. The skin in this region has adipose
compartments in the subcutaneous layer. These adipose compartments function as shock absorbers and also
as a protector for the nerves and arteries that are found in the sole.
Removing the skin, the next structure is the plantar aponeurosis, arising from the tuber calcanei and
covering the middle part of the plantar region. It sends two septa (medial and lateral intermuscular septa)
which define medial, lateral, and middle groups of muscles. These groups are called lateral, intermediate,
and medial eminences (analogous to thenar, mesothenar, and hypothenar areas of the palm). The medial and
lateral eminences are covered by a fascia which is a continuation of the plantar aponeurosis.
Deep to the plantar aponeurosis, you can see the nerves and arteries of the plantar region that are
branches of the medial and lateral plantar arteries and of the medial and lateral planter nerves. The medial
plantar nerve innervates the medial 3½ toes by common and proper digital planter nerves and the lateral
plantar nerve innervates the lateral 1½ toes also by common and proper digital plantar branches (analogous to
palmar innervation). Both are branches of the tibial nerve.
Together with the nerves, there are the plantar arteries with the same names coming from the plantar arch.
In the medial plantar sulcus (between the abductor hallucis and flexor digitorum brevis), find the medial
plantar artery and nerve. In the lateral plantar sulcus (between the flexor digitorum brevis and quadratus
plantae), find the lateral plantar artery and nerve (and the first portion of the plantar arch).
The plantar arteries arise from the posterior tibial artery, and the plantar nerves arise from the tibial
nerve. The posterior tibial artery and the tibial nerve pass behind the medial ankle, and you should cut the
abductor hallucis to see them.
The first layer in the intermediate eminence is the aponeurosis plantaris, then the flexor digitorum brevis.
If you remove the flexor digitorum brevis, you will see the flexor digitorum longus muscle, together with the
lumbricals, and the quadratus plantae inserting in the tendons of the flexor digitorum longus. The
quadratus plantae corrects the movements of the flexor digitorum longus because the direction of this muscle
is a little medial to lateral, and the direction of the quadratus plantae is lateral to medial.
The medial plantar artery supplies only the first toe and the medial side of the second toe. To reveal the
next part of the plantar arch, cut the flexor digitorum longus. To see the last portion of the plantar arch, cut
24
the oblique head of the adductor hallucis (arising from the base of the metatarsal bones and covering the
plantar arch). The transverse head arises from the heads of the 3rd, 4th, and 5th metatarsals. Both the
transverse and the oblique heads are inserted to the proximal phalanx of the 1st (big) toe.
The plantar arch is closed by the dorsalis pedis artery. This arch gives the common and proper digital
plantar arteries.
The lateral plantar nerve innervates the abductor and flexor digiti minimi, the adductor hallucis, the
quadratus plantae, the last 2 or 3 lumbricals, and all the interosei muscles.
In the last layer, you can find the interosseous muscles and the long plantar ligament above the interosseous muscles, covering the tendon of the peroneus longus muscle.
Then, we can speak about the muscles of the medial and lateral eminences. In this region, the layers of
the muscles in the intermediate eminence are the most frequently asked. So:
1st layer: Aponeurosis plantaris,
2nd layer: Flexor digitorum brevis,
3rd layer: Flexor digitorum longus, lumbricals, and quadratus plantae,
4th layer: Adductor hallucis, interosseous muscles, and the long plantar ligament,
5th layer: Tendon of the peroneus longus muscle.
In the medial and lateral eminences, we don't have layers.
In the superior part of the region, the flexor digitorum longus crosses the flexor hallucis longus. The
flexor digitorum longus is the crosser (the same as in the posterior crural region).
25
SKULL
The frontal bone has a frontal part called the squama ossis frontalis and an orbital part which is
composed by the orbital plane (or lamina) having a orbital surface (lower) and a cerebral (upper) surface.
The frontal lobe of the brain is located in the anterior cranial fossa on the cerebral surface of the orbital
plane. Between the orbital parts, the nasal part of the frontal bone forms the groove of the nasal cavity
(above the nasal bone, the roof of the nasal cavity; inside this part is the frontal sinus). The middle portion,
between the supraorbital lines (or above the supraciliary margins), is smooth and called the glabella (it means
smooth with no hair). The glabella is the anterior wall of the frontal sinus, so the sinus can be reached by
piercing it. The frontal sinus opens into the nasal cavity.
Paranasal sinuses are located around the nasal cavity and open into it. They are filled by air and lined
by mucous membrane on the inner surface. One of these sinuses is the frontal sinus that has a process
which is called zygomatic process. It is attached to the frontal process of the zygomatic bone.
Between the orbital lamina and behind the nasal part, lies the ethmoid bone. It has the cribiform plate
(or lamina) and the crista galli. The lamina cribrosa forms the horizontal plate of the ethmoid bone, making
it a T-shaped bone. The continuation of the crista galli below the cribiform plate is the perpendicular plate
which forms the septum nasi (the vomer joins the perpendicular plate to form the main inferior-posterior part
of the nasal septum). Thus, the nasal septum contains two bones.
The ethmoid bone has another lamina which is the orbital lamina (or lamina papyracea: thin like paper).
One more surface covers the air cells (cellule ethmoidale) that communicate with each other forming a sinus
called the ethmoid sinus. This sinus also opens into the nasal cavity.
If someone suffers an inflammation in these sinuses, the voice will be changed (hose-like sound). These
air cells are between the orbital cavity and the nasal cavity. They are separated from the orbital cavity by
the orbital lamina of the ethmoid bone and from the nasal cavity by this rough surface of the ethmoid bone to
this nasal surface which is not a straight place, but a rough surface. To this nasal surface, the two nasal
conchae (superior and middle nasal conchae) attach. It is easier to understand in a frontal section through
the sinuses.
The concha nasalis inferior is a separate bone, and it is attached to the maxilla and the palatine bone.
The concha nasalis media and c. n. superior arise from the nasal surface of the perpendicular plate of the
ethmoid. The superior concha is very short, and you can find it only in the posterior part of the nasal cavity.
The middle and inferior concha are much longer.
The meatus nasi superior and meatus nasi media are between the conchae and the ethmoid bone. Below
the concha inferior, there is a meatus nasi inferior.
The maxilla has a maxillary sinus and a maxillary hiatus opening into the middle nasal meatus. A part
of this maxillary hiatus is covered by the concha (by the maxillary process of the inferior nasal concha). If
the inferior nasal concha is attached to the maxilla, the hiatus is just a tiny opening. This opening (hiatus
maxillaris) is on the superior part of the sinus. If there is fluid inside, it cannot come out because the
opening is at the top of the maxillary sinus (the patient should stand upside down for the fluid to drain out).
That's why infection of this sinus is so frequent. From the frontal sinus, infected fluid simply flows out and
downward into the maxillary sinus.
The cribiform plate is between the orbital plates of the frontal bone.
Behind the frontal bone, lies the sphenoid bone. Its main parts are the lesser wings, the greater wings,
and the body. The greater wing has different surfaces: Cerebral surface (related to the temporal lobe of
the cerebrum in the middle cranial fossa), Temporal surface, Infratemporal surface (the border between
26
the temporal and infratemporal surfaces is the infratemporal crest, at the level of the zygomatic arch),
Orbital surface.
The pterygoid process has two lamina: lateral and medial, and a body forming the sella turcica (Turkish
saddle). The middle of the sella is the hypophesial fossa. The Turkish saddle connects the two middle
cranial fossae in the midline.
Between the ala minor and major ("wings"), there is fissure called the superior orbital fissure. There is
also an inferior orbital fissure (if you look inside the orbital cavity). The superior orbital fissure connects
the orbital cavity with the middle cranial fossa, and it contains the cranial nerves III, IV, V 3, & VI and the
superior ophthalmic vein (taking blood into the cavernous sinus, which is lateral to the Turkish saddle).
DURAL SINUSES:
The main veins of the brain inside the skull are different from the veins in the periphery, outside the skull.
The difference is that the wall of these veins is formed by dura mater. There is an important venous sinus
which is called sinus cavernosum. It is extremely important for two reasons: 1) the motor nerve of the eye,
the ophthalmic nerve, and the internal carotid artery pierce through this sinus, going to the superior orbital
fissure, 2) the superior ophthalmic vein (from the orbital cavity) has an anastomosis with the facial vein (main
vein of the face), and this anastomosis is here in the medial angle of the eye. An infection from the face
could be spread through the ophthalmic vein into the cavernous sinus, and the result could be paralysis of the
eye (because of the location of the motor nerve of the eye). This vein (the anastomosis) is called the
angular vein because it is at the medial angle of the eye.
Behind the superior orbital fissure, there is a round-shaped foramen called the foramen rotundum.
Through this foramen, the 2nd branch of the trigeminal nerve (maxillary nerve) passes. The foramen
rotundum leads to the pterygopalatine fossa.
Behind, there is an oval-shaped foramen called the foramen ovale. [Foramen rotundum is just behind the
fissure, and foramen ovale is a little behind and lateral.] The foramen ovale transmits the mandibular nerve.
Medial to f. ovale, there is an emissary foramen that is for veins connecting the inner surface of the skull with
the outer surface (accessory meningeal vein). In some skulls, this foramen is missing.
Posterior and lateral to the oval foramen, the foramen spinosus transmits the middle meningeal artery,
which is the main artery of the dura matter (outermost membrane of the skull). The sulci arteriosi is for the
middle meningeal artery. The sulci arteriosi is also called the sulcus of the middle meningeal artery.
These sulci start from the spinous foramen.
There is another tiny nerve; the meningeal branch of the mandibular nerve (not so important). The
spinous foramen is called that because this tiny posterior apex of the ala major is called spina ossis
sphenoidalis.
The temporal bone is irregularly shaped, and consists of two main parts: pars petrosa and pars
squamosa. The squamous part This pyramid is the part of the petrous temporal (pars petrosa) because of
the shape. The pyramid is the main part of the petrous temporal. The other part is the mastoid-styloid part.
Between the pyramid and the sphenoid bone, there is a big foramen called the foramen lacerum. This
foramen is not a real foramen in the living skull, because it is covered by a fibrous tissue membrane. It is
just a foramen in the bony skull. In this foramen, there are fissures for two tiny nerves: greater and lesser
petrosal nerves (coming out from the pyramid sheath). On the anterolateral surface of the pyramid, we have
two tiny hiatus called hiatus canalis nervi petrosi majoris and h.c.n. minoris. These sulci go on the anterior
surface of the pyramid, and they go out through the foramen lacerum. Medial to the foramen lacerum, there
is a sulcus (on the lateral side of the sella turcica) called the carotid sulcus, for the inner carotid artery. The
artery comes into the skull through the carotid foramen which is inside the pyramid. The inlet is called the
carotid foramen. The internal carotid artery arises in the skull making the sulcus caroticus. Then, it runs
through the cavernous sinus and divides into end branches, giving the ophthalmic artery and the middle +
anterior cerebral arteries for the brain. THE CAROTID CANAL IS THE MOST IMPORTANT STRUCTURE OF THE
SKULL.
The Turkish saddle (sella turcica) is bordered anteriorly by the sulcus prechiasmatis (chiasmatic sulcus)
and posteriorly by the tuberculum sellae. The two ends of this tubercle form two tiny clinoid processes
27
which are called the middle clinoid process. The two ends of the dorsum sellae form the posterior clinoid
processes. The back of the sella turcica is called the dorsum sellae (normally is elevated). The middle of
the sella is called the hypopheseal fossa. The clinoid processes are important because they point to the
hypopheseal fossa.
On the pyramid, the arcuate eminence (eminentia arcuata) is formed by the anterior semicircular canal of
the inner ear. Lateral to the eminentia arcuata and a little anterior, a very thin wall called tegmen tympani
forms the roof of the tympanic cavity. An infection can be spread into the cranial cavity through the thin
wall. The tegmen tympani has a process downward which is not visible because it is inside the pyramid and
is called the tegmental crest. This crest separates the squamous part from the tympanic part (because the
crest belongs to the petrous part of the temporal part). So, there are two fissures here. One is between the
tympanic and petrosa, called the fissura petrotympanica, and the other is between the petrosa and squamous
part, called the fissura petrosquamosa. The pterygotympanic fissure is more important because the chorda
tympani nerve (from the facial nerve) passes through.
In the superior margin of the petrosa bone is the sulcus for the sinus petrosus superior. This sinus drains
blood from the cavernous sinus into the sigmoid sinus.
At the apex of the pyramid, therer is an impression on the anterior surface called the trigeminal
impression (for the trigeminal ganglion). The trigeminal nerve divides into its three branches at this level.
The MIDDLE CRANIAL FOSSA is composed of the greater wing of the sphenoid (ala major), the
anterolateral surface of the pyramid of the temporal bone, and the squama of the temporal bone.
The POSTERIOR CRANIAL FOSSA is formed by the posteromedial surface of the pyramid, the basilar part of
the occipital bone (also called the clivus - "slope"), the lateral part of the occipital bone, and the squama of
the occipital bone. The borderline between the middle and posterior cranial fossae is the sulcus sinus
petrosis superioris and the dorsum sellae. Posteriorly, it is the sulcus sinus transversi. If you cut the
calvaria of the skull, cut it right above the external occipital protuberance.
The posterior cranial fossa is a closed fossa. It is closed by a dura in the horizontal plane which is a
double layer of the dura matter, called the tentorium cerebelle. This tentorium separates the cerebellum
from the occipital lobe of the cerebrum. The tentorium cerebelle is inserted to the sulcus sinus transversi
and to the sulcus sinus petrosi inferior. It has a notch called the tentorial notch (insisura tentorii) for the
mesencephalon brain, the pons, and the medulla.
The porus acusticus internus goes into the meatus acusticus internus. The meatus acusticus internus has
a ganglion inside. The facial nerve and the vestibulocochlear nerve pass through the porus acusticus
internus. Then, they divide in the floor of this meatus which is the fundus acusticus interni. Also, the
labyrinthine artery passes through on its way to the labyrinth (inner ear). So finally, we have: porus a.i.
meatus a.i. fundus a.i. division of the nerves.
The vestibulocochlear nerve goes to the labyrinth (for the vestibule and the cochlea), and the facial nerve
goes inside the facial canal which is also inside the pyramid bone. The first part of the facial canal is
vertical and perpendicular to the axis of the pyramidal bone (it is inside the bone). After this, the canal turns
backward and goes parallel to the axis of the pyramidal bone. This is the external genu of the facial canal.
The hiatus canalis nervi petrosi majoris starts at the genu of the facial canal because the nerve comes out of
the facial canal. After this second part of the canal, is goes downward. This is the perpendicular part, and
it comes out through the stylomastoid foramen. So, this foramen is the outlet of the facial canal. Here, the
facial nerve also gives a branch from the descending part which is the chorda tympani. It goes into the
tympanic cavity and comes out through the petrotympanic fissure. The inlet of the facial canal is the fundus
of the internal acoustic meatus.
The apertura externa aqueductus vestibuli is right behind the porus acusticus internus below this arcuate
eminence. (There are three semicircular canals: anterior, posterior, and lateral; that belong to the vestibular
organ [sensitive for the angular movement of the head]. The anterior canal makes the arcuate eminence).
Above the pore, we have the subarcuate fossa. More important is the jugular foramen. It is an "8"-shaped
foramen. The intrajugular process separates them into anterior and posterior foramina.
28
The jugular foramen is between the lateral part of the occipital bone and the petrous part of the temporal
bone. The anterior part of the foramen transmits the glossopharyngeal, vagus, and accessory nerves (CN IX,
X, XI). The posterior part transmits the internal jugular vein, which is the continuation of the sulcus sinus
transversi. This is the internal occipital protuberance, the crista occipitalis interna, and the sulcus sinus
sagitalis superioris from the calvaria.
Another very important canal is the hypoglossal canal crossing the occipital condyle. It is an oblique
canal which crosses the occipital condyle through the lateral part of the occipital bone. It runs from
posteromedial to anterolateral. It transmits the hypoglossal nerve (CN XII).
There is another canal called the condylar canal. It is parallel to the occipital condyle. It transmits the
emissary veins. Sometimes, it doesn't exist. Sometimes, it is very small.
Through the foramen magnum, the following structures pass through (most important): spinal cord
(medulla oblongata), vertebral artery, spinal root of the accessory nerve, anterior and posterior spinal arteries,
a tiny branch of the meningeal artery, and the spinal origin from the upper part of the spinal cord.
EXTERNAL SURFACE OF THE SKULL
The nasal bone forms the bony part of the anterior wall of the nose.
The maxilla has 4 processes and a body. The body has a cavity called the maxillary sinus. The four
processes are 1)Frontal, 2)Palatine, 3)Zygomatic, 4)Alveolar. The shape of the body is pyramidal or
tetrahedral. The anterior surface of the maxilla has the fossa canina (name comes from dogs where it is
very large). It also has the orbital surface, the infratemporal surface (having the tuber maxillae), and the
nasal fossa with the hiatus of the maxillary sinus.
The zygomatic bone has a temporal process which helps form the zygomatic arch (with the zygomatic
process of the temporal bone). It has three surfaces: Orbital, temporal, and lateral.
The zygomatic canal is a Y-shaped canal. Its inlet is the foramen zygomatico-orbitale. Its two outlets
are the foramina zygomaticofaciale and zygomaticotemporale. The canal divides into two parts inside the
zygomatic bone and transmits the zygomatic nerve (branch of the maxillary nerve) innervating a part of the
face above the zygomatic bone.
The vomer, which is the posteroinferior part of the septum nasi, forms two tiny wings called the alae
vomerum. They are attached to the inferior surface of the body of the sphenoid bone.
The palatine bone is an L-shaped bone, having a perpendicular plate and a horizontal plate. The
perpendicular plate divides into two processes (sphenoidal and orbital). The first is attached to the body of
the sphenoid bone, and the second forms a part of the inferior wall of the orbital cavity. Between them,
there is a notch called the sphenopalatine notch (incisura). This notch is the inferior border of the
sphenopalatine foramen (or fossa). The superior border is the inferior part of the body of the sphenoid bone.
This foramen connects the pterygopalatine fossa with the nasal cavity. The horizontal part of the palatine
bone forms the posterior part of the hard palate. The pyramidal process is between the pterygoid process
and the maxilla. The conchal crest is where the inferior nasal concha is attached to the maxilla and palatine
bone.
The lacrimal bone is an oval-shaped bone right behind the frontal process of the maxilla. It has a
posterior lacrimal crest and an anterior lacrimal crest on the maxilla. Between these two crests, there is a
fossa called the fossa sacci lacrimalis (fossa for the lacrimal sac). We have also the lacrimal canal that
leads to the inferior nasal meatus (tears drain to the nasal cavity through this canal). Inferior nasal concha is
a separate bone which is attached to the maxilla and the palatine bone.
The pterygoid process has two lamina: medial and lateral lamina of the pterygoid process. The medial
process forms a hook called the hamulus pterygoideus. The tendon of the tensor veli palatini muscle is
attached there. If you follow the medial lamina (root), you will find the scaphoid fossa that continues lateral
and backward to the sulcus tubae auditivae, which in turn continues to the canalis musculotubarius
(containing the auditory tube and tensor tympani muscle).
29
With the auditory tube, the pressure of the ear is equalized because the tympanic cavity is closed to its
one end by the tympanic membrane. So, the air communicates with the pharynx through this tube.
The lower part of the canalis musculotubarius goes into the tympanic cavity.
The foramen ovale and spinosum connect the middle cranial fossa with the outer surface of the skull.
At the root of the pterygoid process, there is a canal called the pterygoid canal. This leads to the
pterygopalatine fossa. The greater petrosal nerve comes out from the foramen lacerum, then goes into the
pterygoid canal, arising in the pterygopalatine fossa. Inside the fossa, there is the pterygopalatine ganglion.
So, the greater petrosal nerve takes the preganglionic fibers to the ganglion.
The pharyngeal tubercle is at the outer surface of the skull. The pharynx is behind the nasal cavity and
behind the oral cavity. It has posterior and lateral walls, but no anterior wall, because anteriorly, it
communicated with the nasal cavity, oral cavity, and larynx.
The carotid foramen is the inlet of the carotid canal.
The tegmental crest separates two fissura: petrotympanic and petrosquamosa.
Lateral to the jugular foramen, we have the jugular fossa for the internal jugular vein.
Between the carotid foramen and the jugular foramen, there is a tiny fossa called the fossa petrosa. The
canaliculi tympanici runs in this fossa, and then goes into the tympanic cavity. It transmits the tympanic
nerve (from the glossopharyngeal). When this nerve comes out from the tympanic cavity, it is called the
LESSER PETROSAL NERVE. The GREATER PETROSAL NERVE is a branch of the facial nerve. The sulcus nervi
petrosi majoris comes out from the facial canal. The sulcus nervi petrosi minoris comes out from the
tympanic cavity. There is another tiny opening on the margin of the pyramidal bone, below the porus
acusticus internus. This is the apertura externa aqueductus vestibuli (or cochleae). Two openings are
found in the fossula petrosa (1canaliculus tympanicus and 2apertura externa aqueductus cochleae).
On the wall of the carotid canal, there are tiny canaliculi called the canaliculi caroticotympanici.
The foramen stylomastoidea is the outlet of the facial canal. The incisura mastoidea is lateral to the
sulcus arteriae occipitalis (for the occipital artery, which is a branch of the external carotid artery).
The temporal fossa communicates below with the infratemporal fossa. The temporalis muscle,
belonging to the muscles of mastication, arises from the temporal fossa. On the superior border of the fossa,
there are the superior and inferior temporal lines. They begin from the frontal bone. The temporalis
muscle is inserted to the mandible at the coronoid process. Its function is to move the mandible upward to
close the mouth. Its posterior fibers move the mandible back to the mandibular fossa. This muscle is
covered by the temporal fascia which arises from the superior nuchal line and attaches to the zygomatic arch.
It has an inner and an outer layer which surround some connective tissue.
The border between the temporal and infratemporal fossae is the zygomatic arch and the infratemporal
crest. This fossa communicates with the pterygopalatine fossa through the pterygomaxillary fissure. In the
infratemporal fossa, the maxillary artery goes to the pterygopalatine fossa.
30
MANDIBLE
The mandible has a body (corpus mandibulae) and a ramus (ramus mandibulae). The angle between
them is called the angulus mandibulae. The ramus has two processes: the anterior is called the coronoid
process, and the posterior is called the condylar process. The condylar process has two parts: the caput
mandibulae and the column mandibulae. The area between the two processes is called the mandibular notch
(incisura mandibulae). The head is part of the temporomandibular joint. Just below the head, we have the
fovea pterygoidea (for the lateral pterygoid muscle). The medial pterygoid muscle is inserted to the inner
pterygoid tuberosity. On the outer surface of the angle, there is another tuberosity called the masseteric
tuberosity (for the so named muscle).
The mylohyoid line (for the mylohyoid muscle) and the mylohyoid sulcus (for the mylohyoid nerve) can
be found on the inner surface of the mandible.
The MENTAL SPINE is a spine for the "genio-" muscles ("geneion" is Greek for "chin"). Just beneath the
mental spine, there are two tiny fossas called fossae digastricae (for the digastric muscles). Lateral and
superior to this fossa, there are two foveae called submandibular foveae (for the submandibular glands).
Above the mylohoid line, there are two other foveae called the sublingual foveae (for the sublingual glands).
There are three main pairs of salivary glands: parotid, sublingual, and submandibular.
The main structure of the mandible is the MANDIBULAR CANAL. The inlet of this canal is the foramen
mandibulae, which is located on the inner surface of the ramus. The outlet is called the foramen mentale,
which is located on the outer surface of the body of the mandible. The inferior alveolar nerve and artery run
inside the canal. Out of the canal, there is a groove (sulcus) which comes from behind the mandibular
foramen and is called mylohyoid sulcus. This sulcus is for the mylohoid nerve.
The foramen mandibulae is covered by a tiny lingula (lingula mandibulae) which forms a protrusion. In
order to anesthetize the lower teeth, we have to inject toward this lingula.
The mandible has the alveolar process having the dental alveola inside, and these alveola are separated by
the interalveolar septa (septa interalveolaria). For the posterior teeth that have two roots, a septum
separates them, called the septum intermusculare (it also appears on the maxilla).
We also have the mental prominence. Behind the molar teeth, we have a tiny retromolar triangle. On
the outer surface, there is a line called the linea obliqua (origin for the muscles of the facial expression).
ORBITAL CAVITY
Inlet: aditus orbitae,
Outlet: optic canal.
It is a pyramid-shaped cavity. The axis of this cavity is a little oblique, from posteromedial to
anterolateral. There are four walls:
Superior: Orbital plate of the frontal bone (anterior) and lesser wing of the sphenoid bone (posterior).
Lateral: Orbital surface of the greater wing of the sphenoid bone and orbital surface of the zygomatic
bone.
Between the superior and lateral walls, the superior orbital fissure (CN III, IV, V3, VI, and
superior ophthalmic vein).
Between the lateral and inferior walls, the inferior orbital fissure leads either to the pterygopalatine fossa or to the infratemporal fossa. Through this, run the infraorbital nerve + artery,
the zygomatic nerve, and the inferior ophthalmic vein.
Inferior: Orbital surface of the maxilla (anterior) and orbital process of the palatine bone (posterior).
Medial: Frontal process of the maxilla, lacrimal bone, lamina orbitalis of the ethmoidal bone (or lamina
papyracea), and the body of the sphenoid bone.
The ethmoidal air cells are divided into three groups: anterior, middle, and posterior. The anterior and
middle cells open into the meatus nasi media, and the posterior cells open into the meatus nasi superioris.
31
The largest air cell is called the BULLA ETHMOIDALIS and makes an elevation on the lateral wall. Below this
elevation, there is a process called the processus uncinatus. The bulla ethmoidalis is usually found in the
middle group of air cells. Between the bulla and the process, there is a crescent-shaped hiatus called the
semilunar hiatus. From the posterior end of the semilunar hiatus, if we go downward and laterally, it will
lead us to the maxillary sinus. From the middle part of the hiatus, if we go a little upward and laterally, it
will lead to the anterior and middle ethmoid air cells. From the anterior part of the hiatus, if we go in front
and upward, it will lead to the frontal sinus (through the ethmoid sinus - bone). So, you can say that the
semilunar hiatus is the common opening for the maxillary sinus, frontal sinus, and anterior & middle groups
of air cells.
The borders of the semilunar hiatus are:
Superior: bulla ethmoidalis,
Inferior and anterior: processus uncinatus.
Connections of the Orbital Cavity:
The infraorbital canal and foramen (outlet) opens into the fossa canina. This canal starts with a
sulcus called the sulcus infraorbitalis, and then, it continues as a canal that opens into the anterior surface of
the face (fossa canina). It transmits the infraorbital artery and nerve.
The supraorbital foramen or notch (sometimes) transmits the supraorbital artery and nerve.
Medial to the supraorbital foramen, the frontal notch is for the frontal branch of the frontal nerve or
the medial branch of the supraorbital nerve. Both terms are used. If you use the second term, you should
say that the lateral branch passes through the supraorbital foramen. The frontal nerve is a branch of the
ophthalmic (CN V1).
There are two tiny foramina between the frontal bone and the ethmoid bone: posterior and anterior
ethmoidal foramen. The anterior one leads into the fossa cranii anterioris and the posterior goes into the
ethmoidal air cells. The structures that pass through are anterior ethmoidal artery and nerve and the
posterior ethmoidal artery and nerve.
The nasolacrimal canal is a descends into the inferior nasal meatus. It starts from the fossa sacci
lacrimalis which is bordered by the anterior lacrimal crest and the posterior lacrimal crest on the lacrimal
bone. It ends into the inferior nasal meatus, allowing tears to drain into the nasal cavity.
On the zygomatic bone, there are three tiny foramina: 1zygomaticoorbital (beginning of the zygomatic
canal that is inside the zygomatic bone), 2zygomaticofacial, and 3zygomaticotemporal. The last two are
the outlets of the zygomatic canal. So, the zygomatic canal is a Y-shaped canal.
The optic canal transmits the optic nerve and the ophthalmic artery. It connects the orbital cavity
with the middle cranial fossa.
The superior margin of the orbital cavity is called margo supraorbitalis, and the inferior one is called
margo infraorbitalis. Above the supraorbital margin, we have the supraciliary arches, and between them,
the glabella.
32
NASAL CAVITY
Inlet: apertura piriformis (pear-shaped aperture): bordered by the nasal bone, the frontal process of the
maxilla, and by the body of the maxilla.
Outlet: choanae.
Borders of the choanae: LATERAL: medial plate of pterygoid process. INFERIOR: horizontal plate
of the palatine bone. MEDIAL: vomer. SUPERIOR: body of the sphenoid bone (having the ala
vomeris on it).
In the inferior part of the cavity, there is a spine which is called spina nasalis anterioris.
The nasal cavity has four walls:
Anterior: nasal bone.
Superior: nasal part of the 1frontal bone (ant.), 2cribiform plate (mid.), and 3body of the sphenoid
bone (post.). The anterior surface of the body has the hiatus sinus sphenodalis opening into the
nasal cavity. So, the superior wall has three parts.
Medial: The septum nasi. Between the perpendicular plate of the ethmoid and the vomer, there is a
V-shaped space in front, filled with cartilage and forming the cartilaginous part of the septum
nasi. There are cartilaginous and bony parts of the septum nasi.
Inferior: The hard palate, which is composed of the palatine process of the maxilla (front) and the
horizontal plate of the palatine bone (behind).
In the midline of the nasal cavity, there is a crest which is called the crista nasalis (where the
septum nasi is ossified). The crista nasalis forms a spine in front and behind which is called
spina nasalis anterior and posterior.
Lateral: Anteriorly, is the frontal process of the maxilla. Behind and a little below, lies the lacrimal
bone (a part of which closes the nasolacrimal canal). Above and behind the lacrimal bone, we
have the ethmoidal bone. Beneath the middle nasal concha are the processus uncinatus and the
bulla ethmoidalis. Between them, we have the semilunar hiatus. Below the ethmoid bone, lies
the maxilla, which has the inferior nasal concha (a separate bone which is ossified to the maxilla,
palatine bone, processus uncinatus, lacrimal bone).
Behind the maxilla, we have the perpendicular plate of the palatine bone. Behind this is the medial plate
of the pterygoid process.
[The crista conchalis is where the inferior nasal concha is ossified]
CONNECTIONS OF THE NASAL CAVITY:
Paranasal sinuses (4) are cavities surrounding the nasal cavity, filled by air, and layered by mucous
membrane. They open into the nasal cavity.
a) Frontal sinus: opens into the middle nasal meatus through the anterior part of the semilunar hiatus.
b) Maxillary sinus: opens into the middle nasal meatus through the posterior part of the semilunar
hiatus.
c) Ethmoid sinus: the anterior and middle groups of air cells open into the middle nasal meatus, and
the posterior group opens into the superior nasal meatus.
d) Sphenoid sinus: opens into the sphenoethmoidal recess (an angle between the sphenoid bone and
the lamina cribrosa). The recess doesn't belong to any meatus, but is superior to the superior
concha.
Sphenopalatine foramen (or pterygopalatine) that connects the nasal cavity with the pterygopalatine
fossa. So, the inferior border of the sphenopalatine foramen is the sphenopalatine notch which is
between the orbital process and the sphenoid process of the palatine bone.
Canalis incisivus that connects the nasal cavity with the oral cavity. It transmits the nasopalatine
nerve and artery.
Cribiform plate. It transmits the fila olfactoria (nervi olfactorii).
Nasolacrimal canal. It connects the orbital cavity with the inferior nasal meatus.
33
ORAL CAVITY
Superior wall: hard palate,
Inferior wall: mylohyoid muscles (arising from the mylohyoid line of the mandible),
Lateral wall: If the mouth is closed, the mandible (below) and alveolar process of the maxilla
(above). If the mouth is open, the buccinator muscle.
CONNECTIONS OF THE ORAL CAVITY:
Canalis incisivis: connects the oral cavity with the nasal cavity.
Canalis palatinus major and minor: connects the oral cavity with the pterygopalatine fossa.
transmits the artery and nerve with the same name.
Mandibular canal: Inlet - mandibular foramen. Outlet - foramen mentale.
It
PTERYGOPALATINE FOSSA
Medial wall: pterygoid process and perpendicular plate of the palatine bone,
Superior wall: body of the sphenoid bone,
Anterior wall: maxilla,
Inferior: fusion of the anterior and posterior walls. If you go through the pterygomaxillary fissure, you
will arrive in the pterygopalatine fossa.
Lateral: is open, into the infratemporal fossa.
CONNECTIONS TO THE PTERYGOPALATINE FOSSA:
Pterygomaxillary fissure: it transmits the maxillary artery and the nerves supplying the posterosuperior
teeth (superior alveolar nerve coming from the infraorbital nerve). There are tiny foramina on the
maxilla where the nerves enter the maxilla and reach the posterior teeth, called the tuber maxillae.
Inferior orbital fissure: connection with the orbital cavity.
Sphenopalatine foramen (or pterygopalatine): transmits the sphenopalatine artery and posterior nasal
nerve to the nasal cavity.
Foramen rotundum: connection with the middle cranial fossa.
Greater and lesser palatine foramina: connect with the oral cavity via the greater and lesser palatine
canals. They transmit the greater and lesser palatine nerves and the descending palatine artery.
Pterygoid canal: connection with the outer surface of the skull. At the root of the medial plate of the
pterygoid process, it goes straight forward into the pterygopalatine fossa. It transmits the great
petrosal nerve to the pterygopalatine fossa. Inside the fossa, there is a ganglion (group of nerve cell
bodies surrounded by a capsule).
Pterygovaginal canal (not so important): transmits a pharyngeal branch of the maxillary nerve and
artery.
34
TEMPOROMANDIBULAR JOINT
Head: caput mandibulae,
Cavity: mandibular fossa of the temporal bone and the articular tubercle.
The articular surfaces are covered by fibrous cartilage. Inside the joint, there is an articular disc, which
has an S shape, between the head and the cavity. It is fused with the capsule, and it divides the cavity into
two parts: 1Discotemporal part (superior) between the disc and temporal bone, and 2Discomandibular part
(inferior) between the disc and the mandible.
ARTICULAR CAPSULE:
Loose, and is attached in front to the root of the zygomatic process and anterior to the fissura petrosquamosa. It inserts to the neck of the mandible (right below the head). This is important because on
the neck, we have the attachment of the lateral pterygoid muscle. It must be outside the capsule.
LIGAMENTS (not very important according to the movements):
Stylomandibular: styloid process to the angle of the mandible.
Sphenomandibular: sphenoid bone to the lingula mandibulae.
Temporomandibular: root of the zygomatic arch to the column mandibulae (neck). This ligament is
fused with the capsule and is also called the lateral ligament.
MOVEMENTS:
1
Opening and closing of the mouth. During this movement, the caput mandibulae rotates in the
inferior part of the joint (discomandibular part). This rotation is around an axis which connects the foramina mandibuli. This is important because there are arteries and nerves going to the mandibular canal.
So, if you consider that the axis is the fixed point of a movement, you can understand that the structures will
not break.
At the same time (with the rotation), the head of the mandible comes out to the articular tubercle together
with the articular disc. The anterior movement is done by the lateral pterygoid. The rotation is made by
the suprahyoid group of muscles (mylohyoid, digastric, and geniohyoid muscles).
Closing of the mouth is made by the temporal, pterygoid, and masseter muscles (last from the zygomatic
arch to the masseteric tuberosity). The masseter muscle is completely parallel to the medial pterygoid.
The posterior fibers of the temporal muscle move the mandible backward to the mandibular fossa.
2
Protraction and retraction (we have to open the mouth a little). This movement is made by the lateral
pterygoid muscle.
3
Lateral movement. In this case, we have different movements in the right and the left joint. If the
mandible moves to the left, the head of the mandible comes out to the articular tubercle on the right
(contralateral) side. On the ipsilateral side, there is a passive rotation. The axis if this movement is a
longitudinal axis through the column mandibulae.
4
Circumduction is the combination of these three main movements (chewing movement). The
longitudinal axis ("jumping axis") of this movement is postponed laterally between the two end faces.
FINAL REMARKS:
The parallel part of the facial nerve is out of the tympanic cavity, and then it descends and comes out
from the stylomastoid foramen. When it descends, it gives a branch back to the tympanic cavity called the
chorda tympani. So, the facial nerve comes in the meatus acusticus interni through the porus acusticus
interni, and in the fundus acusticus interni, the facial canal starts. The facial canal is first vertical to the axis
of the pyramidal bone, then parallel, and finally it turns downward and comes out through the stylomastoid
foramen. In the angle between the vertical part and the parallel part, it gives a branch called greater petrosal
nerve. Then, it gives the chorda tympani.
35
The apertura externi aqueductus vestibulae is behind the porus acusticus interni and below the arcuate
eminence.
The apertura externi canaliculi cochlei is in the fossula petrosa.
The subarcuate fossa is below the arcuate eminence and above the porus acusticus interni.
The four surfaces of the maxilla are: 1anterior, 2orbital, 3infratemporal, 4nasal.
The sulcus tubae auditivae (groove for the auditory tube): in order to find the sulcus, first you should
find the scaphoid fossa and follow it backward and laterally. Then, the sulcus continues in the bony canal
called canalis musculotubarius and terminates inside the tympanic cavity.
The choana continues to the pharynx, which has three parts. The first part opens into the nasal cavity
(through the choana). The second part opens into the oral cavity. The third part communicated with the
larynx.
The fossula petrosa is between the carotid foramen and jugular foramen. The fossula petrosa has two
openings. The first is called canaliculus tympanici, and the second is called apertura externi canaliculi
cochlei.
The sphenopalatine artery (together with the posterior nasal nerves) goes to the nasal cavity through the
sphenopalatine foramen and the pterygomaxillary fissure.
The hiatus pterygoidei is a space between the lateral and medial pterygoid muscles (not a bony space).
The inferior nasal concha is ossified
The canalis incisivum + greater and lesser palatine foramen.
36
FACE
FRONTAL REGION
Margins: supraorbital arch, midline, sutura coronalis, temporal line.
SKIN INNERVATION:
Ophthalmic nerve (CN V1).
The frontal nerve (from the ophthalmic) gives branches that pass through the supraorbital notch
(supraorbital nerve - lateral branch) and through the frontal notch (ramus frontalis nervi frontalis - medial
branch). The third branch is the supratrochlear nerve. Together with these nerves, there are arteries with
the same name which are branches of the ophthalmic artery that comes from the internal carotid artery.
ALL THE ARTERIES OF THE FACE COME FROM THE EXTERNAL CAROTID ARTERY
EXCEPT THE FRONTAL BRANCHES.
The frontal branch of the superficial temporal artery (from the external carotid) is located at the lateral
part of the region (coming from the temporal region).
SUPERFICIAL STRUCTURES:
Together with the nerves and arteries, we have the frontal muscle (or the frontal head of the
occipitofrontalis muscle - a.k.a. the epicranius muscle). This muscle belongs to the muscles of facial
expression innervated by the facial nerve. The frontal muscle is inserted to the galea aponeurotica
(connective tissue cap of the head) and to the skin of the eyebrow.
Medially, we have the corrugator supercilii muscle and the depressor supercilii muscle, both belonging
to the muscles of facial expression. Both are therefore innervated by the facial nerve.
TEMPORAL REGION
Borders: superior temporal line, zygomatic arch.
SKIN INNERVATION:
Auriculotemporal nerve (from the mandibular nerve - CN V3), which innervates the external ear, external
acoustic meatus, temporal region, and a small part in front of the ear.
Removing the skin, you can find a very thick fascia that covers the temporalis muscle called the temporal
fascia. The fascia arises from the superior temporal line, covers the temporal muscle and inserts to the
zygomatic arch. It has two layers: an outer layer (inserted to the outer surface of the arch) and an inner layer
(inserted to the inner surface of the arch). Between these two layers there is fat and connective tissue.
Medial to the zygomatic arch, the temporalis muscle runs toward the mandible and inserted to the coronoid
process. In front of the external ear, there are three structures ascending through the region:
Auriculotemporal nerve (from the mandibular nerve), Superficial temporal artery, and Superficial
temporal vein. The superficial temporal artery is the end branch of the external carotid artery (the other is the
maxillary artery). This division of the external carotid artery occurs behind the ramus mandibulae inside the
parotid gland in the retromandibular fossa. The maxillary artery goes to the infratemporal fossa and finally
to the pterygopalatine fossa. The superficial temporal artery is superficial in this region, and we can even
palpate it (sometimes).
37
The temporalis muscle belongs to the muscles of mastication. Its function is to elevate the mandible,
and the posterior fibers move the mandible back to the mandibular fossa (retraction). The muscle is
innervated by the mandibular nerve (V3). The mandibular nerve innervates all the muscles of mastication.
To see the nerves innervating the temporalis muscle (and the arteries giving blood supply to the muscle),
you should cut the fascia and the muscle. You will see the deep temporal artery (maxillary artery
external carotid artery) and the deep temporal nerve (from the mandibular nerve).
INFRAORBITAL AND BUCCAL REGION
Posterior: anterior margin of the masseter,
Medial: nasolabial line (from the nose to the lips),
Inferior: base of the mandible,
Superior: infraorbital margin.
SKIN INNERVATION:
Infraorbital branch of the maxillary nerve (through the infraorbital canal/foramen, together with the
infraorbital artery -from the maxillary artery).
The infraorbital artery and nerve are not superficial. You have to cut the levator labii superioris muscle
to see them. The levator labii superioris muscle has three heads: 1zygomaticus minor (most lateral), 2levator
labii superioris (middle - and the same name as the whole muscle!), 3levator labii superioris alaeque nasi
(medial).
The middle head was first named infraorbital head. But, the new nomenclature is levator labii superior.
The most superficial structures in this region are the muscles of the facial expression. Mainly, the
levator labii superior, the inferior fibers of the orbicularis oculi muscle (surrounds the orbital cavity) and the
zygomaticus major. Below the mouth, there is another muscle called the depressor anguli oris muscle (if we
cry, it moves the angle of the mouth downward).
Beneath these muscles (or going to these muscles), run the branches of the facial nerve. The branches
come out from the parotid gland. These are the marginal mandibular branch, buccal branch, zygomatic
branches, temporal branch, and the cervical branch (innervates the platysma, which is the only muscle of the
facial expression that is located on the neck and is innervated by the facial nerve).
Beneath the muscles, run the facial artery and vein. These two structures are located just in front of the
masseter muscle at the anterior border, on the body of the mandible. You can palpate the pulse of the artery.
To distinguish between them, you should know that the artery is in front and is wavy, while the vein is behind
and straight. The facial vein anastomoses with the superior ophthalmic vein and this anastomosis is called
the angular vein. The facial artery comes from the external carotid artery and gives the superior and inferior
labial branches and the submental artery. Finally, it gives the angular artery. Sometimes, there is a nasal
branch also (for the nose). The labial branches are dissectable. The facial vein is drained to the internal
jugular vein together with the retromandibular vein (from the superficial temporal and maxillary veins).
First, the facial and retromandibular veins are joined together, and then they drain in the internal jugular vein
(sometimes they drain into the external jugular vein: variation).
Another important structure here is the ductus parotidus (parotid duct) coming from the parotidomassseteric region on the surface of the masseter muscle, 1 cm below the zygomatic arch (parallel to it). It
pierces through the buccinator muscle and open into the oral cavity, the vestibulum oris (between the lips and
the teeth). So, it opens on the mucous membrane of the cheek, opposite to the upper first and second molar
teeth.
On the buccinator muscle, we can find the buccal nerve, the only sensory branch of the motor group of
the mandibular nerve. It innervates the mucous membrane of the cheek and the two angles of the mouth.
The mandibular nerve has a motor group (innervating the muscles of mastication) and has three sensory
branches (auriculotemporal, buccal, lingual, and inferior alveolar).
38
The motor group has just one sensory branch called the buccal nerve.
The buccal artery comes from the maxillary artery.
The orbicularis oculi muscle has three parts:
Orbital part (surrounds the orbital cavity),
Palpebral part (inside the palpebra),
Lacrimal part (arises from the lacrimal bone and from the wall of the lacrimal sac). It moves the
lateral wall of the lacrimal sac making a vacuum inside, forcing the draining of the tears into the
nasal cavity.
MENTAL REGION
It is a tiny region in front of the infraorbital and buccal region until the midline and of course at the level
of the mandible below (including the lower lip).
In this region, only the mental nerve and artery emerging from the mental foramen are important. They
are branches of the inferior alveolar nerve and artery, inside the mandibular canal. The endbranches come
out from the mental foramen as the mental nerve and artery supplying the mental region and innervating its
skin.
Muscles of facial expression are in this region: Depressor anguli oris, Depressor labii inferioris, and the
mentalis muscle (they depress the lips).
We have also the 1risorius muscle, which is a very superficial muscle and comes from the infraorbital and
buccal region. It is also called the "smiling" muscle. 2Orbicularis oris is attached to the jugum, a protrusion
that the teeth form on the mandible and the maxilla.
PAROTIDOMASSETERIC REGION
Anterior: anterior border of the masseter muscle,
Posterior: external ear and ramus of the mandible,
Superior: zygomatic arch.
SKIN INNERVATION:
Auriculotemporal nerve (from the mandibular).
Beneath the skin, the parotidomasseteric fascia covers the parotid gland and the masseter muscle. This
fascia continues on to the neck forming the superficial cervical fascia (very thin).
There are three fascias in the neck: Superficial, Middle, and Deep cervical fascia. The platysma is
superficial to the superficial cervical fascia.
Superficially, the branches of the facial nerve emerge from the parotid gland (more details earlier).
Together with the nerve, a tiny artery comes from the parotid gland, running parallel to the parotid duct,
called the transverse facial artery (sometimes is so small that you cannot find it). It comes from the
superficial temporal artery piercing through the parotid gland from posterior to anterior.
The parotid gland and its duct (on the masseteric muscle) opening into the oral cavity can be found in this
region (more details previously).
We can also find in the anterior part of the region the facial vein and artery and the origin and insertion of
the masseter muscle (zygomatic arch masseteric tuberosity: functions to elevate the mandible).
The parotid gland is located in the nidus parotidus (nest of the gland).
Borders of the nidus:
Superior: zygomatic arch,
Inferior and Posterior: sternocleidomastoid muscle and posterior belly of the digastric muscle
(both coming from the styloid process).
39
Anterior: masseteric muscle and medial pterygoid muscle and the ramus of the mandible.
Deep (or medial) wall: styloid muscles (arising from the styloid process): Stylopharyngeus, to the
pharynx; Stylohyoid, to the hyoid bone (together with the posterior belly
of the digastric muscle); Styloglossus, to the tongue.
The facial nerve innervates: 1) muscles of facial expression, 2) stylohyoid muscle, 3)posterior belly
of the digastric muscle, 4)stapedius muscle (in the middle ear).
The parotid is pierced through by several structures: Posterior to Anterior
Facial nerve (giving temporofacial and cervicofacial roots in the gland).
Transverse facial artery.
Superficial temporal vein. When it is inside the parotid gland, it receives the pterygoid plexus (a
venous plexus) forming the retromandibular vein. So, the vein that finally leaves the parotid gland is
called the retromandibular vein.
External carotid artery passes also through the parotid gland and fives the superficial temporal artery.
Auriculotemporal nerve, passing through the gland from deep to the surface (medial lateral).
The parotid gland is innervated by the glossopharyngeal nerve; all the other glands by the facial
nerve.
The lesser petrosal nerve is a branch of the glossopharyngeal nerve and is the same nerve as the tympanic.
It is called tympanic when it is inside the tympanic cavity. Outside the tympanic cavity, it is called the
lesser petrosal nerve (it exits the skull through the foramen ovale). All the other glands are innervated by
the facial nerve.
INFRATEMPORAL FOSSA
You should remove the mandible to see this region. If you remove it, you will see the infratemporal
fossa (or the retromandibular fossa).
The pterygoid muscles are covered by the mandible.
The pterygoid hiatus is between the two muscles (medial and lateral pterygoid muscles).
To see all these structures, cut the masseteric muscle and the articular capsule of the temporomandibular
joint, remove the head of the mandible, dissect the alveolar nerve and artery from inside the mandible, and
then the side of the mandible can be removed.
THE STRUCTURES PASSING THROUGH THE PTERYGOID HIATUS ARE:
Maxillary artery: through this hiatus, it goes into the pterygopalatine fossa.
Lingual nerve and inferior alveolar nerve come out through the hiatus pterygoidei.
40
Medial pterygoid
Origin-Deep head: medial surface of the lateral pterygoid plate and pyramidal process of the palatine
bone. Superficial head; pyramidal process of palatine and tuber of the maxilla.
Insertion- medial surface of the mandible near the angle .
Lateral pterygoid
Origin-Upper head: infratemporal surface of sphenoid bone. Lower head: lateral surface of the
lateral pterygoid plate.
Insertion- pterygoid fovea below condyloid process of mandible and the intra-articular cartilage of
the temporomandibular joint.
THE MAXILLARY ARTERY GIVES BRANCHES HERE:
Auricularis profundus (external acoustic meatus) and tympanic anterior (tympanic cavity).
Middle meningeal artery (surrounded by the two roots of the auriculotemporal nerve).
Anterior and posterior deep temporal arteries.
Buccal artery.
Inferior alveolar artery (through the mandibular canal, it innervates the lower teeth).
After these branches, it reaches the pterygopalatine fossa, and there it divides into end branches:
Descending palatine artery (oral cavity).
Sphenopalatine artery (nasal cavity).
Infraorbital artery (orbital cavity).
There are also tiny arteries supplying the muscles having the same name.
In the deepest part of the pterygoid hiatus, lies the chorda typmani, joining the lingual nerve. The
chorda tympani transmits taste sensory fibers and preganglionic secretomotor fibers.
The lingual nerve contains three types of fibers: a) general sensory fibers, b) taste fibers, and c) secretory
fibers.
The anterior 2/3 of the tongue is innervated by the lingual nerve and the posterior 1/3 by the
glossopharyngeal nerve.
The inferior alveolar nerve gives sensory innervation for the lower teeth through the mandibular canal,
and it has one motor fiber which is the mylohyoid nerve (located in the mylohyoid sulcus). The mylohyoid
nerve gives innervation for the mylohyoid muscle and the anterior belly of the digastric muscle.
The inferior alveolar artery runs together with the inferior alveolar nerve, and their end branches are
called the mental artery and nerve.
SUMMARY OF THE SENSORY INNERVATION OF THE FACE
Frontal region, upper palpebral region, and the root of the nose: Supraorbital, frontal, and
supratrochlear nerves (from the ophthalmic nerve).
Lower palpebral region, nose, upper lips, and cheek: Infraorbital nerve (endbranch of the maxillary).
Lower lips and mental region: Mental nerve (end branch of the inferior alveolar nerve).
Front of the ear, temporal region, external acoustic meatus, external ear, temporomandibular
joint: Auriculotemporal nerve.
Skin covering the zygomatic bone: Zygomatic nerve.
These branches come out through three foramina that are in the same line: 1Supraorbital, 2Infraorbital,
and 3Mental foramen. This has an important clinical significance because sometimes, the patients have
neuralgia (a terrible headache). If you press the nerve at the point where it emerges through the foramen,
the patient will feel pain. In this way, you can determine the presence of neuralgia.
41
ORAL CAVITY
Borders of the vestibule:
Anterior: lips,
Lateral: cheek (+ buccinator muscle),
Posterior: teeth and gums.
Borders of the oral cavity proper:
Superior: hard and soft palates,
Inferior: tongue and floor of the oral cavity,
Floor: mylohoid muscle (covered by the mucous membrane),
Lateral: mandible (above the mylohyoid line) + teeth.
The lips are connected to the gums by the frenulum labii inferioris and superioris. The tongue is
connected to the floor of the oral cavity by the frenulum linguae. Lateral to the frenulum linguae, we have
the caruncula sublingualis which is the common opening of the submandibular and sublingual glands.
From the apex of the tongue toward the lateral direction, there is a fold which is called plica fimbriata
(and a vein inside called sublingual vein).
The submandibular duct and the lingual nerve, after the sulcus lateralis linguae, cross each other. So,
after the crossing, the submandibular duct is superior and the lingual nerve is inferior.
The soft palate consists of two muscles - the levator and tensor veli palatini. We have also the tiny
uvulae muscle.
From the uvulae to the root of the tongue and the pharynx, there are two important arches:
a)
Palatoglossal arch (anterior) and b) Palatopharyngeal arch (posterior). These two arches have muscles
inside with the same name. Between the two arches, the tonsilar fossa is where the palatine tonsils are
located.
MUSCLE
ORIGIN
INSERTION
FUNCTION
INNERVATION
Tensor Veli
Palatini (L-shaped
muscle)
Scaphoid fossa +
cartilage of auditory
tube + hamulul
ptery-goidei
Soft palate
Extend the soft
palate + open the
pharyngeal opening
of the auditory
tube.
Trigeminal nerve.
(mandibular)
Levator Veli
Palatini (medial &
behind the tensor
veli palatini)
(V-shaped muscle)
Apex of pyramidal
bone + sphenoidal
bone
Soft palate
Elevates the soft
palate and closes
the choana when
you swallow, so the
food doesn't go to
the nasal cavity. It
also helps to open
the auditory tube.
Palatoglossal
muscle
Soft palate
Root of tongue
Glossopharyngeal
nerve
Palatopharyngeal
muscle
Soft palate
Wall of pharynx
Vagus nerve
(or facial)
Vagus nerve.
(or facial)
42
The communication between the oral cavity and the oropharynx is the oropharyngeal isthmus faucium.
Borders of the isthmus faucium:
Lateral: the above two mentioned arches,
Superior: uvula,
Inferior: root of the tongue.
Above the palatine tonsils, we have the supratonsilar fossa (where the fish bones may stick). Between
the root of the tongue and the body of the tongue, we have the sulcus terminalis (V-shaped line). In front of
the line, there are circumvallate papillae. Behind is the follicular surface of the tongue (or lingual tonsils).
The pharyngeal and tubal tonsils are in the nasopharynx. The four tonsils (tubal, pharyngeal, palatine, and
lingual) form the Waldeyer's ring (or lymphatic ring).
PHARYNX: Is the tube where the respiratory tract and GI tract divide (where the ways of the food and
air divide).
TEETH
The teeth have different surfaces: the inner one is called palatinal (only for the upper teeth) or lingual
(for both upper and lower).
The opposite surface, facing toward the lips or toward the cheek, is called the labial or buccal surface
(depending on the place of the teeth). If it is a front tooth, it has a labial surface. A molar or premolar has
a buccal surface.
The third surface is the masticatory surface, but we have this surface only for the molar and premolar
teeth. On the masticatory surface, there are tubercles (the surface is not smooth).
There are also contact surfaces for each tooth; medial and distal contact surfaces. The medial surface
is closer to the tooth in front, and the distal surface is closer to the tooth behind.
You should recognize the tooth according to the shape of the crown and the number of the roots. Each
tooth is divide into three parts: crown, neck, and root. The crown of the incisors have two surfaces: lingual
and labial. The upper first incisor is a little larger than the second (this happens only for the upper incisors).
The lower are the same. The incisors have one root.
The crown of the canines is cone-shaped, having an apex. They have only two surfaces: labial and
lingual. The lingual surface is concave, and the labial surface is convex. The root is single and longer than
the one of the incisors.
The premolars have masticatory surfaces and on these surfaces, they have tubercles (two). One of the
two tubercles is palatinal, and the other is buccal. They are separated by a sulcus. The premolars have
also one root, except the upper first premolar which has the double apex, or sometimes inside there are two
crowns (inside the root, the canal is doubled). But the root itself is just separated by a sulcus (not real two
roots).
All incisors, canines, and premolars have one root.
The upper molars have three roots, and the lower molars have two roots. The position of the root is two
buccal (masticatory) and one lingual (for the upper teeth) or one medial and one distal (for the lower molars).
The crown of the upper molars have three or four tubercles, and the crown of the lower molars have four or
five tubercles. If they have five tubercles, the fifth one is distal.
So, if the teeth have one root, it can be an incisor, canine, or premolar. If it is premolar, it must have
masticatory surface (with two tubercles). If it is an incisor, it must have the wedge-shaped crown. If it is a
canine, it must have a long root and an apex on the crown. If it has three roots, it must be an upper molar.
If it has two roots, it must be a lower molar.
You don't have to distinguish which number of the molar it is, just if it is upper or lower.
For the other types (except the molars), you don't have to distinguish if it is upper or lower. It is
impossible because they look exactly the same.
43
The above described teeth (until now) were the permanent teeth. The decidual teeth grow out in the half
year until the third year. The number of the decidual teeth is 20 (not 32 as the permanent): 2 incisors, 1
canine, 2 molars (decidual molar).
INNERVATION AND BLOOD SUPPLY:
The superior teeth are innervated by superior alveolar nerves and arteries forming three groups:
anterior, middle, and posterior. All three groups of the nerves come from the infraorbital nerve, a branch of
the maxillary nerve (according to some sources, only the anterior and middle superior alveolar nerves
come from the infraorbital nerve with the posterior superior alveolar nerve coming directly from the
maxillary nerve). The posterior superior alveolar artery comes from the maxillary artery. The anterior
and middle superior alveolar arteries come from the infraorbital artery.
The inferior teeth are innervated by the inferior alveolar nerve and artery. The nerve comes from the
mandibular branch of the trigeminal nerve, and the artery comes from the maxillary artery.
For the lower teeth, to remove as many as eight teeth (one side), inject the inferior alveolar nerve at the
level of the mandibular foramen (lingula mandibulae).
For the upper teeth, two or three injections (for one tooth) are necessary because the gum in front and
behind is innervated by different nerves. The labial gum is innervated by the infraorbital nerve. The
buccal (masticatory) gum is innervated by the buccal nerve. The upper lingual gum is innervated by the
greater and lesser palatine nerves (also the hard palate). The whole hard palate and the soft palate are
innervated by the greater and lesser palatine nerves (from the maxillary nerve) except the lingual gum of the
upper incisors (nasopalatine nerve).
NASAL CAVITY
The nasal cavity is divided into two parts: Vestibulum nasi (nasal vestibule), Cavum nasi proprium
(proper nasal cavity). The borderline between them is the limen nasi. The cavum nasi proprium is also
divided into two parts: the meatus nasi commini (common nasal meatus-- the medial part along side of the
nasal septum) and the lateral part that is composed of the three nasal meati: superior, middle, and inferior.
The mucous membrane of the nasal cavity is divided into two parts: a) olfactory region, and b) respiratory
region. The olfactory mucous membrane covers the superior nasal concha and the septum which is opposite
to the superior nasal concha (the superior part of the septum and the top of the nasal cavity). The epithelium
of the olfactory region is of a special type which gives the origin of the fila olfactoria. It is a primary
neuroepithelium. The fila olfactoria are running through the lamina cribrosa and form the olfactory nerve.
All the other parts of the nasal cavity is called the respiratory region and is covered by pseudo-stratified
columnar kinociliated epithelium having mucous glands inside.
PARANASAL SINUSES:
The superior nasal meatus has the opening of the posterior ethmoidal air cells. The middle nasal
meatus has the opening of the frontal sinus, maxillary sinus, and between them the anterior and middle
ethmoidal air cells. All these three open through the semilunar hiatus which is bordered superiorly by the
bulba ethmoidalis and inferiorly by the processus uncinatus. From this semilunar hiatus, we have an
infundibulum anterior that leads to the frontal sinus. From the posterior part, you can go into the maxillary
sinus or the "highmoon cavity". From the middle part of the hiatus, you can go to the ethmoidal air cells.
The inferior nasal meatus has the opening of the nasolacrimal duct which is inside the nasolacrimal canal.
44
The sphenoethmoidal recess doesn't belong to any meatus because it is above the superior concha, so it is
on the roof of the nasal cavity.
The nasal cavity communicates with the nasopharynx through the choana.
The anterior opening is the apertura piriformis (pear-shape) on the bony skull, and it is called nostril
(nares) inlet of the nasal cavity.
The nasal septum is composed of two perpendicular plates of the ethmoid bone (anterosuperior part of the
septum) and the vomer (posteroinferior part). In addition to these two, the cartilaginous part of the septum
nasi is a quadrangular-shaped cartilage that is connected to the nasal bone superiorly behind the bony septum
nasi. Anteriorly, it is fused with other cartilages forming the ala nasi and the dorsum of the nasi. Dorsum,
apex, alae: inside is hyaline cartilage in the shape of the bone (alae are semilunar shape).
The covering of the vestibule is the same as skin outside (skin continues inside) and in men (mostly) the
hair comes inside.
BLOOD SUPPLY AND INNERVATION:
This is given from two arteries and two nerves. First, the anterior ethmoidal artery and nerve come from
the ophthalmic artery (from internal carotid) and the nasociliary nerve (from the ophthalmic n.).
(Kiesselbach point: the anastomosis between the two arteries). These structures begin in the orbit, pass
through the anterior ethmoidal foramen and canal to the fossa cranii anterior, then down to the nasal cavity
through the lamina cribrosa. They innervate and supply the superior part of the nasal cavity. The inferior,
main part of the nasal cavity, is innervated by the posterior nasal nerve that comes from the maxillary nerve,
and is supplied by the sphenopalatine artery that comes from the maxillary artery.
The facial and glossopharyngeal nerves supply all the glands in the head and neck. Glands of the nose
and the lacrimal gland are innervated by the sphenopalatine ganglion via the greater petrosal nerve from the
facial nerve.
45
NECK
SUBMANDIBULAR REGION
Superior: body of the mandible,
Inferior: anterior and posterior bellies of the digastric muscle.
SKIN INNERVATION:
Cervical plexus (transverse coli nerve).
Removing the skin, you will find the platysma first, which belongs to the muscles of facial expression.
The superficial cervical fascia, which is the continuation of the parotidomasseteric fascia, lies beneath the
platysma This fascia covers the submandibular gland, the main structure of the submandibular triangle.
Removing the fascia exposes the gland, which is pierced by the facial artery. The floor of the
submandibular triangle is the mylohyoid muscle. The two mylohoid muscles are connected in the midline
by a raphe, forming the diaphragm of the oral cavity (diaphragma oris). The submandibular gland lies on
the mylohyoid muscle.
To lift the submandibular gland, first lift the anterior border, because the duct arises from the posterior
part. If you remove the gland, you will find two tiny structures superficial to the mylohoid muscle: the
mylohyoid nerve and the submental artery.
Removing the superficial structures, the sulcus lateralis linguae, between the mylohyoid muscle (lateral
wall) and the hyoglossus muscle (medial wall, with the hyoid bone and tongue), can be seen. This is a Vshaped space. Three structures pass through it: the LINGUAL NERVE (superior), the SUBMANDIBULAR DUCT
(middle), and the HYPOGLOSSAL NERVE (inferior).
Lingual nerve: innervating the anterior 2/3 of the tongue carrying: 1 taste-sensory and secretory fibers to
the sublingual and submandibular gland and to the tiny glands of the tongue. 2Taste-sensory fibers for the
anterior 2/3 of the tongue. 3General sensory fibers for the anterior 2/3 of the tongue. So, the lingual nerve
contains three types of fibers: taste, sensory, and secretory.
The posterior muscle of the tongue is innervated by the glossopharyngeal nerve by all the three types of
fibers.
The taste-secretory fibers of the lingual nerve are given by the facial nerve (via chorda tympani) that joins
the lingual nerve in the hiatus pterygoidei (between the two pterygoid muscle).
The submandibular duct opens into the oral cavity on the caruncula sublingualis that are two tiny
elevations (papillae) on the frenulum linguae. The main duct of the sublingual duct also opens on this
caruncula. The other tiny duct of the sublingual gland are opening lateral to the caruncula sublingualis.
The hypoglossal nerve passes through the carotid triangle from between the internal jugular vein and the
internal carotid artery, medial to the posterior belly of the digastric. After that, it goes into the sulcus
lateralis linguae and then into the tongue. The hypoglossal nerve is the motor nerve for the extrinsic
(styloglossus, hyoglossus, genioglossus) and intrinsic (3 directional) muscles of the tongue.
All these muscles are innervated by the hypoglossal nerve that innervates also the tiny geniohyoid
muscle.
Another important structure in this region is the lingual artery, which is not a structure of the sulcus
lateralis linguae. It is located deep to the sulcus, covered by the medial wall of the sulcus (hyoglossus
muscle), so to see it, you should cut this muscle. The arises from the external carotid artery and goes in the
Pirogow triangle. The Pirogow triangle is formed by the hypoglossal nerve (superior), the tendon of the
46
digastric muscle (inferior), and by the posterior border of the mylohyoid muscle (anterior) [Tájanatómia
p.222]
The posterior belly of the digastric muscle and the stylohyoid muscle are innervated by the facial nerve.
The suprahyoid muscles have different innervations: the anterior belly of the digastric and mylohyoid
are innervated by the mylohoid nerve. The posterior belly of the digastric and the stylohyoid are innervated
by the facial nerve.
The infrahyoid muscles are innervated by one nerve called the ansa cervicalis.*
*Some sources recognize a single ansa cervicalis; others recognize an ansa cervicalis superficialis (formed from the transverse
cervical nerve and the cervical branch of the facial nerve) which innervates the platysma and overlying skin
and an ansa cervicalis profundus (superior root from the hypoglossal nerve; inferior root from C2 & C3) which inner
vates the infrahyoid muscles. In this case, the thyrohyoid is described as receiving innervation directly from the supe
rior root of the deep ansa cervicalis. Ask your lab instructor.
In the posterior part of the region, we have the internal jugular vein, the internal and external carotid
arteries, the hypoglossal nerve , and the accessory nerve. The accessory nerve runs on the levator scapulae
muscle (parallel) and one branch of it pierces through the sternocleidomastoid muscle. The other branch
descends on the levator scapulae muscle and enters the trapezius muscle. The branch that goes to the
sternocleidomastoid muscle is located in the very posterior part of the region (out of the triangle). The
vagus nerve (between the internal jugular vein and the internal carotid artery) is also found here.
CAROTID REGION (aka Carotid Triangle)
Superior: posterior belly of the digastric muscle,
Posterior: sternocleidomastoid muscle,
Inferior: superior belly of omohyoid muscle.
SKIN INNERVATION:
Transverse coli nerve (cervical plexus). The transverse coli nerve forms an ansa with the cervical (or
descending) branch of the facial nerve called superficial cervical ansa (not dissectable and not important - see
note above).
Removing the skin, we can find the platysma and then the superficial cervical fascia. This fascia
ensheathes the sternocleidomastoid muscle and covers the infrahyoid muscles. It is very thick below the
hyoid bone and thin above it. So, you can say that the fascia covering the submandibular gland is very thin
and sometimes is not even mentioned!
Beneath the superficial cervical fascia, the middle cervical fascia (or pretracheal) ensheathes all the
infrahyoid muscles and forms the carotid sheath (or vagina). It also forms a capsule for the thyroid gland.
So, in this region, you can see 1 the anterior border of the sternocleidomastoid muscle, 2 the superior belly
of the omohyoid muscle, 3 the posterior belly of the digastric muscle, and 4 the thyrohyoid muscle.
The main structures are the common carotid artery; hypoglossal, accessory, and laryngeal nerves; internal
jugular vein; and the vagus nerve (CN X); all inside the sheath. In this region, we can see the division of the
common carotid artery (into external and internal carotids) and three branches of the external carotid artery.
To distinguish between the internal and external carotid arteries, you should know that the external carotid
gives branches here, but the internal carotid does not have any branch outside the skull. Also, the external
carotid is anterior, and the internal carotid is posterior.
In front of the carotid sheath (on the anterior scalene muscle), the ansa cervicalis (motor nerve for the
infrahyoid muscles) goes together with the hypoglossal nerve and is from the cervical plexus:
Behind the carotid sheath is the sympathetic trunk.
47
From the external carotid artery, we have branches here:
Superior thyroid artery, which has an additional branch called the superior laryngeal artery running
together with the superior laryngeal nerve (coming from the vagus nerve). Both the nerve and the
artery pierce through the thyrohyoid membrane and reach the larynx (innervating its upper part).
The superior laryngeal nerve has a branch that remains out of the larynx, called the external branch,
descending to the cricothyroid muscle and innervating it. The cricothyroid is the only muscle of the
larynx that is not innervated by the inferior laryngeal nerve (from the thoracic part of the vagus).
The Vagus nerve starts at the level of the jugular foramen, then it descends to the carotid sheath,
entering the thoracic cavity and innervating the organs of the thoracic cavity. From the thoracic
cavity, it descends into the abdominal cavity and innervates the organs of the abdominal cavity until
the last colic flexure (including the main part of the large intestine). The rectum and the last part of
the large intestine are innervated from fibers of the spinal cord.
The superior thyroid artery supplies the thyroid gland together with the inferior thyroid artery (from
the subclavian artery).
Ascending pharyngeal artery, supplying the pharynx and ascending on the wall of the pharynx. It
arises from the division of the common carotid artery (on the inner surface).
Lingual artery, located on the superior part of the region (more detail previously).
SUPRACLAVICULAR REGION (aka the Supraclavicular triangle)
Anterior: sternocleidomastoid muscle,
Posterior: trapezius muscle,
Inferior: clavicle.
This triangle is divided by the inferior belly of the omohyoid muscle into two triangles: the omoclavicular
(inferior and anterior), and the omotrapezoid (posterior).
Removing the skin, you can find the platysma, then the superficial cervical fascia that ensheathes the
sternocleidomastoid muscle. Beneath the fascia, the middle cervical fascia ensheathes the infrahyoid
muscles. The middle cervical fascia (or pretracheal) forms a thick layer between the tendon of the
omohyoid muscle and the clavicle and this tendon is attached to the carotid sheath and through this sheath, to
the wall of the internal jugular vein. In this way, the omohyoid muscle prevents the vein from collapsing
because of the negative pressure inside the thoracic cavity. Inside the thoracic cavity, between the two
layers of the pleura (between the lung and the thoracic cavity) there is a negative pressure (vacuum). So, the
thin wall of the vein would collapse. To prevent this, the omohyoid muscle is attached to it and keeps it
dilated.
Omohyoid muscle has two bellies: Superior and inferior. The superior belly is attached to the hyoid
bone and the inferior is attached behind onto the superior transverse scapular ligament. The two bellies
meet each other at the level of the internal jugular vein, forming a tendon.
The sternocleidomastoid muscle (the name includes the origin and insertion). The origin is the
sternum and medial end of the clavicle, and the insertion is the mastoid process.
Trapezius muscle (see "Upper Limb").
The main structure of the (omotrapezoid triangle) is the cervical plexus. The cervical plexus is a
network formed by the ventral rami of the spinal nerves of C1-C4. The cervical plexus is located at the
origin of the scalenus muscles. They arise from the transverse processes of the cervical vertebrae.
There are only two motor branches: 1) Phrenic nerve, and 2) Ansa cervicalis (inferior root). The
phrenic nerve arises from the C4 segment (mainly) and it descends on the anterior surface of the scalenus
anterior muscle. This nerve is together with the ascending cervical artery (from the sub-clavian).
The other branches of the cervical plexus are sensory: 1) Transverse coli nerve: it comes out to the
surface from the posterior border of the sternocleidomastoid muscle and there it runs transversely. 2)
48
Greater auricular nerve: it ascends on the sternocleidomastoid muscle behind the ear, and innervates a small
part behind and below the ear. 3) Lesser occipital nerve (see Nuchal Region). 4) Supraclavicular nerve.
On the posterior part of the region, we can find the accessory nerve (the descending branch that
innervates the trapezius).
In the omoclavicular triangle, the superficial cervical artery come from the thyrocervical trunk (from
subclavian). It goes from medial to lateral, above the inferior belly of the omohyoid muscle.
The superficial cervical artery is also called the transverse cervical artery.
OMOCLAVICULAR TRIANGLE:
In this triangle, you can find the hiatus scaleni, which is between the anterior and middle scalenus
muscle. The two structures of this hiatus are the trunks of the brachial plexus and the subclavian artery.
The brachial plexus forms trunks above the clavicle: Superior (C5, C6); Middle (C7); Inferior (C8, T1).
On the neck, the branches of the of the superior trunk are:
Long thoracic nerve (inferior - pierces through the scalenus middle muscle),
Dorsal scapular nerve (superior - pierces through the scalenus middle muscle),
Suprascapular nerve (runs along side the clavicle, backward).
Nerve to the subclavius (between the clavicle and the 1st rib).
Branches of the subclavian artery passing through the hiatus scaleni:
Suprascapular artery (from the thyrocervical trunk),
Transverse coli artery (from 3rd part of the subclavian). It runs deep between the trunks of the
brachial plexus.
The deep cervical fascia (or prevertebral) covers the scalenus muscles (anterior, middle, and posterior).
SCALENOTRACHEAL FOSSA
It's not exactly a region because it is a deep part of the supraclavicular region. The name includes where
it is: between the scalenus anterior muscle and the trachea. In the scalenotracheal fossa, there are
longitudinal and transverse structures. The longitudinal structures are the structures of the carotid sheath
and those parallel to it. The transverse structures are branches of the subclavian artery passing through the
fossa. These arteries are thyrocervical trunk and its branches (mainly the inferior thyroid artery). The
inferior thyroid artery goes to the thyroid gland and crosses a nerve in the scalenotracheal fossa; the inferior
laryngeal nerve (or recurrent laryngeal nerve).
The recurrent laryngeal nerve comes from the thoracic cavity. The left recurrent laryngeal nerve
hooks around the aortic arch and the right nerve goes around the right subclavian artery because both develop
from the 4th branchial arteries. The nerve of the branchial arch is the vagus nerve. So, the nerves and the
arteries developing from the same arches are together. From a surgical point of view, this crossing is very
important because if a surgeon operates on the thyroid gland, he has to ligate first the superior and inferior
thyroid arteries to cut the gland. If the surgeon cuts this nerve, the patient will have a big problem, because
the inferior laryngeal nerve innervates all the muscles of the larynx (except one), and the voice of the patient
will be affected..
The fossa also includes the first branch of the subclavian artery, the vertebral artery, which ascends
through the transverse foramen of the cervical vertebrae (see Nuchal Region). Another branch of the
subclavian artery descends in this region called the internal thoracic artery, running parallel with the
sternum.
The third branch of the subclavian artery is the thyrocervical trunk, and all the first three branches from
the thoracic part of the subclavian artery.
Branches of the thyrocervical trunk: Suprascapular artery (below the omohyoid muscle), Superficial
cervical artery (above the omohyoid muscle), Inferior thyroid artery.
49
Sympathetic and parasympathetic are the two main parts of the autonomic nervous system. The cervical
part of the sympathetic trunk has three ganglia: superior, middle, and inferior cervical ganglia. THE MIDDLE
GANGLION IS LOCATED IN THE SCALENOTRACHEAL FOSSA. From the middle cervical ganglion, fibers
surrounding the subclavian artery are called the ansa subclavia.
Branches of the subclavian artery:
THORACIC PART: (medial to the scalenus anterior muscle)
Vertebral artery,
Internal thoracic artery (arising opposite the vertebral artery, sometimes opposite to the thyrocervical
trunk).
a) Pericardiacophrenic artery
b) Superior epigastric artery
Thyrocervical trunk,
a) Inferior thyroid artery (first ascends and then turns inferiorly forming a hook)
Ascending cervical artery
Inferior laryngeal artery
b) Superficial cervical (or transverse cervical) artery: anastomoses with the deep cervical.
c) Suprascapular artery
MUSCULAR PART: (behind the scalenus anterior muscle)
Costocervical trunk,
a) Deep cervical artery
b) Highest intercostal artery (supplies the first two intercostal spaces)
CERVICAL PART: (lateral to the scalenus anterior muscle)
Transverse coli artery (or dorsal/descending scapular), runs laterally and backward between the
trunks of the brachial plexus.
MEDIAN COLI REGION (OR ANTERIOR)
Superior: hyoid bone,
Inferior: insisura jugularis of the sternum,
Lateral: superior belly of the omohyoid muscle and sternocleidomastoid muscle.
In this region, we can find infrahyoid muscles, namely the sternohyoid muscle (between the manubrium
sterni and the hyoid bone), superior belly of the omohyoid muscle, thyrohyoid muscle (covered by the
sternohyoid muscle). All these muscles are innervated by the ansa cervicalis and are surrounded by the
middle cervical fascia (or pretracheal) which forms a capsule for the thyroid gland.
In the midline, there is one vein (or occasionally, two lateral veins) called vena coli media (or two:
anterior jugular veins). These veins are drained into the external jugular vein. External jugular vein is
exactly on the sternocleidomastoid muscle and drains into the internal jugular vein or to the subclavian. The
external jugular vein starts behind the external hear as the retroauricular vein, and also receives veins from
above the scapula as suprascapular veins and the anterior jugular vein. If the vein is inside (deep to) the
sternocleidomastoid muscle, it must be the internal jugular vein, and if it is outside, it must be the external
jugular vein.
There is another vein which is deep to the muscles, and it arises from the thyroid gland and is the main
structure of the region. This vein is called inferior thyroid vein, and it starts from the gland as a plexus and
later it becomes one vein. The inferior thyroid vein drains into the left brachiocephalic vein and is also
called vena inferior impar and the plexus-plexus impar ("impar" means single).
The thyroid gland is located at the two sides of the trachea and has a capsule. It has two lobes, and
sometimes it has a middle lobe called pyramidal lobe. The arteries of the gland arise from the superior and
50
inferior thyroid artery. Above the thyroid gland, the cricothyroid muscle belongs to the laryngeal muscles
and is innervated by the superior laryngeal nerve (external branch).
Two laryngeal cartilages (thyroid & cricoid) are in front. Between the two cartilages, the conic ligament
(or median cricothyroid ligament - cricothyroideum medianum) has an important clinical use! Sometimes,
the larynx has an allergic reaction and the space of the larynx, where air goes through the trachea, will be
closed (). In this case, transection of the ligament allows air to enter the trachea below the larynx. This
procedure is called conicotomy.
Above the thyroid cartilage, there is a membrane called the thyrohyoid membrane (between the thyroid
cartilage and the hyoid bone). On the lateral part of this membrane (not in the region), the superior
laryngeal artery and nerve pierce this membrane, going to the larynx.
NUCHAL REGION
Superior: external occipital protuberance,
Inferior: vertebral prominence (7th cervical),
Lateral: along side of the mastoid process.
SKIN INNERVATION:
Lesser occipital nerve (branch of the cervical plexus), Greater occipital nerve (dorsal branch of the
spinal nerve coming out from the 2nd spinal segment), and Tertial occipital nerve (dorsal branch of the 3rd
spinal nerve).
To remove the skin, make a cut in the midline along side of the spinous processes of the cervical
vertebrae. Beneath the skin, the superficial nuchal fascia, covers the trapezius and laterally the splenius
capitis. It you remove the fascia, you will see the trapezius. Beneath the trapezius, lies the splenius capitis
muscle, a V-shaped muscle originating from the spinous processes of the lower cervical and upper thoracic
vertebrae and ascending to the superior nuchal line of the occipital bone. The lateral part of the splenius
capitis is called the splenius cervices because lateral fibers do not ascend to the skull, but they terminate on
the transverse processes of the cervical vertebrae.
Cutting the splenius capitis and cervicis, you will see the semispinalis capitis muscle, an upside-down Vshaped muscle originating from the transverse processes of the upper thoracic and lower cervical vertebrae
and inserting to the superior nuchal line, medial to the splenius capitis. The semispinalis and splenius
capitis make the rounded shape to the back of the neck.
Before cutting these muscles, find the great occipital nerve and the tertial occipital nerve coming out from
the deep through these muscles, becoming superficial, and turning onto the head.
Together with the lesser occipital nerve, we have the occipital artery (a little deeper).
Deep to the semispinalis capitis, the deep nuchal fascia covers the suboccipital triangle and the
semispinalis cervicis muscle.
The suboccipital triangle is made of three muscles: the rectus capitis posterior major, obliquus capitis
superioris, and obliquus capitis inferioris. The rectus capitis posterior major arises from the spinous
process of the axis and is inserted to the inferior nuchal line (medial part). The obliquus capitis inferioris
muscle arises from the same place and is inserted to the transverse process of the atlas. The obliquus capitis
superioris arises from the transverse process of the atlas and ascends to the skull to the lateral part of the
inferior nuchal line.
The rectus capitis posterior minor muscle is medial to the rectus capitis posterior major and is shorter
because it arises from the posterior tubercle of the atlas and the inferior occipital line.
Inside the suboccipital triangle, the main structure of the region is the vertebral artery, located on the
posterior arch of the atlas (in the vertebral sulcus). The vertebral artery comes from the subclavian artery
(inside the foramen transversarium) and goes up to the atlas. On the atlas, it runs a little lateral, then turns
medially. Then, it pierces through the posterior atlantooccipital membrane and enters the skull to supply the
brain (together with the internal carotid artery).
51
Inside the suboccipital triangle, runs the suboccipital nerve (from the dorsal ramus of the 1st spinal
nerve). The suboccipital nerve emerges between the atlas and the occipital bone and supplies the muscles of
the suboccipital triangle (Tájanatómia p. 333).
At the lateral border of the region, you can see the sternocleidomastoid muscle (arising from the
manubrium sterni and medial third of the clavicle and inserting to the mastoid process of the temporal bone
and the occipital bone).
IMPORTANT IN THIS REGION ARE THE LAYERS OF THE MUSCLES:
Superficial nuchal fascia, trapezius, splenius capitis, semispinalis capitis, deep nuchal fascia,
suboccipital triangle, and the semispinalis cervicis.
3 CERVICAL FASCIAS
Superficial cervical fascia: ensheathes the sternocleidomastoid muscle and covers the infrahyoid
muscles.
Middle cervical fascia (or pretracheal): thick in front of the sternocleidomastoid muscle and thin
behind. It ensheathes all the infrahyoid muscles, forms a capsule for the thyroid gland, and forms also the
carotid sheath (vagina).
Deep cervical fascia (or prevertebral): covers the scalenus muscles, the deep cervical muscles (namely
the longus coli and longus capiti). It also covers the sympathetic trunk.
In this way, as the prevertebral fascia covers the scalenus muscles (close the inlet of the thoracic cavity),
it forms a tent (pyramid-shaped). This fascia that covers the scalenus muscles has a layer which is sagittal
and lateral to the trachea and esophagus, separating the neck into three regions. The middle region is
between the two sagittal layers, while the two lateral regions contain the scalenus muscles and many other
structures. Inside this tent, we have the apex of the lung. So, the apex of the lung is above the clavicle,
approximately 1 cm.
PHARYNX
The pharynx is a tube which has posterior and lateral walls. It has no anterior wall because anteriorly, it
communicates with the oral cavity, nasal cavity, and larynx. The muscles forming the lateral and the
posterior wall arise from the pterygoid process of the sphenoidal bone. The first part of the pharynx is a
fascia (membrane) called the pharyngobasilar fascia that arises from the basilar part of the occipital bone and
is inserted to the superior constrictor muscle.
After this very short fascia, the next part of the pharynx is the superior constrictor muscle. It has four
origins: 1 from the pterygoid process of the sphenoid bone, and this part is called the pterygopharyngeal
part; 2 from the pterygomandibular raphe (between the pterygoid process and mandible), and this part is
called the buccopharyngeal part because the buccinator muscle arises from the same raphe; 3 from the
mylohyoid line, and this part is called the mylopharyngeal part; 4 from the root of the tongue, and this part is
called glossopharyngeal part.
The third part is the middle constrictor pharyngis muscle which overlaps the superior. It arises from the
greater and lesser horns of the hyoid bone. The borderline between the superior and the middle constrictor
pharyngis muscles is marked by the stylopharyngeus muscle (entering the pharynx between them). The
glossopharyngeal nerve runs along the stylopharyngeus muscle.
The inferior constrictor pharyngis muscle has two parts: thyropharyngeal and cricopharyngeal parts
(according to their origins - thyroid and cricoid cartilages). The inferior constrictor overlaps the middle
constrictor muscle.
52
All three constrictors are inserted to the PHARYNGEAL RAPHE, a connective tissue septum on the posterior
wall of the pharynx. In addition, there are the levator muscles of the pharynx which are: 1stylopharyngeal
muscle, 2salpingopharyngeal muscle (inside the salpingopharyngeal fold, which is behind the ostium
pharyngeum tubae auditivae), 3palatopharyngeal muscle (forms the palatopharyngeal arch, which is behind
the palatine tonsils).
The cavity of the pharynx has three parts: Nasopharynx (or epipharynx), Oropharynx (or mesopharynx),
and Laryngopharynx (or hypopharynx).
NASOPHARYNX (or EPIPHARYNX)
It starts from the roof of the pharynx, which is formed by the basilar part of the occipital bone, until the
soft palate. Anteriorly, it communicates with the nasal cavity through the choanae. Below, it
communicates with the oropharynx. Superiorly, it communicates with the roof of the pharynx, and it has
another communication with the tympanic cavity through the auditory tube or ostium pharyngeum tubae
auditivae. Behind this opening, there is an elevation called the tubal elevation, or torus tubarius, formed by
the cartilaginous part of the auditory tube. From this elevation, we have a fold downward which is called
the salpingopharyngeal fold and a fold in front called the salpingopalatine fold. Behind and a little above
this tubal elevation, the pharyngeal recess is where the tubal tonsils are located. The fornix of the pharynx
is between the superior and posterior walls of the pharynx, and in the fornix, we have the pharyngeal tonsils.
The ostium pharyngeum tubae auditivae is at the level of the inferior nasal meatus. So, we have to go
through the inferior nasal meatus to reach the opening.
OROPHARYNX (or MESOPHARYNX)
It is also called pars oralis pharyngis. It starts from the soft palate and goes until the superior part of the
epiglottis. It communicates with the oral cavity through the oropharyngeal isthmus or isthmus faucium. Its
borders are the palatoglossal and palatopharyngeal arches (medial and lateral); Root of the tongue (inferior);
and Uvula (superior).
Vallecula epiglottica: between the root of the tongue and the epiglottis ("vallecula" is Latin for "little
valley"). It is bordered by the median glossoepiglottic fold and the lateral glossoepiglottic folds. A fish
bone may be stuck there.
Between the two arches (palatoglossal and palatopharyngeal), we have the tonsilar fossa, where the
palatine tonsils are located. Above the palatine tonsils, there is a fossa called supratonsilar fossa. A fish
bone may also be stuck there.
LARYNGOPHARYNX (or HYPOPHARYNX)
From the epiglottis until the esophagus. The most important structure is the inlet of the larynx, bordered
1
by: epiglottis (in front), 2 aryepiglottic fold (laterally), 3 insisura interarytenoidea (so named because it is
between the arytenoid cartilages), 4 tuberculum cuneiforme + corniculatum (not important).
The food from the oral cavity passes through the piriform recess which is in the two sides of the
epiglottis, then it goes to the esophagus.
53
INNERVATION:
The muscles of the pharynx and the mucous membrane are innervated by the glossopharyngeal nerve
(upper part) and the vagus nerve (lower part). The pharyngeal plexus is formed by the two nerves and by
some sympathetic fibers of the sympathetic trunk (cervical part).
BLOOD SUPPLY:
The main artery that supplies the pharynx is the ascending pharyngeal artery (from the external carotid).
LARYNX
It starts from the aditus laryngis and it has three main parts: a) vestibule, b) ventricle, c) infraglotic cavity.
VESTIBULE
It starts with the aditus laryngis. If you go through the aditus, you arrive into the vestibule. The
inferior border of the vestibule is the ventricular (or vestibular) fold, and the lateral wall is formed by the
quadrangular membrane. This membrane has four borders (as the name indicates): Anterior, epiglottis;
Posterior, arytenoid cartilages. The superior and inferior borders are free. The free superior border forms
the aryepiglottic fold (it is covered by mucous membrane forming a fold). The free inferior border forms
the ventricular fold. This fold is sometimes called the vestibular fold because it is the borderline between
the ventricle and vestibule. This fold is called the false vocal ligament (or vestibular ligament). It is above
the true vocal ligament and a little lateral.
VENTRICULUM LARYNGIS (or laryngeal sinus)
It is recessed a little laterally, and after that, the most constricted part of the larynx is the rima glotidis or
glottis. It is bordered superiorly by the ventricular fold and inferiorly by the vocal fold.
INFRAGLOTTIC CAVITY
The cavity which is below this glottis is called infraglottic or subglottic cavity. It becomes dilated,
giving the larynx an hour-glass shape (or water clock - clepsydra). The wall of the cavity is formed by the
conus elasticus (elastic membrane with a cone shape) which is attached to the thyroid cartilage (in front) and
to the cricoid cartilage (behind). This anterior part, between the cricoid and thyroid cartilages, is called the
conic ligament or median cricothyroid ligament. The membrane is also attached posteriorly to the arytenoid
cartilages, and the superior border forms the vocal ligament. The vocal ligament, together with the vocalis
muscle, forms the vocal fold. The vocal ligament arises from the thyroid cartilage (in front) and to the
arytenoid cartilages (behind). The two vocal ligaments form a space which is V-shaped and is called the
rima glottidis. Rima glottidis has two parts: the anterior is between the vocal ligaments and is called the
intermembranous part, and the posterior is between the two arytenoid cartilages and is called the
intercartilaginous part.
Cartilages:
Thyroid: It has two lamina (dextra et sinistra). They meet in front in an angle called prominencia
laryngis ("Adam's apple"). Posteriorly, the thyroid cartilage is open. Anterosuperiorly, the two
lamina meet, forming a notch called the incisura thyroidea superioris. The posterior thyroid
cartilage has two horns (on each lamina). The inferior horn has a joint with the cricoid cartilage
called the articulatio cricothyroidea. The axis of the joint is transverse, and the muscle that acts on
this joint is the cricothyroid muscle. The lamina has a line which is called linea obliqua, and there,
muscles attach or insert.
Cricoid: It has a ring shape. It has a lamina posteriorly and an arch anteriorly. On the lamina,
there are two articular surfaces for the arytenoid cartilages, and forming the cricoarytenoid joints.
The axis of these joints is longitudinal, going through the superior apex of the arytenoid cartilages.
54
The muscles that work on this joint are the cricoarytenoid posterior and lateral muscles and partly the
interarytenoid muscles (not exactly).
Arytenoid: Pyramidal in shape. It has articular surfaces that are related to the cricoarytenoid joint.
It has medial, posterior, and lateral surfaces. It has a base and an apex. On the apex, we have the
corniculate cartilage. There is a muscle on the lamina of the cricoid cartilage called the
cricoarytenoid posterior muscle (the only muscle that opens the rima glotidis). This muscle moves
the muscular process medially. Because the axis is in the middle of the arytenoid cartilage, the rima
glottidis opens.
The antagonistic muscle of the posterior cricoarytenoid is the lateral cricoarytenoid muscle,
arising from the arch of the cricoid and inserting to the muscular process. Its action is opposite that
of the posterior cricoarytenoid, thus closing the rima glottidis (the main closing muscle).
There is a muscle between the thyroid cartilage and the lateral surface of the arytenoid cartilage. Some
medial fibers of it are inserted to the vocal ligament, forming the vocalis muscle. The other whole muscle is
called the thyroarytenoid muscle. So, this muscle increases the tension of the vocal ligament (making the
ligament harder and tenser). The vocalis muscle is also the fine modulator of our voice: if the ligament is
tenser, the voice is higher, and if it is looser, the voice is lower.
There is another muscle between the arytenoid cartilages which is called the interarytenoid muscle (or
arytenoid muscle). Its function is to close the posterior intercartilaginous part of the rima glottidis. This
muscle has transverse fibers and oblique fibers. Some of the oblique fibers ascend into the aryepiglottic
fold, and this part is called the aryepiglottic muscle. The function of this muscle is to constrict the aditus
laryngis.
The thyroarytenoid muscle has also some ascending fibers that ascend into the quadrangular membrane
forming the thyroepiglottic muscle. This muscle is the antagonistic muscle of the aryepiglottic muscle,
because it constricts the vestibule itself and opens the aditus laryngis.
The cricothyroid muscle is at the external surface of the cricoid cartilage and arises from the arch of the
cricoid cartilage and is inserted into the lamina of the thyroid cartilage, having straight fibers and oblique
fibers. This muscle works on the cricothyroid joint. It moves the anterior part of the cricoid cartilage
toward the thyroid cartilage. If the cricoid is fixed, it moves the thyroid toward the cricoid.
SENSORY INNERVATION:
Above the rima glottidis: superior laryngeal nerve (pierces through the thyrohyoid membrane together
with the superior laryngeal artery.
Below the rima glottidis: inferior laryngeal nerve.
The hyoid bone is connected with the thyroid cartilage by the thyrohyoid membrane (anteriorly) and to
the thyrohyoid ligament (posteriorly) which is between the greater horn of the hyoid bone and the superior
horn of the thyroid cartilage.
55
PARAPHARYNGEAL SPACES
Lateral to the pharynx, we have the parapharyngeal spaces:
Medial wall: pharynx,
Lateral wall: medial pterygoid muscle, ramus mandibulae, and masseter muscle,
Anterior: Bichat's fat pad (corpus adiposum buccae),
Posterior: styloid muscles, digastric, and sternocleidomastoid muscles,
Inferior: submandibular triangle.
Structures:
Glossopharyngeal nerve (CN IX),
Vagus nerve (CN X),
Accessory nerve (CN XI),
Hypoglossal nerve (CN XII),
Internal jugular vein,
Superior cervical ganglion of the sympathetic trunk,
Internal carotid artery.
The parapharyngeal space is also called the peritonsilar space because only the pharyngeal wall separates
the palatine tonsil and the lymphatic vessels of the palatine tonsils going through this space into the deep
cervical lymph nodes. The other reason for the importance of this space is that the internal carotid artery
sometimes forms a loop which is close to the pharyngeal wall. If you operate on the palatine tonsil, be
careful not to cut too deep because we may cut the pharyngeal wall and the internal carotid artery.
RETROPHARYNGEAL SPACE
It is located behind the pharynx, so the anterior wall is the pharynx. The posterior wall is the prevertebral fascia. Laterally, it is separated from the parapharyngeal space by connective tissue (not a wall).
Inferiorly, it leads to the posterior mediastinum, and for this reason this space is important. Any infection
on the posterior wall of the pharynx could be spread to the retropharyngeal space. From this space,the
thoracic cavity (posterior mediastinum) is accessible.
56
THORAX
LUNGS
Segments:
The segments are the morphological, functional, pathological, and surgical units of the lung. The
segment is a pyramidal shaped part of the lung. The apex of the pyramid is facing toward the hilus, and the
base faces toward the surface of the diaphragm. At the apex of this pyramid, the segmental bronchus enters
the segment together with the segmental branch of the pulmonary artery. So, in the center of the segment,
we have the bronchus tree and the pulmonary artery (next to each other). Segments are separated from each
other by connective tissue septa. Inside this connective tissue are the pulmonary veins and lymph vessels
running toward the hilus. So, the veins are collected toward the periphery of the segment running inside the
connective tissue of the septum, but the artery and the bronchus tree are running in the center of the segment.
We can remove one segment surgically if there is a disease or tumor.
The segment is composed of smaller units called lobules. The lobules are the same pyramidal shape, but
they are smaller. Inside the lobule, are the bronchioli. One lobule belongs to one terminal bronchus which
is branching inside the lobule forming bronchioli. The difference between bronchi and bronchioli-- no
cartilage, no glands, but there is smooth muscle.
On the surface of the lung, you can see small, approximately 1-2 cm areas bordered by black color
(surrounded) that are the lobules. We can see only the base because the base is facing toward the surface.
The black area is pollution inside the connective tissue that separates the lobules from each other (just as the
largest units, the segments, are separated from each other). So, the tiny lobules are visible on the surface.
In a newborn, the connective tissue is not black, but whitish.
There are ten segments in each lung:
Right: three in the superior lobe, two in the middle, and five in the inferior lobe.
Left: five in the superior lobe and five in the inferior. We don't have to know the names of the
segments.
Impressions:
RIGHT LUNG: impressions for the azygos vein (below and above the hilus) and also the superior vena
cava. Because the azygos vein drains into the superior vena cava, we also have the impressio cardiaca
pulmonis (impression for the heart).
LEFT LUNG: It has a wide impression called the aortic sulcus. It is made by the descending thoracic
aorta and the aortic arch. It also has the sulcus of the subclavian artery that is next to the apex.
On the costal surface, there are impressions for the ribs.
Lymphatic drainage:
Lymph from the lung is collected in the lymph nodes of the hilus and then to the bronchomediastinal
trunk. The bronchomediastinal trunk is collected by the thoracic duct.
Important features:
Bronchus tree.
Blood supply.
Double circulation (functional and nutritive).
Surface of the lung (anatomy notes- 2nd semester).
57
Structures in the lung:
From superior to inferior:
Left lung (artery, bronchus, vein)
Right lung (Bronchus, artery, vein)
From anterior to posterior:
Vein, artery, bronchus (in both lungs)
There is a difference between the right and left lungs. The right lung has three lobes, but the left has
only two lobes. These three lobes are separated by two fissures: one horizontal and one oblique. The
horizontal separates the superior lobe from the middle, and the oblique separates the middle from the inferior.
The inferior lobe is mainly behind, and in front, we have the superior and middle. The horizontal fissure
follows the fourth rib. The oblique starts from the horizontal fissure in the axillary line and crosses the 5 th
rib, terminating at the 6th rib (at the 6th sternocostal joint). So, in front, between the 4th and 6th ribs, if you
percuss a dullness, it means that there is a tumor or infection in the middle lobe. If you percuss something
above the 4th rib, it means that the infection is at the superior lobe. If you percuss it behind, it means that it
is in the inferior lobe.
In the case of the left lung, there is no horizontal fissure, but only the oblique fissure separating the
superior from the inferior lobe. The superior is in front, and the inferior is mainly behind.
PLEURA:
The lung is layered by the visceral pleura, and the chest wall, diaphragm, and mediastinum are layered by
the parietal pleura. So, the parietal pleura has three main parts: a) Costal (or sternocostal), b)
Diaphragmatic, and c)Mediastinal. Between the two mediastinal pleura, we have the mediastinum (middle
part of the thoracic part).
MEDIASTINUM
This is the middle part of the thoracic cavity, which is separated from the pleural cavities by the
mediastinal layer of the parietal pleura. Anteriorly, it is bordered by the sternum. Posteriorly, it is
bordered by the vertebral column.
The mediastinum is separated into anterior and posterior mediastina by the root (hilus) of the lung, which
is composed of the principal bronchi and the pulmonary arteries and vein. In front of the root of the lung,
we have the anterior mediastinum. Behind, we have the posterior mediastinum.
Below the root of the lung, the pulmonary ligament separates the anterior from the posterior mediastinum.
Above the root of the lung, there is no border between them. The pulmonary ligament is the reflection of
the visceral pleura into the mediastinal part of the parietal pleura.
The anterior mediastinum has two parts. In the inferior part of the anterior mediastinum, we have the
heart, so it's called the cardiac mediastinum. Above the heart, we have the supracardiac mediastinum. The
supracardiac mediastinum has four layers: 1 thymus, 2 venous (SVC), 3 arterial (aorta, aortic arch), 4 trachea.
The posterior mediastinum is behind the root and the pulmonary ligament.
The pleura is a little larger than the lung itself (mainly below the lung). So, you should know the
projections of the pleura, too. It is very easy, because the projections of the pleura to the chest wall is one
rib lower than the projection of the lung:
6th rib: parasternal line
7th rib: medioclavicular line
8th rib: anterior axillary line
9th rib: middle axillary line
10th rib: posterior axillary line
11th rib: scapular line
BUT: behind, the pleura is a little lower than one rib, so finally, it reaches the vertebral column at the level of
the 12th vertebra. So, it means that the space between the lung and the parietal pleura here is about 7-10 cm
(more than one rib).
58
Importance of the parietal pleura:
You can find recesses at the junction (or reflection) of the different parts of the parietal pleura. The
pleural recesses are formed only by the parietal pleura. In the pericardium, both visceral and parietal layers
make the recesses (know this difference).
The three different parts are continuous with each other. At the junction, there are recesses or sinuses:
Phrenicocostal recess: between the diaphragmatic and costal layers of the parietal pleura.
Phrenicomediastinal recess: between the diaphragmatic and mediastinal layers.
Costomediastinal recess: between the costal and mediastinal layers.
The phrenicocostal recess is the most important because:
CLINICAL: It is the lowest point of the pleural cavity, so the fluid inside the cavity is collected there.
We can drain this fluid and examine the quality (serous, blood, etc.)
PHYSIOLOGICAL: The lower margin of the lung descends into this sinus during inspiration. The
inferior border of the lung descends into this sinus.
You must know how to find the phrenicocostal recess. Your hand along the side of the ribs, and it will
stop at the diaphragm. So, there is a blind recess between the diaphragm and the ribs.
PROJECTIONS OF THE LUNG TO THE CHEST WALL
The lungs cover the heart except at one part, where the cardiac notch of the left lung is.
The apex of the lung is above the clavicle, approximately 1-3 cm above the 1st rib.
nd
The medial borders of the lungs run toward each other. The closest point is at the level of the 2 ribs.
At this point, the border of the right lung is in the midline of the sternum, and the medial border of the left
lung is at the left margin of the sternum. From the second rib, the medial border descends until the fourth
rib, where the left lung makes a notch between the 4th and 6th ribs, called the dardiac notch. The medial
border of the right lung descends straight down until the 6th rib. So, a part of the heart is not covered by
lung (between the 4th and 6th ribs, left side).
The inferior border of the lung starts from the 6th rib (upper border) and descends a little. In the
medioclavicular line, it crosses the inferior border of the 6th rib. At the anterior axillary line, it is at the level
of the 7th rib. At the middle axillary line, it is at the level of the 8th rib. At the posterior axillary line, it is
at the level of the 9th rib. At the scapular line, it is at the level of the 10th rib. At the vertebral column, it is
at the level of the 11th rib (10th vertebra).
TRACHEA
The bifrucation of the trachea is at the level of the 4th thoracic vertebra, and it starts at the level of the 6th
cervical vertebra below the cricoid cartilage.
RELATIONS:
Behind the trachea, runs the esophagus. At the two sides, we have the thyroid gland. Between the
esophagus and the trachea, there is a sulcus called the esophageotracheal sulcus where the recurrent (or
inferior) laryngeal nerve is located. The trachea is also related to the common carotid artery and the
brachiocephalic trunk (see supracardiac mediastinum). The brachiocephalic trunk and the left common
carotid artery arise just at the two sides of the trachea from the aortic arch. The trachea is also related to the
left brachiocephalic vein because it passes through the midline.
PRINCIPLE BRONCHI:
The left principle bronchus is related to the thoracic aorta. The right principle bronchus is related to the
azygos vein. So, on the right side, the azygos vein is turning around from behind and upward (making a
hook), riding on the principle bronchus.
59
Difference between right and left principle bronchi:
The right one is shorter, wider, more vertical, and a little more posterior than the left. The medical
importance that the right is more vertical and wider is that if you inspirate a foreign material, it is more
likely to enter the right lung.
POSTERIOR MEDIASTINUM
The mediastinum is the middle part of the thoracic cavity which is bordered laterally by the mediastinal
pleura, anteriorly by the sternum, and posteriorly by the vertebral column (thoracic part).
This middle part of the thoracic cavity is separated into two: the anterior and the posterior mediastinum,
and the borderline between these two is the hilus and the pulmonary ligament. The anterior mediastinum is
also divided into two parts: the cardiac, and the supracardiac mediastinum.
The posterior mediastinum contains several very important structures: the esophagus, vagus nerve,
sympathetic trunk, thoracic part of the descending aorta, thoracic duct, azygos vein, and hemiazygos vein.
Right side: vagus behind the esophagus.
Left side: vagus in front of the esophagus.
The thoracic duct is located between the azygos vein and the thoracic aorta, and is located in the right
posterior mediastinum. Approximately at the level of the 4th thoracic vertebra, it turns to the left side behind
the esophagus in front of the vertebral column, and it runs into the left venous angle, and it collects different
lymphatic trunks.
The thoracic duct arises from the CISTERNA CHYLI, located in the abdominal cavity behind the aorta at the
level of the 1st lumbar vertebra. The cisterna chyli collects the lymph from the lower limbs (posterior
abdominal wall) and from the abdominal viscera. The name of these trunks are the trunci lumbales dexter
and sinister (right and left lumbar trunk - lower limb and posterior abdominal wall) and the truncus
intestinalis (intestinal trunk - intestines). These three trunks drain to the cisterna chyli and from there, the
thoracic duct drains the lymph upward. The thoracic duct runs through the diaphragm, together with the
aorta (behind the aorta) through the aortic hiatus (right posterior mediastinum between the azygos vein and
the thoracic aorta). Its left relation is the thoracic aorta, its right relation is the azygos vein, and its anterior
relation is the esophagus. Approximately at the level of the 4th-5th thoracic vertebra, it passes to the left side
and enters into the left venous angle. Before entering, it collects the following lymphatic trunks: left
jugular trunk (left side, head and neck), left subclavian trunk (drains the left upper limb), and left
bronchomediastinal trunk (drains the lung and the thoracic cavity mediastinum, so the left part of the whole
thoracic cavity). So, you can say that the thoracic duct drains 3/4 of the body. The right superior quarter is
drained by the right lymphatic truncus (truncus lymphaticus dexter). It receives the same lymphatic trunks:
right jugular trunk, right subclavian trunk, right bronchomediastinal trunk, then drains into the right venous
angle.
The azygos vein starts in the abdominal cavity as the vena lumbalis ascendens (ascending lumbar vein).
In the abdominal cavity, it collects the segmental lumbar veins which drain the posterior abdominal wall. It
pierces through the diaphragm together with the greater and lesser splanchnic nerves between the medial and
lateral crus of its lumbar part. More particularly between the medial and intermedial crus (see below diaphragm). After piercing the diaphragm, it runs into the posterior mediastinum. At the right side it is
called azygos and at the left side is called hemiazygos. The azygos and hemiazygos collect the intercostal
veins in the thoracic cavity (drain the thoracic wall), the bronchial veins from the lungs, the esophageal veins,
and the external vertebral venous plexus (plexus venosus vertebralis externus), taking the blood from the
body of the vertebrae and some part of the spinal cord. They also collect veins from the mediastinum and
pleura. Only the intercostal veins are visible and dissectable. The others are tiny and not visible or
dissectible. The azygos vein receives the hemiazygos vein from the left side which collects the same veins
from the left side plus the accessory hemiazygos vein (above the junction between the azygos and
hemiazygos, there is no hemiazygos. This superior part of the vein, which drains superior into the
60
hemiazygos is called accessory hemiazygos vein). The accessory hemiazygos vein drains the superior
intercostal veins (approximately the upper five intercostal veins).
SUPRACARDIAC MEDIASTINUM
The supracardiac mediastinum has four layers:
Adipose thymus (just behind the sternum)
Layer of main veins (tributaries of the superior vena cava)
a) left brachiocephalic vein (oblique and long) approx. 10-12 cm.
b) right brachiocephalic vein (straight and short) approx. 2-3 cm.
(these form the superior vena cava)
Into the left brachiocephalic vein, drains the inferior thyroid vein (from the thyroid gland). Into the
superior vena cava, the azygos vein drains (structure of the posterior mediastinum, not the
supracardiac mediastinum).
Main arteries (branches of the aortic arch):
a) brachiocephalic trunk
b) left common carotid artery
c) left subclavian artery
The brachiocephalic trunk divides into two: right and common carotid and right subclavian arteries.
Between the layers of the main arteries and main veins, the vagus nerve and phrenic nerve enter the
thoracic cavity.
Trachea.
ESOPHAGUS
The esophagus has three parts: cervical, thoracic, and abdominal (very short). The thoracic part is located
behind the trachea, starting at the level of the 6th cervical vertebra and a little left to the midline. It has an
angustia cricoidea (at the beginning) because of the cricoid cartilage ["angustia" is a constriction]. From
the 3rd-4th thoracic vertebra, at the bifrucation of the trachea, the esophagus is located a little to the right of
the midline between the 4th and 8th thoracic vertebra. At the level of the 7th thoracic vertebra, it crosses the
aorta and from this point, it runs in front and left to the aorta. Finally, it pierces the diaphragm left and in
front of the aorta at the level of the 11th thoracic vertebra. There is also an angustia at the crossing with the
aorta and is called angustia aortica. The last is at the level of the diaphragm and is called angustia
diaphragmatica (level of 11th thoracic vertebra). Some text books describe another angustia at the level of
the bifrucation of the trachea (very small one angustia trachea).
Together with the esophagus, you should mention the vagus nerve.
61
THORACIC AORTA
The thoracic aorta is located in the left posterior mediastinum and it is riding on the left principle bronchus
forming an impression on the lung and have the crossing with the esophagus. It gives branches here which
are the anterior and posterior intercostal arteries and inferior thoracic artery. There are ten pairs because
the highest intercostal and the highest thoracic arteries supply the first two intercostal spaces. These ten
pairs arise from the posterior surface of the aorta. That's why they are not visible.
The aorta also gives the bronchial artery, usually through 2nd and 3rd intercostal arteries, but sometimes
directly from the aorta. The bronchial artery is a tiny artery– usually not dissectable– that gives the
nutritional circulation to the lungs.
SYMPATHETIC TRUNK
The sympathetic trunk is composed of twelve ganglia which are called paravertebral ganglia, located in
front of the heads of the ribs. These ganglia are connected with interganglionic fibers forming a chain of
ganglia. The preganglionic fibers come from the vertebral column by the spinal cord. Inside the spinal
cord (from the 1st thoracic to the 3rd lumbar segment of the spinal cord), the lateral horn has the vegetative
sympathetic neuron cell bodies. This means that the cervical part of the spinal cord and the sacral part of
the spinal cord do not have sympathetic neuron cell bodies. The cervical region has no vegetative neurons,
and the sacral part has parasympathetic vegetative. The other part of the parasympathetic is located in the
brain. "Para" means parallel to the sympathetic. Sympathetic is from the thoracolumbar region;
parasympathetic is from the craniosacral.
The preganglionic fibers originating from the lateral horn of the spinal cord pass through the ventral root
of the spinal cord, then through the spinal nerve and from the spinal nerve into the anterior and posterior
rami. From the spinal nerve, some fibers enter the sympathetic ganglia and terminate inside. These fibers,
between the spinal nerve and the ganglia, are called ramus communicans albus (white communicating fibers).
These fibers terminate in the ganglia and have synapses to the neuron cell bodies being inside the ganglia.
The axon fiber originating from the neuron cell body (inside the ganglion) turns back to the spinal nerve and
runs out inside the ventral and dorsal rami, out to the periphery, to the different glands and smooth muscle of
the blood vessels or of the skin (ex: smooth muscle of the viscera). These fibers, which arise from the
ganglion cell body, are called post-ganglionic fibers or ramus comminicans griseous (grey communicating
fibers). They don't have myelin sheaths, hence their grey color.
The fibers running toward the cervical sympathetic ganglia originate from the upper thoracic part of the
spinal cord. The axon runs through the ventral root of the spinal cord. The ventral root is motor, and the
dorsal root is sensory. In the dorsal root, there is a ganglion having sensory neuron cell bodies which are
pseudounipolar. This means that the axon originates as a single axon then immediately divides into two.
One goes into the center and the other out to the periphery somewhere, for example to a receptor (muscle
spindle or pain receptor, etc.). The direction of impulse is from the periphery into the center (afferent), and
from there to the cortex to feel the sensation.
There are also somatomotor fibers originating from the ventral horn of the spinal cord. They go out
innervating skeletal muscles. The direction of impulse is efferent (from the center to the periphery).
The masses of cell bodies of the periphery are called ganglia, and the masses of cell bodies inside the
sensor are called nuclei.
Inside the ventral root: vegetative motor, somatomotor fibers.
Inside the dorsal root: only sensory (pure) fibers.
Inside the spinal nerves: all three types of fibers (mixed).
Spinal nerves divide into two (dorsal and ventral) rami. The ventral rami form plexuses (brachial,
cervical, etc.) except in the thoracic part, where they remain segmented, forming the intercostal nerves.
There is another type of sympathetic fiber. They run through the ganglia without synapsing, forming the
splanchnic nerves. The 6th-9th ganglia give rise to the GREATER SPLANCHNIC NERVE. Ganglia 10 & 11 give
rise to the MINOR SPLANCHNIC NERVE. So, these fibers are preganglionic fibers passing through the
62
diaphragm together with the azygos vein and terminating in the celiac ganglion (a prevertebral ganglion
together with superior and inferior mesenteric and aorticorenal). These splanchnic nerves terminate in the
ganglia where they synapse. From there, postganglionic fibers run along the blood vessels and innervate the
blood vessels of the viscera and the smooth muscle of the abdominal viscera.
DIAPHRAGM
It separates the thoracic cavity from the abdominal cavity. Above the diaphragm, are the lungs inside
the pleural cavity. Between them, lies the pericardium having the heart. All three (lungs and heart) are in
the thoracic cavity. The highest level of the diaphragm is the 5th rib (liver).
See "the Abdomen" for a thorough discussion of the diaphragm.
HEART
Projections:
We determine the heart by four points: a) upper right point (entrance of the superior vena cava to the right
atrium), b) upper left point (left superior end of the sulcus coronarius), c) right inferior point (right lower end
of the sulcus coronarius), and d) left inferior point (apex of the heart).
RIGHT SUPERIOR POINT: is located at the third rib, 1cm right or the midline or next
to the right margin of the sternum (at the third rib) - or second intercostal space.
LEFT SUPERIOR POINT: 3 cm left of the sternum, also on the third rib.
RIGHT INFERIOR POINT: 1 cm right to the 6th sternocostal joint or at the right side of the
sternum.
LEFT INFERIOR POINT: 5th intercostal space, 9 cm left of the midline of the sternum.
If we connect these four points by a convex arch-shaped line, we get the margin of the heart. The
shorter axis of the heart is a line connecting the superior left and inferior right points. By connecting the
right superior point with the left inferior point, you will find the longer axis of the heart. The longer axis is
oblique from superior-right-posterior to inferior-left-anterior. That means that the apex of the heart is closer
to the chest wall than the superior vena cava (right atrium). This permits palpation of the heart beat on the
apex.
In the plane of the sulcus coronarius (the plane of the shorter axis), we have the fibrous ring (or annulus
fibrosus) of the heart which has the different ostia. There are four ostia: 1 right atrioventricular ostium (or
right venous), 2 left atrioventricular ostium (or left venous), 3 ostium aortae, 4 ostium trunci pulmonalis.
These ostia (or orifices) are called venous and arterial because through the venous ostia, blood flows into the
heart, and through the arterial ostia, the blood flows out from the heart. These descriptions are independent
from the quality of the blood (oxygenated or non-oxygenated).
PROJECTIONS OF OSTIA ON THE CHEST WALL:
Ostium of the Pulmonary Trunk: located on the left side, at the level of the third sternocostal
joint.
Ostium of the Aorta: right below the third rib, behind the sternum.
Ostium Venosum Sinistrum: at the level of the 4th sternocostal joint, left side.
th
Ostium Venosum Dextrum: at the level of the 5 sternocostal joint, right side.
The most superficial ostium is the ostium of the pulmonary trunk (closest to the chest wall). The
deepest is the left venous ostium. The importance of the ostia is that there are valves closing them.
63
Auscultating of the sounds of the valves (by phonendoscopy) is necessary to detect abnormal or pathological
functions (ie. stenosis).
The sound of the aortic valve will be auscultated at the 2nd intercostal space, 2 cm right to the sternum.
The aorta comes from the left ventricle, but we hear it on the right side because it crosses the pulmonary
trunk (embryology).
The bicuspid valve is on the left venous ostium, and the tricuspid is on the right venous ostium. The
sound of the bicuspid valve is auscultated at the apex (5th intercostal space, 9 cm left of the midline – or
midclavicular line) of the heart. The sound of the tricuspid valve will be auscultated at the 5 th intercostal
space, right side of the sternum (next to it).
The arterious ostia are closed by the semilunar valves, composed of a lunula and a nodulus. They open
in the systolic phase. At this phase, the venous valves (left and right atrioventricular valves) are closed. At
the diastolic phase, the arterious valves are closed and the venous valves are open. So, the beat of the heart
is: the first beat belongs to the closure of the atrioventricular valves, and the second belongs to the closure of
the arterial valves (aortic and pulmonary).
ABSOLUTE AND RELATIVE DULLNESS OF THE HEART:
Percussion of the chest above the lungs produces a sound, resulting from resonance within the air-filled
lung (1st and 2nd intercostal spaces).
Going down to the third intercostal space, the resonance will be dull due to the fluid-filled heart being
behind the lung. So, the sound changes, and this is called relative dullness. If you go down to the fourth
intercostal space (near the sternum), the sound will be more dull because the lung does not cover the heart.
The sound reaches only the blood-filled heart, and therefore no resonance. This sound is called absolute
dullness. The region of absolute dullness is at the level of the 4th -5th intercostal spaces (left side). The
size of the absolute dullness area gives the size of the cardiac notch. Absolute dullness is not so important
as the relative dullness because the relative dullness marks the upper border of the heart. If you hear the
relative dullness at the 2nd intercostal space instead of the 3rd, it means that the heart is enlarged superiorly.
You must also know where to percuss the right and left points of the heart. For the right border, place
your finger parallel to the expected border, and you will hear the dullness at the right side of the sternum. If
you hear the dullness farther from the right side of the sternum, it means that the heart is enlarged to the right.
For the left border, place your finger parallel to the expected border. Normally, you can find it left of the
medioclavicular line. If the heart is enlarged, it will exceed the medioclavicular line to the left.
The heart is surrounded by the pericardium. The pericardium has parietal and visceral layers. The
parietal pericardium reflects to the visceral layers. The arterious reflections are exactly at the division of the
pulmonary trunk. On the aorta, they are at the beginning of the aortic arch (so, below the right
brachiocephalic trunk). Thus, the whole ascending aorta and the pulmonary trunk are inside the pericardiac
cavity. The venous reflection on the superior vena cava is at the entrance of the azygos veins into the
superior vena cava. There is also a reflection on the inferior vena cava which is where the vein pierces
through the diaphragm. So, the whole thoracic part of the inferior vena cava (approximately 1 cm) is inside
the pericardiac cavity. The main part of the inferior vena cava is inside the abdominal cavity. There are
also reflections at the pulmonary veins (approximately 1-2 cm are inside the pericardiac cavity). These
reflections form a letter "T" which is called Sappey's T.
During embryonic development, the heart tube is initially straight down with the venous end below and
the arterious end above. Then, the venous end migrates upward and behind the arterious end, and if forms a
"U" shaped tube. There is a reflection (visceral - venous) behind and upward, and the venous reflection
which was below will now be behind the arterious reflection. Between the arterious and venous reflections,
there is a pericardiac sinus called the transverse sinus of the pericardium. The transverse sinus is found
between the main arteries and the main veins. The main veins develop from the venous end, and the main
arteries develop from the arterious end. Finally, the transverse sinus is found behind the arterious reflection
on the main arteries (pulmonary trunk and aorta) and in front of the venous reflection (superior vena cava and
right + left pulmonary veins). The transverse sinus is an open sinus (if you put your finger or forceps into it,
you will see both ends of the forceps. Put them behind the aorta and pulmonary trunk in front of the
superior vena cava and left pulmonary veins).
64
There is another sinus, called the oblique sinus of the pericardium, located at the venous reflection only.
If you lift the apex of the heart, you will see the posterior wall of the pericardium, and you can put your
forceps behind and below the heart, between the parietal and visceral pericardium to the venous reflection.
If you move the apex to the right, you will see the oblique sinus. The oblique sinus is a blind recess with a
dead end at the inferior part of Sappy's T.
SURFACES OF THE HEART:
The heart has an anterior or sternocostal surface (related to the ribs and the sternum). It has a diaphragmatic surface (related to the centrum tendineum of the diaphragm). It has a left or pulmonary surface
(related to the left lung). It has a posterior surface which is related to the posterior medastinum and to the
esophagus (inside the posterior mediastinum).
The anterior or sternocostal surface is composed of the right atrium and right ventricle, and
a small part of the left ventricle.
The left or pulmonary surface is formed by the left ventricle.
The diaphragmatic surface is formed mainly by the right ventricle and partly by the left.
The posterior surface is formed by the left atrium.
To best present the heart in the lab, you should hold the diaphragmatic surface because it is the most flat.
The apex should be on the left side, the base on the right side, and the pulmonary trunk in front.
The X-ray of the heart has two arches on the right side and four arches on the left side. The superior
arch on the right side is formed by the superior vena cava and the ascending aorta. The inferior arch on the
right side is formed by the right atrium. On the left side, the arches are formed by 1 aortic arch, 2 pulmonary
trunk, 3 left auricle, and 4 left ventricle. The inferior border of the heart is not visible because below, we
have the liver, and the density of the heart and liver is the same.
In the same X-ray, you can find the lung and the lymph nodes (if enlarged) in the hilus of the lung (and
also the arteries going into the lungs).
CAVITIES:
The right atrium is located on the right side (right border of the heart), forming the anterior surface of the
heart. It has two main parts: the auricle and the atrium proper. They are separated from each other by the
sulcus terminalis (outside) and by the crista terminalis (inside). The crista terminalis develops from the
septum spurium (see embryology). The difference between the auricle and the atrium proper is the presence
of pectinate muscles inside the auricle. The atrium proper, has none (the inner surface is smooth). The main
part of the atrium proper is the sinus venarum cavarum (receives the superior and inferior venae cavae).
The smooth part develops from the sinus venosus, and the other part develops from the atrium commune
(embryology).
At the orifice of the inferior vena cava, there is a valve which is called the Eustachian valve. This valve
guided the blood from the inferior vena cava through the oval foramen to the left atrium in fetal life. In the
adult, the valve has no function. The superior vena cava doesn't have a valve.
There is another ostium into the right atrium, the ostium of the coronary sinus. It is located between the
fossa ovalis and the orifice of the inferior vena cava. This sinus also has a valve which is called the
thebesian valve or ostium sinus coronari. The coronary sinus is the main vein of the heart taking blood
directly into the right atrium. The superior vena cava takes the blood from the head, neck, and upper limb.
The inferior takes the blood from the lower limb, abdominal wall, and paired organs of the abdominal cavity.
Inside the right atrium, we have the pacemaker of the heart, called the sinoatrial node or the sinus node.
This node is located in the upper end of the terminal sulcus at the inlet of the superior vena cava (in the wall
of the right atrium).
In the right atrium, on the interatrial wall separating the two atria, lies the oval fossa, a depression of the
septum covered by a valve called the valva fossae ovalis. This fossa was opened in the fetal life, at that time
called the foramen ovale. The valve fuses with the limb of the foramen ovale after birth, so the foramen is
closed. Sometimes, this fossa remains open, and this symptom is called foramen ovale apertum. The fossa
ovalis is surrounded by a border which is called limbus fossae ovalis. The function of the foramen ovale in
65
the fetal life was the circulation of blood through the foramen into the left atrium before the lungs breathed
air.
The right ventricle is located mainly on the anterior and also on the diaphragmatic surface of the heart.
Inside the right ventricle, the papillary muscles form the inner muscle of the heart. Generally, the ventricles
have three muscular layers and the atria have two muscular layers; therefore, the ventricles are thicker than
the atria. These papillary muscles form the inner layer of the ventricle together with the bridges and ridges
or the trabeculae carneae (Rathke's bundles). The function of the papillary muscles is to connect the
cuspid valves to the muscular wall. These connections are made by the chordae tendineae (tendinous cords)
between the cusps and the papillary muscles. In the right ventricle, the largest papillary muscle has a
muscular cord from the interventricular septum. This cord is called TRABECULA SEPTOMARGINALIS. The
anterior papillary muscle connects the anterior cusp of the tricuspid valve. Between the right ventricle and
right atrium, we have the tricuspid valve, having three cusps (anterior, septal, and posterior).
The anterior cusp is connected to the anterior papillary muscle through the tendinous cords. Septal and
posterior papillary muscles connect the other cusps, but the anterior is the largest. These papillary muscles
contract the same way as the muscles of the ventricles during the systolic phase. So, during the systolic
phase, the length of the ventricle will be shorter because of the contraction. The same happens with the
papillary muscles. If the papillary muscles wouldn't contract the same way, the chordae tendineae would
become loose and the valve would be reflected into the atrium, allowing blood to flow back to the atrium.
This way, the papillary muscles are responsible for the closure of the valve during the systolic phase and for
preventing the back-flow of blood into the atrium.
The ventricle has two main parts: 1) Inflowing part. The venous blood flows from the right atrium to
the right ventricle. 2) Outflowing part. Blood flows out from the ventricle through the ostium trunci
pulmonalis. So, the ventricle is V-shaped, the first part lying behind the second part.
If you put a forceps in the right venous ostium and another forceps into the left arterial ostium, you will
see the V shape. The outflowing part forms a cone on the outer surface which is called the conus arteriosus.
From this conus, the pulmonary trunk starts. The outlet of the pulmonary trunk from this conus is called the
infundibulum (where it starts from the ventricle).
In the right ventricle, the crista supraventricularis separates the inflowing and outflowing parts of the
ventricles from each other. So, it is just a protrusion on the interventricular septum.
The left ventricle forms the left surface (or the pulmonary surface) and the diaphragmatic surface of the
heart. It is separated from the right ventricle by the anterior interventricular groove (or sulcus) having a
branch of the left coronary artery inside. It has the bicuspid valve inside between the left atrium and left
ventricle. The valve has two cusps (anterior and posterior) which are connected to the muscular wall by the
anterior and posterior papillary muscles. This ventricle also has the trabeculae carneae forming the inner
muscular layer of the ventricle. The wall of the left ventricle is much thicker than the wall of the right
(about 1-1.5 cm), and the interventricular septum is also formed by this thick wall of the ventricle. So, in
cross section, the left ventricle is round. From the left ventricle, we have the ostium aortae (the origin of the
aorta). The ostium is covered by the semilunar valve which has three valvules; two in front and one behind.
In the pulmonary trunk, there is one in front and two behind.
The above is the ex-situ terminology (nomenclature), and the in-situ terminology is how you can find it in
the body (the opposite). In-situ terminology isn't so important for the dissecting laboratory.
The left atrium contains the ostia of the pulmonary veins. Two veins from the left side and two from
the right side open into this atrium. It is located on the posterior surface (or mediastinal) of the heart, and
this atrium has a close relation with the esophagus. This fact has a very important clinical note: there is an
instrument called the esophagoscope (or gastroscope). If you put it into the esophagus and accidently pierce
the wall of the esophagus, there is risk of injury to the left atrium of the heart.
The atrium has two parts: the AURICLE and the ATRIUM PROPER. The auricle has the pectinate muscles.
The smooth part is the atrium proper. The atrium proper receives the pulmonary veins. The auricle is the
only part of the left atrium which is visible at the left margin of the heart. The two auricles form an arrow
toward the aorta and the pulmonary trunk.
66
VALVES:
There are cuspid and semilunar valves. The cuspid valves are located between the atria and the
ventricles, covering the atrioventricular orifices (see above).
The cuspid valves are composed of two or three cusps that have mesothelium on both surfaces (superior
and inferior). Between the mesothelium layers, we have fibrous cutaneous tissue. These cusps are
attached to the tendinous cords that connect the cusps to the papillary muscles.
The tricuspid valve has anterior, posterior, and septal cusps. The bicuspid valve has anterior and
posterior cusps. These valves arise from the annulus fibrosus, the skeleton of the heart. The right
atrioventricular ostium has the tricuspid valve, and the left atrioventricular ostium has the bicuspid valve.
The semilunar valves (aortic and pulmonary valves) have three lunules (position previously mentioned).
Between the lunulae, we have nodules. So, the function of the nodules is th close the orifice (the central
part - triangular in shape). There are 6 lunulae and 3 nodules in one valve. The valve itself has a dense
part (pars densa) and a flexid part (pars flexida). The dense part is the peripheral part (arising from the
fibrous ring), and the flexid part is the central part (loose).
Above the valve of the aorta, there is a dilated part on the aorta which is called the aortic sinus. This
dilated part from outside is a bulb. This aortic sinus, has the orifice of the coronary arteries (right and left).
If you can't easily identify which is the aortic ostium and which is the pulmonary ostium (for example, on
a fresh heart), you should know that where we can find the orifice of the chorda above the valve, that's the
aortic ostium.
The semilunar valves are closed in the diastolic phase and open in the systolic phase. In the systolic
phase, the blood goes out from the ventricles through the aorta and pulmonary trunk. In the diastolic phase,
the heart will be filled by blood through the atrioventricular ostia.
FIBROUS RINGS:
These form the skeleton of the heart. The muscles of the atria and ventricles arise from this fibrous ring,
and it has the ostia (orifices). Between these rings, there are triangular shaped areas. There is a triangle
between the left and right venous ostia and the aorta called the trigonum fibrosum dextrum. The left one is
between the aorta and the left venous ostium. The right fibrous triangle is the most important because
through this triangle, we have the His bundle (atrioventricular fascicle, belonging to the conducting system
of the heart). From the atrium, the impulse goes through the fibrous ring into the ventricle (conducting the
impulse).
CONDUCTING SYSTEM:
It starts with the pacemaker (sinoatrial node). From this node, it then reaches the atrioventricular node
which is in the interatrial septum below the fossa ovalis and left to the ostium of the coronary sinus. The
atrioventricular fascicle (His bundle) arises from the atrioventricular node, piercing through the right fibrous
triangle (entering the ventricle). Between the sinoatrial and atrioventricular nodes, we don't exactly have
macroscopically visible bundles (or fascicles) to conduct the impulse. So, the impulse reaches the AV node
through the muscle of the atrium (this differs from the physiological discussion of the conduction system!).
The His bundle divides into two parts: crus sinistrum and crus dextrum. These two crura ride on the
interventricular septum. The right crus is on the right surface of the septum. They are also called Tawara
bundles. The right crus is located inside the septomarginal trabecula.
LAYERS OF THE HEART:
We have three main layers:
A serous layer, which is called the epicardium (visceral layer is the pericardium).
A muscular layer, which is called the myocardium.
An inner layer, which is called the endocardium.
The epicardium is layered by mesothelium, and it is connected to the muscle by a fibrous connective
tissue which has fat. So, if the heart is fatty, the fat accumulates beneath the epicardium, between it and the
myocardium (and also inside the myocardium). The coronary artery and cardiac veins lie beneath this
epicardium. So, to dissect the coronary vessels, we have to remove the epicardium, the fat, and the
connective tissue.
67
The muscle of the ventricles has three layers:
The outer, oblique layer starts from the right end of the coronary sulcus on the anterior surface and
descends toward the apex from right and superior to left and inferior. On the posterior surface,
it starts from the left side to the right side. At the apex, these fibers meed each other and form a
turn which is called vortex cordis. The fibers turning inward and upward continue into the
inner muscular layer of the heart (papillary muscle and trabeculae carneae).
2)
The middle layer is circular, parallel to the coronary sulcus. This layer is missing on the apex,
where there is only the vortex cordis.
The muscle of the atrium is not so regular and is thin (just two layers). The outer is longitudinal
and the inner is circular.
There is regular muscle at the inlet of the veins (superior and inferior venae cavae) where the
muscle is circular--surrounding the inlet.
3)
The innermost layer is the endocardium which has the fibrous layer that connects the endothelium
(innermost layer) to the myocardium. So, the endocardium is composed of two layers: a fibrous
layer and an epithelial (endothelial) layer.
The valves are also layered by this endocardium, both inferior and superior surfaces, and between
these endothelial layers, there is the fibrous layer.
1)
BLOOD SUPPLY:
Arteries:
The coronary arteries arise from the sinus (ascending) aorta, which is the first dilated portion of the
aorta just above the valves. From above the anterior right aortic sinus, the right coronary artery.
From above the anterior left aortic sinus, the left coronary artery arises. The right one emerges between
the right atrium and the pulmonary trunk, and it runs in the right part of the coronary sulcus toward the
posterior surface of the heart (main right coronary artery). Going backward in the posterior part of the
sulcus coronarius, it gives a descending branch between the left and right ventricles in the sulcus
interventricularis posterior which is called the ramus interventricularis posterior of the right coronary
artery. This artery supplies the right ventricle, except a 1 cm stripe along side the descending branch of
the left coronary artery. The right coronary artery also supplies the right atrium, and it gives a branch
for the sinoatrial node. It supplies also the posterior part of the interventricular septum (by the
descending branch) by the posterior septal artery.
The left coronary artery arises from the left anterior aortic sinus, between the left auricle and the
pulmonary trunk. So, the first part (approximately 1-1.5 cm) is covered by the pulmonary trunk. After
that, it divides into two branches: the anterior interventricular branch, and the circumflex branch (runs
left inside the left part of the coronary sulcus backward).
From the circumflex branch, there are marginal branches located at the left border of the heart. The
circumflex branch anastomoses with the main right coronary artery behind. This artery supplies the left
ventricle and the 1 cm stripe of the right ventricle along side the descending branch. It also supplies the
left atrium and the anterior part of the interventricular septum (anterior septal artery).
Veins:
They run together with the arteries, and you have to know which vein belongs with which artery.
So, the right coronary artery runs together with the vena cordis parva (SMALL CARDIAC VEIN). This
vein enters the main vein, the coronary sinus, from the right side. This way, it flows into the coronary
sinus at the right end of it.
The vena cordis magna (GREAT CARDIAC VEIN) runs together with the anterior interventricular branch
of the left coronary artery. After that, together with the circumflex branch of the left coronary artery,
and it enters the coronary sinus from the left side. So, the coronary sinus receives both parva and magna
from left and right, and it also receives the vena cordis media (middle cardiac vein) from the posterior
surface of the heart, running together with the posterior interventricular branch of the right coronary
artery. At the point where the vena cordis media joins the vena cordis parva, we have the right end of
the coronary sinus. So, the confluence of these two veins gives the right end of the coronary sinus.
The confluence of the vena cordis magna with a tiny vein from the left atrium (oblique vein of the left
68
atrium or Marssal vein) gives the left end of the coronary sinus. Between the right and left ends, the
coronary sinus opens into the right atrium of the heart.
In addition to these three veins, there are also tiny veins on the right ventricle (anterior surface) called
venae cordis anterioris. They cross the coronary sulcus to enter the right atrium directly. There are
also the tiny veins called venae cordis minimae (thebesian veins) from the atria which also directly drain
to the atria.
NERVE SUPPLY:
The heart is supplied by both sympathetic and parasympathetic fibers. These fibers reach the heart in
three plexuses called superior, middle, and inferior cardiac plexuses.
The sympathetic fibers of the superior plexus arise from the cervical ganglia of the sympathetic trunk.
The sympathetic fibers of the middle plexus arise from the stellate ganglion (fusion of the last cervical with
the first thoracic). The sympathetic fibers of the inferior plexus are from the thoracic sympathetic ganglia.
The parasympathetic fibers arise from the vagus nerve, which also carries the sensory fibers.
The sympathetic innervation increases the heart frequency, and the parasympathetic innervation decreases
it. So, if you cut both the sympathetic and parasympathetic fibers, the heart will beat in only one frequency
(standard) dependent on the sinoatrial node. Anxiety, stress, or physical labor will not change.
Between the layers of the supracardiac mediastinum, the phrenic and vagus nerves enter the thoracic
cavity, coming from the neck. The two nerves enter the thoracic cavity between the layer of main veins and
the layer of main arteries (behind the veins, in front of the arteries).
The vagus nerve is a little more medial than the phrenic nerve. The right vagus nerve enters the thoracic
cavity between the right subclavian vein and artery. It gives a branch here that turns back behind the right
subclavian artery, called the recurrent laryngeal nerve. The recurrent laryngeal nerve turns back behind the
aortic arch. On the left side, the vagus nerve is between the aortic arch and the left subclavian vein. This
happens because the 4th branchial arch has the arteries (aortic arch - left side; subclavian artery - right side).
The nerve of the 4th arch is the vagus, so the artery determines the position of the nerve. Then, the vagus
nerve runs into the posterior mediastinum behind the root of the lung.
The phrenic nerve is a little more lateral and enters the thoracic cavity between the subclavian vein and
artery (on both sides). It remains on the anterior mediastinum in front of the root of the lungs between the
pericardium and the mediastinal pleura. The phrenic nerve is accompanied by an artery called
pericardiacophrenic artery (branch of the internal thoracic) which supplies the pericardium and the upper
surface of the diaphragm. The phrenic nerve arises from the 4th cervical segment (cervical plexus) and
descends to the diaphragm carrying motor and sensory fibers. The sensory fibers innervate the pleura
carrying the diaphragm.
69
ABDOMEN
MEDIAN ABDOMINAL REGION
The skin of the abdominal region is innervated by the cutaneous end branches of the lower six intercostal
nerves, the ilioinguinal nerve, and the iliohypogastric nerve.
Beneath the skin, the superficial epigastric artery and vein run toward the umbilicus. There is another
pair at the level of the inguinal ligament toward the iliac crest called the superficial circumflex iliac artery
and vein. Both pairs come from the femoral artery and vein. The third superficial branch of the femoral
artery isn't on the abdominal wall, but runs to the external genitals and is called the external pudendal artery.
All three branches come out through the fascia of the thigh at the hiatus saphenus.
The superficial abdominal fascia lies below these superficial structures
Removing this fascia exposes
the anterior wall of the rectus sheath. The rectus sheath is formed by the aponeuroses of three different
abdominal muscles: 1 External oblique, 2 Internal oblique, 3 Transverse abdominis. The aponeurosis of the
external oblique and the anterior half of the aponeurosis of the internal oblique form the anterior wall of the
rectus sheath (or lamina anterior). The posterior half of the aponeurosis of the internal oblique and the
aponeurosis of the transverse abdominis form the posterior wall of the rectus sheath. Between the two walls
lies the rectus abdominis muscle.
The posterior wall of the rectus sheath has two arteries: 1 Inferior epigastric artery (from external iliac), 2
Superior epigasatric artery (from internal thoracic). They anastomose with each other.
The linea arcuata is an arch-shaped line (convex upward) that is located three fingers below the
umbilicus (on the posterior wall of the rectus sheath). Below this line, both anterior and posterior walls of
the rectus sheath pass in front of the rectus abdominis which is lined posteriorly only by the fascia
transversalis and the peritoneum parietale. The peritoneum is a serous membrane that is formed by simple
squamous epithelium (mesothelium).
The rectus abdominis muscle is separated by tendinous intersections into small parts. These parts act as
separate muscles rather than as a large one.
The internal oblique muscle originates where the external oblique is inserted (also in the thoracolumbar
fascia). The fibers of the two muscles cross each other. External oblique: fibers come from superolateral
to inferomedial. Internal oblique: fibers come from inferolateral to superomedial.
The linea alba is a line formed by the crossing of the three aponeuroses (from the xiphoid process to the
pubic tubercle).
REGIONS OF THE ABDOMINAL WALL
Right
Hypochondriac region
(hypochondrium)
Middle
Epigastric region
(epigastrium)
Right lumbar region
Umbilical region
Left
Hypochondriac
region
(hypochondrium)
Left lumbar region
Right iliac region
Pubic or vesical region
Left iliac region
70
The pubic region is so named because of the pubic bone (pubic symphysis) or because of the urinary
bladder (vesica urinaria).
There are two more regions seen posteriorly called renal regions between the 12 th ribs and the iliac crests,
called so because of the kidneys ("ren" in latin).
ORGANS
Right Hypochondriac:
Liver (highest level: 5th rib. Lowest level: right costal arch or a little above). If the inferior
border of the liver is below the level of the right costal arch, it means that the liver is enlarged.
The left lobe of the liver, through the epigastric region, terminates to the left hypochondriac
region. During inspiration, the liver descends because of the descending diaphragm.
Gall Bladder (located in the H-fissure of the liver). To palpate the gall bladder, find it in the
crossing of the medioclavicular line and the right costal arch. If the gall bladder is normal, you
will not palpate it, but if it is painful, it means that there is an inflammation. By this way also,
you can palpate a stone inside the GI.
Right Colic Flexure [or hepatic] (between the ascending and transverse parts of the large
intestine).
Epigastric region:
Stomach. It starts at the cardia which is located at the level of the 11th thoracic vertebra, left side.
The cardia is related to the ribs, found at the level of the 7th rib, 2cm left of the midline. It is the
most fixed part of the stomach.
The pylorus is the second most fixed point of the stomach and is located at the right side of
the first lumbar vertebrae.
Between the cardia and pylorus are the greater and lesser curvatures. The lesser curvature
is right, and the greater is left. The fundus of the stomach starts at the level of the cardia and is
elevated upward into concavity of the diaphragm in the left hypochondriac region (related there to
the spleen). The shape of the stomach is a letter "J" in standing position or "posthorn" shape in
lying position. Normally (in standing position), the pylorus and the greater curvature are above
the umbilicus, but when the stomach is full of food, they could be at the level of the umbilicus (or
even below). So, the greater curvature is mobile (not fixed).
Left lobe of the liver.
Pancreas (behind the stomach) is a retroperitoneal organ. It is located at the curvature of the
duodenum, having a head (right side), an body running in front of the 2nd LV, and a tail which is at
the hilus of the spleen.
Duodenum. The duodenum has four parts: superior horizontal, descending, inferior horizontal,
and ascending. The superior horizontal is located at the level of the 1 st lumbar vertebra. The
descending part at the level of 1st-3rd lumbar vertebrae. The inferior horizontal part at the level of
the 3rd lumbar vertebra. The first thee parts of the duodenum are on the right side. The
ascending part is located at the level of the 3rd-2nd lumbar vertebra, left side also.
The last three parts of the duodenum and the pancreas are retroperitoneal, located behind
the lesser sac. The superior duodenum is intra peritoneal, together with the stomach, and there is
a ligament between them called the hepatogastric ligament. The ligament between the
duodenum and the liver is called hepatoduodenal. The two together form the lesser omentum.
The plane that passes through the pylorus is the transpyloric plane. This plane is between the
insisuta jugularis and the symphysis. Their middle point is the transpyloric plane. The pylorus
is located at the right side of the 1st lumbar vertebra.
71
Left Hypochondriac region:
Spleen (between the 9th-11th ribs). If it can be palpated below the left costal arch, it means that it
is enlarged.
Fundus of the stomach.
Left colic flexure (flexure between the transverse and the descending colon), or the splenic
flexure, because it is related to the spleen (flexura lienalis sinister).
Umbilical region:
Small intestine.
Transverse colon.
Right Lumbar region:
Ascending colon.
Left Lumbar region:
Descending colon.
Renal region:
Kidneys (retroperitoneal).
Right Iliac fossa:
Cecum.
Appendix.
Terminal part of the ileum, with the iliocolic junction (terminal ileum joins the cecum).
Left Iliac fossa:
Sigmoid colon.
Pubic region:
Urinary bladder. In female, behind the urinary bladder, we can find the uterus, and behind the
uterus, the rectum. These are the three organs of the lesser pelvis.
Topography:
LIVER : Superior level - 5 rib. Inferior level - right costal arch.
SPLEEN: Between 9th -11th ribs.
CARDIA: Left side of the 11th thoracic vert. (7th rib, 2-3 cm left of the midline).
PYLORUS: Right side of the 1st lumbar vertebra.
DUODENUM: L1 - L3.
PANCREAS: L1 - L2.
RADIX MESENTERII: (Root of the mesenterium). It is an oblique line down to the right iliac fossa.
It is oblique because of the 270° turn of the umbilical loop of the midgut. It starts from the duodenojejunal
flexure from superior and left to inferior and right, and it terminates to the right iliac fossa (iliocecal
junction). You can find the radix mesentery by putting the small intestine out to the right
and upper part of the abdominal cavity.
Retroperitoneal: behind the parietal peritoneum, on the posterior abdominal wall.
Intraperitoneal: surrounded by peritoneum (inside the peritoneum).
Infraperitoneal: below the reflection of the peritoneum.
•Stomach: intraperitoneal
•Small intestine: intraperitoneal
•Jejunum and ileum: intraperitoneal
•Duodenum (superior horizontal): intraperitoneal
•Duodenum (remaining portions): retroperitoneal
•Cecum and ascending colon: intra-retroperitoneal
•Transverse colon: intraperitoneal
•Descending colon: intra-retroperitoneal
•Rectum (upper 1/3): intraperitoneal
•Rectum (middle 1/3): retroperitoneal
72
•Rectum (lower 1/3): infraperitoneal
•Pancreas and kidneys: retroperitoneal
•Liver: intraperitoneal (except the bare area)
•Spleen: intraperitoneal
Urinary bladder: infraperitoneal
Uterus: intraperitoneal
INGUINAL REGION
Superior: a horizontal line from the anterior superior iliac spine to the midline
Medial: linea alba
Inferolateral: inguinal ligament
The most significant feature here is the Inguinal Canal
Anterior wall: external oblique muscle,
Superior wall: internal oblique and transverse abdominis muscles,
Posterior wall: fascia transversalis and peritoneum parietale,
Inferior wall: inguinal ligament.
This is an oblique canal, from the abdominal cavity to the subcutaneous region (lateral to the pubic tubercle).
OUTLET: annulus inguinalis superficialis (2-3 cm lateral to the pubic tubercle).
INLET: annulus inguinalis profundus (lateral inguinal fossa).
It pierces through the abdominal wall.
There are a number of folds on the anterior abdominal wall: the median, medial (or intermediate), and
lateral umbilical folds. All of them run toward the umbilicus. The lateral folds are raised by the inferior
epigastric arteries (from the external iliac arteries). The medial (or intermediate) folds are made by the
obliterated umbilical arteries or the umbilical ligaments (the first part of the fold is made by the artery and
the end part by the ligament [the umbilical artery has a function only in the fetal life, draining blood from the
fetus to the placenta. It arises from the internal iliac artery]). The median fold lies over the median
umbilical ligament, a remnant of the urachus (reduced portion of the allantois between the apex of the
bladder and the umbilicus).
The medial inguinal fossa is between the medial and lateral umbilical folds. The lateral inguinal fossa is
lateral to the lateral umbilical fold. They are called medial and lateral inguinal fossae because of their
relation to the inguinal canal. The inlet of the inguinal canal is located in the lateral inguinal fossa. The
inguinal canal is an oblique canal. It runs from superior-posterior-lateral to inferior-anterior-medial. The
inlet of the canal is not a true opening; it is covered by the peritoneum. Therefore, the structures of the
inguinal canal are retroperitoneal (behind the peritoneum).
The medial inguinal fossa is at the level of the superficial inguinal ring. So, if you pierce directly
through the superficial inguinal ring, you will arrive in the medial inguinal fossa.
INDIRECT HERNIA: Herniation through the lateral inguinal fossa and the annulus inguinalis
superficialis.
DIRECT HERNIA: Herniation through the medial inguinal fossa and the superficial inguinal ring.
Usually, the small intestine is inside the hernial canal. In this way, the small intestine is a long way
from the spermatic cord (into the canal) and sometimes into the scrotum. To decide if the
hernia is direct or indirect, put your finger to the hernial canal, and you will feel the pulse of the inferior
epigastric artery medial or lateral to the finger. If lateral, it is a direct hernia. If medial, it
is indirect.
The outlet of the inguinal canal is bordered by two crura: medial and lateral crura (thickened collagenous
fibers of an aponeurosis).
73
The PYRAMIDAL MUSCLE: sometimes the fibers of the rectus abdominis are inserted to the pubic tubercle,
and they form the pyramidal muscle. Usually, it is not present because they are together with the rectus
abdominis.
Contents of the INGUINAL CANAL:
Spermatic cord (M) or round ligament of uterus (F).
Ilioinguinal nerve (from the lumbar plexus).
LUMBAR PLEXUS:
It is a network formed by the ventral rami of the spinal nerves T 12 -L4. Branches:
Ilioinguinal nerve,
Genitofemoral nerve,
FEMORAL nerve,
Obturator nerve,
Lateral femoral cutaneous nerve,
Iliohypogastric nerve.
SPERMATIC CORD:
Spermatic duct (or ductus deferens). The ductus deferens gives sperm to the testes.
Testicular artery.
Pampiniform plexus (venous plexus) which forms the testicular vein.
Genital branch of the genitofemoral nerve.
Arteria ductus deferentis.
Cremaster muscle.
Instead of the spermatic cord, females have the teres uteri ligament (round ligament of the uterus) and
the ilioinguinal nerve.
The testes develop in the abdominal cavity and descend down through the inguinal canal to the scrotum.
LIGAMENTS
The diaphragm is above in front of the liver, because it arises anteriorly (from the anterior abdominal
wall) and also posteriorly (from lumbar vertebrae and ribs). It is inserted into a tendinous centrum which
has the heart on it. It is cone-shaped (IMPORTANT). The diaphragm is layered by the parietal
peritoneum which reflects on to the liver, forming the posterior layer of the coronary ligaments (left and
right).
There is another reflection of the parietal peritoneum onto the liver, forming the falciform ligament. So,
the falciform ligament is a double layer of peritoneum in the sagittal plane (almost). The left layer of the
falciform ligament continues into the anterior layer of the left coronary ligament, and the right layer of the
falciform ligament continues in the right coronary ligament. The posterior layer of the coronary ligament
comes from the parietal peritoneum from the diaphragm above. This way, the two layers are next to each
other, forming a double layer at the left coronary ligament. The right ligament remains as separate layers.
The peritoneum reflecting to the liver covers both surfaces of the liver, and the two layers meet each
other again at the porta hepatis along side the fissura ligamenti venosi. This double layer descends in the
stomach and duodenum forming the hepatogastric and hepatoduodenal ligaments that are together called the
lesser omentum. The hepatogastric ligament, reaching the lesser curvature of the stomach, divides into two
layers that cover the stomach and meet each other again at the greater curvature. The new double layer
descends into the lesser pelvis and turns back, forming four layers which is the greater omentum. These
four layers go up until the transverse colon. Here, the third layer of the four runs back to the posterior
abdominal wall and continues with the parietal peritoneum covering the pancreas (posterior wall of the
lesser sac). The fourth layer also turns back to the posterior abdominal wall, but it comes forward again,
74
forming the visceral layer of the transverse colon, then turns back again. These four layers then form the
transverse mesocolon. Then, it comes forward again to form the mesenterium (layering the small intestine).
After this, it reflects onto the posterior abdominal wall.
BURSA OMENTALIS (lesser sac):
Superior wall: liver and superior recess of the lesser sac,
Anterior wall has three parts: 1 lesser omentum, 2 stomach, 3 gastrocolic ligament.
Posterior wall: parietal peritoneum (covering the pancreas)
Splenic recess: the left recess of the lesser sac (at the hilus of the spleen between the gastrolienal and
phrenicolienal ligaments.
The inlet of the lesser sac is the foramen epiploicum or Winslow's foramen. This foramen is located
on the right side of the hepatoduodenal ligament, behind the ligament, and is surrounded by the
hepatoduodenal ligament (front), the liver (above), the hepatorenal ligament (behind), and the duodenorenal
ligament (below).
DEVELOPMENT OF THE
LESSER SAC
The lesser sac is a small sac inside the "greater sac" (abdominal cavity).
At the beginning of the development, the stomach was in the median sagittal plane (future lesser
curvature in front, future greater curvature behind). Anteriorly, the VENTRAL MESOGASTRIUM is the double
layer of peritoneum that connects the stomach to the anterior abdominal wall (reflections between parietal
and visceral peritoneum). Posteriorly, the DORSAL MESOGASTRIUM connects the stomach to the posterior
abdominal wall.
In front of the stomach, inside the ventral mesogastrium, the LIVER develops (in the middle of the ventral
mesogastrium). It divides the ventral mesogastrium into two parts: the falciform ligament connects the
liver to the anterior abdominal wall, while the hepatogastric ligament connects the stomach to the liver.
The SPLEEN develops posterior to the stomach, inside the dorsal mesogastrium. It separates the dorsal
mesogastrium into two ligaments: gastrolienal (between the spleen and the stomach) and phrenicolienal
(between the spleen and the posterior abdominal wall).
Then, the stomach, together with the duodenum (below), turns to the right by 90° ("clockwise" when
viewed from superior to inferior). The spleen, which was between the liver and the stomach, moves to the
frontal plane (from the sagittal). Behind the lesser omentum and the stomach, a recess forms (lesser
peritoneal sac). Its inlet is on the right side of the omentum minus (lesser omentum), and is called foramen
epiploicum (Winslow's foramen). BORDERS: Hepatoduodenal ligament (anterior), Liver (lobus caudatussuperior), Hepatorenal ligament (posterior), and the Duodenorenal ligament (inferior).
To the right of the hepatoduodenal ligament and behind it, we have the inlet of the lesser sac. On the
left, there is no opening because the spleen is there together with the two ligaments (phrenicolienal and
gastrolienal). This way, there is a recess called the recessus lienalis or splenic recess, at the hilus of the
spleen between the two ligaments. The gastrolienal is in the frontal plane, but the phrenicolienal is a little
oblique. Thus, they form a triangular-shaped angle called the splenic recess.
THE LESSER SAC IS DEVELOPED BY THE 90° RIGHT TURN OF THE STOMACH, DUODENUM, AND LESSER
OMENTUM.
McBurney's point: The surface projection of the appendix. Appendicitis (infection of the appendix) is
a frequent condition. In this case, press the area of the appendix to find sensitivity. If it is painful,
it is almost sure to be appendicitis (together with the other symptoms, ex. fever, vomiting, leukocytosis).
The McBurney point is between the lateral and middle third of the line connecting the spina iliaca anterior
superior and the umbilicus (right side).
75
Douglas cavity (or excavatio recto-uterina):
The parietal peritoneum on the anterior abdominal wall reflects onto the urinary bladder (covering only
the anterior surface of it), and then reflect onto the anterior wall of the uterus and covers the
whole uterus. This reflection is exactly on the posterior fornix of the vagina. Then, the peritoneum covers
the rectum (1/3) and reflects onto the posterior abdominal cavity. The Douglas cavity is the lower point of
the abdominal cavity. The medical importance of this cavity is that if there is an infection or bleeding in the
peritoneal cavity, fluid is collected in the Douglas cavity (the lowest point in the abdomen). We can drain
this blood (or serous fluid) from the cavity through the vagina: you have to pierce the wall on the posterior
fornix of the vagina and the peritoneum. When blood is inside this cavity, the most frequent problem is the
extrauterine gravidity (rupture of the Fallopian tube).
RECESSES
A recess is a sac-like cavity made by a peritoneal fold (deeper portion of the peritoneal cavity).
There are three main groups of recesses: around the duodenojejunal flexure, ileocecal junction,
mesosigmoideum. These recesses are the "real recesses" and are formed by peritoneal folds. In addition,
there are the subphrenic recesses and the subhepatic recesses.
The medical importance of the first group of recesses is that the small intestine on the greater omentum
can be obstructed there. The small intestine enters these recesses and the passage of it stops there (Ileum
syndrome). The medical importance of the second groups is that an abscess can appear there.
Superior and inferior duodenal recesses, paraduodenal recess, and retroduodenal recess. The superior
duodenal recess is at the superior end of the ascending duodenum. The inferior duodenal recess is between
the inferior (horizontal) and ascending duodenum. The retroduodenal recess is behind the inferior
duodenum, and the paraduodenal recess surrounds the ascending duodenum. These recesses are bordered
by folds made by the inferior mesenteric vein and the left colic artery.
At the ileocecal junction, there is a recess between the mesentery of the terminal ileum and the root of the
appendix. There is another recess behind the cecum (retrocecal recess). Sometimes, there is an inferior
ileocecal recess below the terminal ileum.
The mesosigmoideal recess is at the mesosigmoideum in front of the left urethra at the division of the left
common iliac artery. Sometimes, this recess doesn't exist.
There is a space between the liver and the diaphragm. If you reach above the liver, your hand will be
between the diaphragm and the liver. The posterior border of this recess is the diaphragm. The left border
is the falciform ligament. The right border is, again, the diaphragm. So, this recess is above the liver and
below the diaphragm, and for this reason, it is called the subphrenic recess. Because it is on the right side, it
is called the right subphrenic recess.
There is another recess, left to the falciform ligament until the spleen (left side). Superior border:
diaphragm. Right: falciform ligament. Left: spleen. Anterior: diaphragm. This recess is called the left
subphrenic recess.
The third is the subhepatic recess which is below the liver. Reaching posteriorly, below the liver, you
can downward until the right kidney (posterior border). Superior: liver. Posterior and superior:
hepatorenal ligament. Right side: diaphragm. Left: epiploic foramen and lesser sac.
LIVER
The liver has two surfaces: VISCERAL and DIAPHRAGMATIC. The diaphragmatic surface (convex) is
related to the diaphragm. The falciform ligament (developing from the anterior part of the ventral
76
mesogastrium) separates the two largest lobes. In the inferior border of the falciform ligament, there is
another ligament called the teres hepatis ligament (round ligament of the liver). This is the remnant of the
left umbilical vein, and it runs onto the umbilicus. The umbilical vein, during the fetal life, takes
oxygenated blood from the placenta to the fetus.
The right layer of the falciform ligament continues upward to the right coronary ligament, and the left
layer continues to the left coronary ligament. The posterior layer of the left coronary ligament is reflected
onto (or from) the diaphragm (reflection of the parietal peritoneum layering the posterior part of the
diaphragm).
The visceral surface has four lobes. Between the left and right lobes are the quadrate lobe and the
caudate lobe. Lobus quadratus is in front and below, and the lobus caudatus is above and behind.
Between these four lobes, we have the H-fissure. The "H" has two longitudinal parts and one horizontal
part which is the PORTA HEPATIS. The right longitudinal part has the gall bladder in its inferior half and the
inferior vena cava in its superior half. The inferior part of the right longitudinal part is called the fossa
vesicae felleae; because if the gall bladder is removed, you can find a fossa in its place. In the upper part of
the right longitudinal fissure, we have the sulcus vena cava inferior, because if the inferior vena cava is
removed, there will be another sulcus.
In the left longitudinal part, there are fissures: inferiorly, it is called fissura ligamenti teretis (because of
the teres hepatis ligament) and the superior part is called fissura ligamenti venosi (because of the legamentum
venosus, which is a remnant of the ductus venosus Arantii: it takes oxygenated blood from the umbilical vein
directly into the inferior vena cava in fetal circulation).
The horizontal part is the porta hepatis which has three structures: Ductus hepatis (or common bile
duct), Proper hepatic artery (left side), Portal vein (between and behind the other two).
The right lobe has a renal impression (for the kidney). The inferior part of the right lobe is related to
the right colic flexure (called the hepatic flexure). Also, on the right lobe, above the renal impression, we
have the suprarenal impression for the suprarenal gland.
The quadrate lobe is related to the pylorus of the stomach. The gall bladder, together with a little part of
the right lobe, are related to the superior duodenum (that's why the superior duodenum is a little green when
seen in dissection).
The stomach (lesser curvature and anterior wall) is related to the left lobe, forming the gastric impression.
The fundus and the greater curvature are below the left lobe.
Inside the inferior vena cava (after cutting the wall), there are openings on its wall formed by the hepatic
veins. The hepatic veins drain into the IVC directly, so the hepatic veins can't be found outside the liver
(because the IVC is embedded into its sulcus).
The liver is fixed to the diaphragm by the "nude area", so named because it is attached to the diaphragm
by connective tissue, and therefore this area will not be covered by peritoneum when removed from the body.
The area nuda is the most important support. Additional supports are the coronary ligament (frontal plane),
falciform ligament (attaches to the anterior abdominal wall), hepatorenal ligament (attached to the kidney
and then to the posterior abdominal wall), and the teres hepatis ligament.
BLOOD SUPPLY:
Blood is supplied by the proper hepatic artery (from the common hepatic artery) which divides into the
left and right hepatic arteries. Sometimes, a branch from the left gastric artery goes to the liver.
The artery enters the liver where the portal vein leaves. Their larger, so called "lobar branches" (3-5)
accompany each other. Interlobular arteries branch off from the lobar arteries. From the interlobular
branches, there are circumlobular branches anastomosing with each other around the lobules. From the
circumlobular branches, we have the sinusoids only for the veins because the branches of the circumlobular
arteries enter the sinusoids forming the capillary system of the liver. From this point, only veins start. The
first are the central veins that are parallel to the long axis of the lobules. These veins are collected by the
sublobular veins (vertical to the long axis of the lobules), that are collected by hepatic veins which are
drained into the inferior vena cava. The inferior vena cava enters the right atrium of the heart.
There are both arteries and veins are inside the liver until the sinusoids (capillaries of the liver). The
difference of the liver from the other organs is that the veins recapillarize ("2 nd capillarization"). The first
77
capillarization is occurs in the arteries at the intestine. The 2nd capillarization (by the veins) is called the
portal system. There are other organs where the arteries have two capillarizations (first arterioles,
capillaries, and then arterioles and not veins), and these are the kidney and the pituitary gland. The portal
vein starts from behind the neck of the pancreas coming from the splenic and superior mesenteric veins.
These two veins join and form the portal vein. Into the portal vein, the inferior mesenteric and the coronary
veins drain as well. The portal vein collects the blood from the single (unpaired) organs of the abdominal
cavity. The border between the caval and the portal systems is at the cardia, because above the cardia
(from the esophagus), the superior vena cava drains the blood, while below the superior third of the rectum,
the inferior vena cava drains the blood.
ANASTOMOSES BETWEEN THE PORTAL SYSTEM AND THE INFERIOR VENA CAVA
One anastomosis has just been mentioned. It is at the cardia, where the esophageal veins are drained
in the superior vena cava. The blood from the stomach (cardia: main part of the stomach) through the right
and left gastric veins to the portal vein. If circulation is blocked in the liver, the blood will be drained by the
IVC, and these esophageal veins will be enlarged. The very thin wall of them is easily ruptured. If this
occurs, a huge bleeding and vomiting (emesis) of the blood will result. To treat this problem, place a special
tube having a balloon at its end in the esophagus when the balloon is deflated. Then, inflate the balloon,
pressing the wall of the esophagus to stop the bleeding.
Between the superior and middle rectal veins, there is another anastomosis. The superior rectal vein
drains into the portal circulation through the inferior mesenteric or the superior mesenteric (or sometimes the
splenic) vein. The middle rectal vein drains into the IVC through the internal iliac vein. For this main
reason, we can also have bleeding from the rectum.
The third anastomosis between the IVC and the portal system is around the umbilicus. From the
anterior abdominal wall (above the umbilicus), the inferior epigastric vein and the inferior vena cava drain
the blood. There are also blood vessels through the ligamenti teres hepatis into the portal vein. If the
portal circulation is obstructed, the blood will be drained only by the superior and inferior venae cavae
systems. In this case, the veins will be dilated and will become visible because they are very superficial
veins (paraumbilical veins). These will be visible around the umbilicus, and this symptom is called caput
medusae. This symptom is very rare, but the diagnosis is very easy.
The fourth anastomosis is in the retroperitoneum, around the kidneys and the pancreas. The veins of
the pancreas are drained to the portal system, and the veins of the kidneys are drained to the IVC, so they
anastomose (not very important).
78
SPLEEN
Between the 9th and 11th rib. It has three surfaces: 1 diaphragmatic surface (convex - related to the
diaphragm), 2 anterior visceral surface, 3 posterior visceral surface.
The anterior and posterior visceral surfaces meet each other at a sharp margin which is called the hilus of
the spleen. The anterior visceral surface is called the gastric surface because it is related to the stomach.
The inferior part of this surface is related to the left colic flexure. This way, we have the colic impression.
The posterior visceral surface is related to the left kidney (renal impression).
The ligaments that support the spleen are: the phrenicolienal ligament (developing from the posterior
mesogastrium), gastrolienal ligament (also from the posterior mesogastrium), phrenicocolic ligament.
Through the hilus, the splenic artery enters or exits the spleen.
The spleen has two poles: superior and inferior. The axis of the spleen between these two poles is
oblique.
It has a superior margin (a little anterior), and an inferior margin (a little posterior).
The phrenicolienal ligament has a part where it is attached to the stomach but not to the spleen, and this
part is called the phrenicogastric ligament.
The most important support of the spleen is the phrenicocolic ligament, between the diaphragm and the
left colic flexure. It is also called the nidus lienalis: nest for the spleen (it prevents the spleen from
descending).
RELATIONS:
Stomach (anterior), kidney (posterior), left colic flexure (inferior). The tail of the pancreas is related to
the hilus of the spleen.
PANCREAS
It is a retroperitoneal organ, having a head, neck, body, and tail. The head of the pancreas is located
between the first and second lumbar vertebrae in the curvature of the duodenum (right side). It is found in
the epigastric region. Between the head and the body, there is a notch which is called the insisura
pancreatis. In front of the notch, the head has a curvature which is called processus uncinatus. The head
and body form an angle (because the body is more horizontal than the head) that makes an elevation called
the tuber omentalis (in the posterior wall of the bursa omentalis). The head is on the right side, but in the
epigastric region, so it doesn't reach the medioinguinal line. The body runs in front of the first lumbar
vertebra (a little higher than the head). The tail is higher, and is found at the level of the 12th thoracic
vertebra.
The left kidney is behind the pancreas, (behind the body and tail). The tail is related to the hilus of the
spleen. The head is related to the curvature of the duodenum. The stomach lies anteriorly, but
communicates with the pancreas just through the lesser sac. As the tuber omentalis is the highest point of
the pancreas, it is related to the lesser omentum (hepatogastric ligament) and via. this ligament, to the liver,
too.
In front of the pancreas, runs the transverse mesocolon. Posteriorly, the pancreas is related to the
posterior abdominal wall, and thus to the lumbar part of the diaphragm
Blood Supply:
Inferior superior pancreaticoduodenal artery
Pancreatic arteries (from the splenic artery)
79
Relations to the blood vessels:
Celiac trunk arises right above the pancreas (neck),
Splenic artery and vein run in the superior border of the pancreas toward the spleen. The vein has its
own groove in the pancreas.
Portal vein starts behind the neck of the pancreas, by the joining of the superior mesenteric and the
splenic, so the neck is related to all three veins.
Superior mesenteric artery arises behind the pancreas, but it comes out in front from the pancreatic
notch (in front of the duodenum also).
Aorta is behind the pancreas. Both superior mesenteric artery and celiac trunk arise here. To the
right of the abdominal aorta is the inferior vena cava, so the pancreas is also related to it.
Superior and inferior pancreaticoduodenal arteries are located at the curvature of the duodenum
(between the head of the pancreas and duodenum).
Gastroduodenal artery descends in front of the head of the pancreas and has its own sulcus in the head.
LYMPHATIC DRAINAGE:
Together with the stomach. Pancreaticolienal lymph nodes drain lymph from the body and tail. The
pyloric lymph nodes drain lymph from the head.
STOMACH
It is an intraperitoneal organ which is located in the epigastric and left hypochondriac regions. The
cardia, which is the first part of the stomach, is located at the left side of the 11th thoracic vertebra and
related to the ribs (7th rib, 2cm left to the midline).
The next part is the fundus. It is located in the left hypochondrium where it is related to the spleen.
The cardia is the most fixed point of the stomach, attached to the diaphragm by the phrenicogastric ligament
and just by connective tissue.
The third portion is the corpus (or body), which has lesser and greater curvatures.
The last portion is the pylorus, having the antrum pylori and canalis pylorus. The pylorus is the second
most fixed point (relatively fixed), found to the right of the 1st lumbar vertebra ("transpyloric plane"). The
lesser and greater curvatures connect the cardia with the pylorus. The shape of the stomach is "J"-shaped in
a standing position and "posthorn"-shaped in a lying position. The greater curvature normally, in lying
position, is between the xiphoid process and the umbilicus. But, if the stomach is full of food, it could be at
the level of the umbilicus or even below. So, the greater curvature is not fixed.
The hepatogastric ligament reaches the stomach at the lesser curvature. The peritoneum surrounds the
stomach. The two layers meet each other at the greater curvature, forming the greater omentum.
BLOOD SUPPLY:
The stomach is supplied by the celiac trunk. The left gastric artery ascends first, reaches the stomach at
the cardia, then descends from the left to the right at the lesser curvature. The right gastric artery comes
from the proper hepatic and goes from the right to the left on the lesser curvature, and the two gastric arteries
anastomose.
The left gastroepiploic artery is a branch of the splenic artery, and it runs on the greater curvature from
the left to the right. This artery is found at the lower border of the gastrolienal ligament. The right
gsatroepiploic artery comes from the gastroduodenal artery and runs on the greater curvature from the right
to the left. The two gastroepiploic arteries anastomose.
There are also the short gastric arteries coming from the splenic artery and supplying the fundus of the
stomach.
VENOUS DRAINAGE:
It is given by the vena coronaria ventriculi, which drains directly into the portal vein or through the
splenic vein. There are also right and left gastroepiploic branches, draining the greater curvature and
80
entering the splenic or the superior mesenteric vein, and finally into the portal vein. But, the main vein is
the coronary vein.
LYMPHATIC DRAINAGE:
NODI LYMPHATICI GASTRICI SINISTRI (left gastric lymph nodes) are the primary lymph nodes for the fundus,
cardia, and lesser curvature. Secondary lymph nodes are located in the mediastinum and around the celiac
trunk (nodi lymphatici celiaci). From the mediastinal nodes, lymph can spread to the Virchow's lymph
node, which is located in the left supraclavicular fossa, so it is palpable if it becomes enlarges.
NODI LYMPHATICI PANCREATICO-LIENALES (pancreatico-splenic lymph nodes) are the primary lymph
nodes for the upper part of the greater curvature. Lymph filtered through these nodes drains to the celiac
nodes alongside the splenic vessels.
NODI LYMPHATICI PYLORICI (pyloric lymph nodes) are the primary lymph nodes for the pylorus and
superior duodenum. Lymphatic vessels from these nodes drain through the celiac nodes which are in
connection with the hepatic nodes. (Stomach cancer frequently gives metastasis to the liver).
NODI LYMPHATICI GASTRICI DEXTRI (right gastric lymph nodes) are the primary lymph nodes for the lower
part of the greater curvature. Lymph from these nodes drains to the cisterna chyli.
Lymphatic vessels from the celiac nodes drain the lymph to the cisterna chyli. "Chyle" is derived from
the Greek word for "juice" and refers to the milky appearance of lymphatic fluid from the intestinal lacteals.
The cisterna chyli is located in the retroperitoneum behind the abdominal aorta, at the 1 st lumbar vertebra.
It collects lymph from the lower limbs (truncus lumbalis dexter et sinister) and from the intestines (truncus
intestinalis). Ductus thoracicus drains the lymph from the cysterna chyli into the left angulus venosus.
DUODENUM
The duodenum has four parts: superior horizontal, descending, inferior horizontal, and ascending. It is
the continuation of the pylorus, so it is mainly on the right side of the first lumbar vertebra (and is therefore at
the level of L1). The descending duodenum descends in front of the hilus of the right kidney until the 3rd
lumbar vertebra (L3). The inferior horizontal part is at the level of the 3rd lumbar vertebra and runs to the
left side in front of the vertebral column. The ascending duodenum ascends to the 2 nd lumbar vertebra (left
side). This point, which is the termination of the ascending duodenum, is called the duodenojejunal flexure
(L2).
The superior duodenum is infraperitoneal, while the other three parts are retroperitoneal. At the
beginning of the development, the duodenum was intraperitoneal, but with the 90° turn of the stomach and
duodenum to the right, it became retroperitoneal (except its proximal part).
As the duodenum develops from both the foregut and the midgut, it is supplied by the celiac trunk and the
superior mesenteric artery. The superior part is supplied by the superior pancreaticoduodenal artery (from
the gastroduodenal artery) and the inferior part is supplied by the inferior pancreaticoduodenal artery (from
the superior mesenteric artery). These two arteries have anastomoses between the head of the pancreas and
the curvature of the duodenum.
RELATIONS:
The superior horizontal duodenum is the continuation of the pylorus. Behind the superior duodenum,
the ductus coledochus (common bile duct) descends to the descending duodenum, while the portal vein
ascends to the liver. The superior duodenum is also related to the gall bladder and the right lobe of the
liver.
The descending duodenum is related to the right kidney (hilus). This is important, because the
duodenum is not exactly related to the right abdominal wall, but just to the hilus of the kidney. They are not
so long (superior and inferior horizontal parts) that they reach the abdominal wall. They just go until the
kidney. The descending duodenum is crossed by the mesocolon venosum.
The inferior horizontal duodenum is crossed by the mesentery that descends to the right iliac fossa.
The blood vessels are also inside the mesenterium (jejunal and iliac branches, ileocolic artery). The inferior
81
duodenum is between the superior mesenteic artery and the abdominal aorta. There is a sharp angle
between them. If we eat too much, the duodenum could be filled by food and the superior mesenteric artery
can press the inferior duodenum against the abdominal aorta or against the posterior abdominal wall, which is
behind the (abdominal aorta). This syndrome is called superior mesenteric syndrome which causes ileus
(passage inside the intestine stops).
The duodenum is not asked in detail in the 2nd semester exam. It is a retroperitoneal organ and is
discussed in the 3rd semester. Be prepared to give its relations to other organs and the Fatter's papillae:
The ductus coledochus opens into the descending duodenum near the posterior wall. This opening has a
muscle called the sphincter oddi. This muscle can close the orifice or keep it open. If the stomach is full,
the muscle keeps the orifice open, and bile goes to the duodenum. If the stomach is empty, the opposite
happens, and bile goes to the gall bladder for concentration. If the bilirubin level is too high, it will appear
in the blood (normally, bilirubin does not appear in the blood). In the case of excess hemolysis, there may
be a hemolytic anemic disease. The patient's skin will be yellow, a symptom of icterus (too much bilirubin).
This is the first cause of icterus. The second is a stone in the ductus coledochus that stops the bile
circulation. In such cases, bile can go only to the gall bladder.
BILE:
Bilirubin is responsible for the green color of the bile. Bilirubin is the decomposition product of the bile
which is secreted from the liver. Bile also has cholesterine, different inorganic salts, and water. Bilirubin
can be found which comes from hemoglobin. Hemoglobin has two main parts: globin (protein) and heme.
The heme has iron inside, and the structure which is connected to the iron is the porphyrin frame of the heme.
The degradation product of this frame is the bilirubin.
EXTRAHEPATIC BILE CIRCULATION:
The bile is secreted by the liver. From the two main lobes of the liver, there are right and left hepatic
ducts. They join each other above the porta or at the porta hepatis. There, we have the united duct which
is called the hepatic duct. This hepatic duct joins with the cystic duct, forming the common bile duct which
is located in the hepatoduodenal ligament. It runs behind the superior duodenum and opens into the
descending duodenum on the Fatter's papillae (papillae duodeni major) together with the main duct of the
pancreas, which is called the ductus pancreaticus major (Wirsung duct). The pancreas has another
opening into the duodenum: the opening of the accessory duct of the pancreas which is a little above the
Fatter's papillae. At the Fatter's papillae, we have the oddis sphincter muscle.
Intrahepatic Circulation is done inside the liver, and it belongs to histology.
SMALL INTESTINE
It starts with the duodenum, then the jejunum, and finally the ileum. The jejunum is located in the upper
left part of the abdominal cavity. The ileum is in the lower and right parts. The border is not well visible
from outside, but usually, it is in the left iliac fossa at the level of the left iliac crest, where the ileum starts to
be vertical. The small intestine mainly occupies the umbilical region, but also the right and left lumbar
regions. It is related to the retroperitoneal organs. The greater omentum covers it. Through this
omentum, it is related to the anterior abdominal wall. The intestine is intraperitoneal, having a long
mesenterium. The mesenterium starts from the flexura duodenojejunalis and terminates in the iliocecal
junction (right iliac fossa). The blood and lymph vessels of the small intestine can be found inside the
mesenterium.
INNERVATION:
82
By both sympathetic and parasympathetic fibers. The parasympathetic innervation is given by the vagus
nerve. The sympathetic innervation is given by the celiac ganglia and superior mesenteric ganglia (the large
intestine receives sympathetic innervation from the inferior mesenteric ganglia).
GANGLIA
Superior and inferior mesenteric, celiac, aorticorenal ganglia are called prevertebral ganglia. The
paravertebral sympathetic ganglia are the superior, middle, and inferior cervical ganglia. From these
prevertebral ganglia (in front of the vertebral column), the organs receive the sympathetic innervation. The
preganglionic fibers arise from the lower six thoracic segments of the spinal cord (and the upper lumbar in
the case of the lower part of the large intestine). The vagus nerve gives parasympathetic innervation for the
large intestine until the left colic flexure. Descending and sigmoid colon and also the rectum are innervated
by the sacral part of the spinal cord (sympathetic fibers).
Stomach: vagus, celiac trunk, and superior and inferior mesenteric ganglia.
Spleen and Liver: vagus, celiac trunk.
LARGE INTESTINE
It starts in the right iliac fossa with the cecum, having the appendix on it, at the junction (meeting point)
of the three teniae. These teniae are analogous to the omental and mesocolic teniae of the transverse colon.
At the junction of the cecum with the ileum, there is a valve called the valvula iliocecalis (or Bowkin
valve). This valve prevents the turning back of the food into the ileum.
Continuation of the cecum upward is the ascending colon, located in the right lumbar region (lateral to
the medioinguinal line). It is a partly intra- and partly retroperitoneal organ. It is related to the right
kidney. It ascends to the liver, then turns to the left (the right colic flexure), and continues as the transverse
colon. The right colic flexure is related to the right lobe of the liver and for that is also called hepatic
flexure.
The transverse colon is located below the stomach, and it is connected to the posterior abdominal wall by
the mesocolon. The greater omentum is attached to the superior surface. There are two teniae here; the
third is free and is called tenia libera. The transverse mesocolon starts from the right colic flexure to the
left.
The left colic flexure is related to the spleen, so it is also called splenic flexure. The phrenicocolic
ligament connects this flexure to the diaphragm, forming the nidus lienalis.
The transverse colon is attached to the stomach by the gastrocolic ligament (first part of the greater
omentum).
The descending colon is located in the left lumbar region, and is related to the left kidney. It is usually
very thin. The relation to the peritoneum is the same as the ascending colon (partly intra-, partly retro-). It
continues into the sigmoid colon. It is surrounded by the mesosigmoideum, and so it is intraperitoneal (as is
the transverse colon). It is an S-shaped colon which is located in the left iliac fossa. The end of the
sigmoid colon is found at the inlet of the lesser pelvis, where the mesosigmoideum terminates.
83
LYMPHATIC DRAINAGE OF THE INTESTINE
Lymph circulation starts in the villi as central lymph vessels (central lacteals), which are collected by the
lymphatic plexus in the submucosal layer. From the submucosal plexus, lymph drains to the subserous
lymphatic plexus, which drain to the mesenteric lymph nodes. Lymph vessels from the mesenteric nodes
run along the branches of the superior mesenteric nodes run along the branches of the superior mesenteric
artery to the intestinal trunk, which drains into the cisterna chyli. This way, the intestinal trunk drains the
small intestine and the cecum, ascending colon, and transverse colon. Lymph from the descending colon,
sigmoid colon, and the rectum is collected by the lumbar trunks, which drain also to the cisterna chyli.
MACROSCOPICAL DIFFERENCES BETWEEN SMALL INTESTINE AND LARGE INTESTINE:
Appendices epiploicae: appendices from the large intestine which is a sac formed by peritoneum
filled by fat (only in large intestine),
Taenie coli muscle: thickened outer longitudinal layer of muscle (only in large intestine),
Haustra coli (semilunar folds): three enlarged, dilated parts of the large intestine which are called
haustre (between the three teniae).
84
RETROPERITONEUM
The retroperitoneum is the space behind the parietal peritoneum of the abdominal cavity.
The retroperitoneal organs are the kidneys, the suprarenal (adrenal) glands, the pancreas, and the main
part of the duodenum (except the superior part).
KIDNEYS
The kidneys are located at the level of the 12th thoracic and first two lumbar vertebrae. The right kidney
is a little lower than the left because the liver presses it down. The superior pole of the right kidney is
crossed from behind by the 12th rib. In the case of the left kidney, the 12th rib divides it into two parts: a
superior, smaller part (1/3), and an inferior, larger part (2/3). The kidneys are related behind to the
quadratus lumborum muscle, the psoas muscle, and the lumbar part of the diaphragm. They have anterior
and posterior surfaces. The anterior surface is a little lateral; the posterior surface is a little medial. So,
they're not exactly in the frontal plane. They have superior and inferior poles. Above the superior pole, sit
the suprarenal glands. On the medial border (it is concave), we have the hilus. The lateral border is
convex.
The kidneys are fixed to the abdominal cavity by three capsules. The most important is the outermost
capsule which is called fascia renalis. This fascia layers the anterior surface of the kidneys, continues to
the posterior layer at the lateral margin of the kidneys, and continues to the posterior layer above the kidneys.
So, it is a closed capsule superiorly and laterally, but it is open inferiorly and medially. Medially, the
anterior layer passes in front from the aorta and inferior vena cava, continues to the other side (anterior
surface) and laterally sides of the kidneys continues to the posterior layer behind the aorta and inferior vena
cava.
The anterior layer of the fascia renalis is fused with the parietal peritoneum. The posterior layer is fused
with the transverse fascia (fascia transversalis) which is the innermost layer of the abdominal wall.
Between the two layers, the middle capsule, the adipose capsule, fills the space between the two layers of the
fascia.
The innermost capsule is the fibrous capsule which is directly on the surface of the kidney. Between
the fibrous capsule and the renal fascia, there are connective tissue fibers through the adipose tissue. So,
finally, the renal fascia is connected to the fibrous capsule and the fibrous capsule to the kidneys. The renal
fascia is connected to the abdominal wall by the transverse fascia and parietal peritoneum. This is the most
important support for the kidneys.
On the medial margin of the kidney, the hilus opens into the sinus of the kidney. The sinus is a cavity
of the kidney which is surrounded by the parenchyma of the kidney (parenchyma: functional tissue of an
organ). The sinus contains the lesser calyces, the greater calyces, the branches of the renal artery and vein
(with loose connective tissue and fat), and the pelvis which continues into the ureter. The adipose capsule
continues into the sinus.
Sinus = cavity.
Hilus = entrance of this cavity.
Pelvis = one of the structures of the cavity that belongs to the urine system, collecting the calices.
The ureter starts at the level of the hilus and is the inferior posterior structure of the hilus. The anteriorposterior order of structures is vein-artery-ureter.
If you make a frontal section through the largest plane, you will see that the outermost layer is the fibrous
capsule on the surface. The next layer is called the cortex cortices (right below the fibrous capsule).
Beneath this, the cortex forms the cortical columns between the medullary pyramids. Inside the cortex,
there are striations called medullary rays (stria medullaris corticis). The cortex continues into the medulla
as cortical columns (columnae renalis or Bertin's columns). The next part of the kidney is the medulla,
forming the medullary pyramids. The apeical (papillary) openings are situated on the minor calyx. On the
surface of the apex, there are tiny openings for the papillary ducts. It is called lamina cribrosa because of
these openings.
85
The kidney develops from lobes. One original lobe was one pyramid and a half of the cortical column
(renal column). Approximately 25-30 original lobes have fused with each other and open to one minor
calyx. Minor calyces are about 8-10 in number. Three minor calyces open to one major calyx, so there are
about three major calyces that open into the renal pelvis.
PELVIS RENALIS: it is the dilated first part of the ureter which is collected from the three major calyces and
continues into the ureter. It is located in the sinus of the kidney. The other name of the pelvis is pyelos,
and the infection inside is called pyelonephritis.
Renal arteries come from the abdominal aorta, belonging to the paired visceral branches of the abdominal
aorta. It enters the kidney through the hilus and divides into interlobar branches which run in the middle of
the Bertin's columns (renal). The renal artery first divides into two main groups of arteries, one in front of
the main plane and one behind. From these main arteries, we have the additional interlobar branches. If
you cut the kidney through the largest plane, you will not cut the main arteries, because one is in front of the
plane and the other behind.
The left and right renal veins drain to the inferior vena cava. The left renal vein passes in front of the
abdominal aorta across the midline because the inferior vena cava is on the right. As a consequence of this
asymmetry, the left renal vein receives the left testicular vein or ovarian vein, but the right does not.
Usually, an additional renal artery (accessory) supplies the superior or inferior pole of the kidneys.
MUSCLES RELATED TO THE KIDNEY:
Quadratus lumborum, psoas major (hilus), and lumbar part of the diaphragm.
The muscle that fills the iliac fossa is the iliacus that inserts to the lesser trochanter of the femur. Its
function is flexion of the hip joint (it is the main flexor).
URETER
The ureter starts from the hilus of the kidney as the inferoposterior structure of the hilus and crosses the
psoas major muscle from superolateral to inferomedial. The ureter is crossed by the
1
testicular (M) or ovarian (F) artery and vein (anteriorly). The next crossing is before it enters the pelvis,
when it runs in front of the 2 common iliac artery at its division into external and internal iliac arteries. The
last crossing is in the lesser pelvis where it crosses the 3 uterine artery (F) or the ductus deferens (M).
The ureter has an abdominal (longer) part and a pelvic part. The abdominal part has the first crossing.
The second crossing is exactly at the border of the abdominal and pelvic part. The third crossing is in the
pelvic part.
The ureter pierces through the wall of the urinary bladder from lateral to medial and posterior to anterior.
So, this entrance is oblique. It forms the orifice of the ureter in the urinary bladder.
Blood supply of the ureter comes from the neighboring blood vessels: testicular, renal, and iliac arteries.
You must not lift the ureter and cut from behind because the blood supply comes from posterior and the
ureter will necrotize.
LUMBAR PLEXUS
The lumbar plexus starts from the lower half of T12, L1-L3, and the upper half of L4 segments.
The psoas major muscle arises from the bodies and transverse processes of the lumbar vertebrae. At the
level of this origin, between its fibers, the lumbar plexus starts from and it divides into branches that emerge
behind the inferior pole of the kidney: iliohypogastric and ilioinguinal. Other branches come out laterally
to the psoas major muscle: lateral femoral cutaneous nerve and femoral nerve. One branch pierces through
the psoas major muscle: genitofemoral nerve. The last branch comes out at the medial side of the psoas
major muscle and is called the obturator nerve.
86
DISSECTION:
Iliohypogastric and ilioinguinal nerves. They enter between the abdominal muscles. The iliohypogastric is between the transverse abdominis and internal oblique and innervate these two muscles. The
end branches pierce through these muscles and innervate the skin on the abdominal wall. The ilioinguinal
nerve passes between the abdominal muscles, but it joins the spermatic cord and passes through the inguinal
canal on the anterior surface of the spermatic cord, coming out through the superficial inguinal ring (outlet of
inguinal canal) and innervated the skin of the scrotum and the medial surface of the thigh that faces toward
the scrotum.
Lateral cutaneous femoral nerve runs on the quadratus lumborum muscle, toward the anterior superior
iliac spine. It comes out from the abdominal cavity 1 cm below the anterior superior iliac spine. It
innervates the lateral surface of the thigh.
Femoral nerve is located lateral to the iliopsoas muscle and leaves the abdominal cavity through the
lacuna musculonervosa together with the iliopsoas muscle.
Genitofemoral nerve pierces through the psoas major muscle and divides into two branches: genital and
femoral branches. The genital branch enters the inguinal canal and it passes inside the spermatic cord and
innervates the cremaster muscle and the layers of the scrotum. The femoral branch passes through the
lacuna vasorum of the subinguinal hiatus and innervates a small part of the skin below the inguinal ligament.
Obturator nerve is located medial to the iliopsoas muscle (the only nerve which is located medially).
It innervates the adductor muscles. It comes out from the pelvis through the obturator canal, together with
the obturator artery.
87
SUPRARENAL GLANDS
The suprarenal glands are located on the superior poles of the kidneys, being inside the renal fascia.
Suprarenal vein (the main vein) drains to the renal vein. The left suprarenal gland is triangular in shape,
but the right one is semilunar in shape. The right suprarenal gland is related to the area nuda of the liver.
The left suprarenal gland is related to the spleen.
ABDOMINAL AORTA
The abdominal aorta has parietal and visceral branches. The visceral branches are paired and unpaired.
For the 2nd semester exam, only the unpaired branches are required: 1) Celiac trunk, 2) Superior mesenteric
artery, 3) Inferior mesenteric artery.
The celiac trunk arises from the abdominal aorta, right above the pancreas (at its superior border). It
divides into three primary branches: a) splenic artery, b) common hepatic artery, c) left gastric artery. This
division of the celiac trunk is called the tripus haleris.
The COMMON HEPATIC ARTERY divides into proper hepatic and gastroduodenal arteries. The
proper hepatic artery gives right and left hepatic arteries inside the liver (but sometimes outside). The
proper hepatic artery also gives the right gastric artery which runs to the lesser curvature of the stomach
from the right to the left. So, the gastric arteries are on the lesser curvature. The proper hepatic artery
also gives the cystic artery, supplying the gall bladder. The gastroduodenal artery descends behind the
pylorus. It divides into 1 superior pancreaticoduodenal (head of pancreas - curvature of duodenum) and
2
right gastroepiploic arteries.
The LEFT GASTRIC ARTERY is a direct branch of the celiac trunk. First, it ascends to reach the
stomach at the cardia, then it descends on the lesser curvature from the left to the right. The two gastric
arteries anastomose with each other on the lesser curvature.
The SPLENIC ARTERY runs behind the stomach, in the upper margin of the pancreas, toward the
spleen, and reaches the spleen at the hilus. It gives the short gastric arteries to the fundus of the
stomach. Another branch is the left gastroepiploic artery to the greater curvature of the stomach (from
the right to the left). The right and left gastroepiploic arteries anastomose on the greater curvature,
supplying both the stomach and the epiploon (Gr.– "omentum"). Also from the splenic artery, the
pancreatic arteries run along the superior margin of the pancreas, supplying mainly its body and tail.
The head is supplied by the superior pancreaticoduodenal artery (from the gastroduodenal artery) and by
the inferior pancreaticoduodenal artery (from the superior mesenteric artery).
There is an anastomosis between the celiac trunk and the superior mesenteric artery in
the curvature of the duodenum, formed by the inferior and superior pancreaticoduodenal arteries.
Sometimes, there are anterior and posterior branches of the pancreaticoduodenal.
The short gastric arteries and the left gastroepiploic artery are located in the gastrolienal ligament.
The vein of the stomach is the coronary vein (vena coronaria ventriculi) instead of the left and right
gastric veins, because the blood drainage inside the vein is one way - from left to right. We also have the
gastroepiploic vein on the greater curvature, but the coronary vein is the most important vein of the stomach.
The superior mesenteric artery (supplying derivatives of the midgut) arises from the abdominal aorta
behind the pancreas (the origin can't be seen without moving the pancreas). The artery emerges behind the
pancreas through the pancreatic notch (between the head and neck of the pancreas).
The first branch of the superior mesenteric artery is the INFERIOR PANCREATICODUODENAL ARTERY,
the second set is the JEJUNAL ARTERIES (3-4 branches, to the left side), the third set is the ILIAC ARTERIES
(right side and below). The last branch is the ILEOCOLIC ARTERY, going to the ileocecal junction. The
88
ileocolic artery gives the appendicular artery that supplies the appendix. It is located in the
mesoappendix (in its free border) and reaches the appendix at its apex.
Also, the RIGHT COLIC ARTERY runs to the ascending colon and the middle colic artery (from the
inferior mesenteric); this anastomosis is called the arcus Riolani (in the left colic flexure).
The primary branches anastomose with each other in the margin of the mesentery. Then, the
secondary branches anastomose approximately 1-2cm from the mesenteric border. The branches from
this anastomosis are the end arteries, and they divide into three branches: 1 anterior (to the anterior wall),
2
posterior (to the posterior wall), and 3 small branch (to the mesenteric border).
The inferior mesenteric artery supplies the derivatives of the hindgut (descending colon, sigmoid colon,
and upper rectum). Its branches are the left colic artery, the sigmoid artery, and the superior rectal artery.
There is an anastomosis between the superior rectal and sigmoid arteries called the Sudech anastomosis.
MEDICAL IMPORTANCE OF SUDECH POINT: to treat a tumor in the rectum, that part of the rectum must
be removed. The external sphincter muscle can be saved (if the sphincter is not involved in the
tumor). The sigmoid colon can be moved because it is S-shaped and long enough, but blood supply
must be maintained. To do this, cut the superior rectal artery
above this point and move it down to the sphincter (because it is longer). This way, we can keep
the external sphincter and suture the sigmoid to it.
PAIRED VISCERAL BRANCHES:
The paired visceral branches of the aorta supply the paired organs: kidneys, suprarenal glands, gonads
(testes and ovaries)
Middle suprarenal arteries,
Renal arteries,
Gonadal arteries.
The suprarenal glands are supplied by superior, middle, and inferior suprarenal arteries, but the superior
comes from the inferior phrenic artery and the inferior from the renal artery.
PARIETAL BRANCHES:
Inferior phrenic artery (supplying the inner surface of the diaphragm),
Lumbar arteries (segmented- supply by posterior abdominal wall, like the intercostal arteries in the
thoracic cavity.
Middle sacral artery is the one unpaired parietal branch which arises exactly from the division of the
aorta into common iliac arteries. It descends into the lesser pelvis in front of the sacrum and supplies
the posterior wall of the lesser pelvis, together with the other parietal branches of the internal iliac
artery.
DIAPHRAGM
The diaphragm has a muscular part (arising from the sternum, ribs, and from the lumbar vertebrae) and a
tendinous part, called the centrum tendineum, which is the insertion of the muscle fibers.
The muscular part has three subportions according to the origin. It has a sternal part, a lumbar part, and
a costal part.
The lumbar part arises from the 3rd and 4th lumbar vertebrae (from their bodies, on the right side), and
from the 2nd and 3rd lumbar vertebrae (from their bodies, on the left side). This part is called the crus
lumbale mediale (medial crus of the lumbar part). The lateral crus of the lumbar part has two arches: medial
lumbocostal arch, lateral lumbocostal arch (or the medial and lateral arcuate ligaments). The medial arch
bridges the psoas major muscle, and the lateral arch bridges the quadratus lumborum muscle. From the
body of the 2nd lumbar vertebra, an additional crus arises which is called the intermediate crus (between the
medial crus and the two arches formed from the lateral). The intermediate crus separates two hiatuses
(between the medial and lateral crura). The medial lumbocostal arch arises from the body of the 2nd lumbar
89
vertebra and arches toward the transverse process of the 1st or 2nd, and lateral from there to the 12th rib.
That's why it is called lumbocostalis: because the medial goes from the lumbar vertebrae to the transverse
process and the lateral one from the transverse process to the 12th rib.
The costal part arises from the inner surface of the lower six ribs. The sternal part arises from the
xiphoid process and the body of the sternum. All these fibers insert into the centrum tendineum that has a
three foliated shape, one anterior and two posterior. On the anterior folium, the heart is located. Between
the two posterior folia, the inferior vena cava passes.
STRUCTURES PASSING THROUGH:
The two medial lumbar crura cross each other and form an arch-shaped hiatus for the aorta called the
aortic hiatus (level of T12). Together with the aorta, the thoracic duct goes through.
The medial crus fibers, after crossing, form another hiatus which is the esophageal hiatus. Together
with the esophagus, the vagus nerves enter the abdomen (left in front, right behind). This hiatus is at the
level of T10.
The aortic hiatus is posterior and a little right to the esophageal hiatus.
Between the medial and intermediate crura, there are two openings for the splanchnic nerves and the
azygos vein. On the other side, the hemiazygos vein ascends between the medial and intermediate crura.
Between the intermediate and lateral crus, the sympathetic trunk passes alone.
Coming forward, between the sternal and costal parts, the internal thoracic artery (endbranch of it is the
superior epigastric artery) passes through the diaphragm, entering the rectus sheath and anastomosing with
the inferior epigastric artery on the posterior wall of the rectus sheath.
THORAX: FINAL NOTES
On the vertebral column, you should know the erector spinae muscle (lateral to the spines of
the vertebrae) that has two main parts: longissimus and iliocostalis. Be familiar with the intercostal
muscles. Longissimus and iliocostalis muscles are surrounded by the thoracolumbar fascia (it has
two layers). It isn't necessary to know all the other tiny muscles.
90
PELVIS
BRANCHES OF THE INTERNAL ILIAC ARTERY:
The internal iliac artery comes from the common iliac artery. The division of the common iliac artery is
at the inlet of the lesser pelvis (at the level of the linea terminalis). The internal iliac artery supplies the
organs of the lesser pelvis by visceral branches and the wall of the pelvis, gluteal region, and adductor
muscles by parietal branches.
PARIETAL BRANCHES:
Iliolumbar artery. The end of this artery is located in the iliac fossa on the iliacus muscle. The first
part of the artery is visible when it arises from the internal iliac to the lateral direction.
Lateral sacral artery. This artery runs medially from the internal iliac artery toward the sacral
foramina. It gives branches ("spinal branches") through the foramina sacrale for the spinal cord and
also for the posterior wall of the lesser pelvis.
Superior gluteal artery runs through the suprapiriform hiatus, supplying the gluteus medius and
minimus.
Inferior gluteal artery runs through the infrapiriform hiatus, supplying the gluteus maximus.
Internal pudendal artery runs through the infrapiriform hiatus, turning around the spina ischiadica,
and goes back through the foramen ischiadicum minus into the ischiorectal fossa. It runs along side
the lateral wall of the fossa which is the obturator internus muscle, in the pudendal canal. This canal
is formed by the fascia obturatoria that forms a double layer, surrounding the internal pudendal artery
and pudendal nerve.
The internal pudendal artery gives branches to the rectum (inferior rectal artery), penis (dorsal or
deep penile artery), urethra (bulbourethral artery), and the perineal muscles (perineal arteries). IT
IS PARTLY A PARIETAL BRANCH, AND PARTLY A VISCERAL BRANCH.
Obturator artery runs through the obturator canal to the adductor muscles.
VISCERAL BRANCHES:
Umbilical artery runs on the anterior abdominal wall toward the umbilicus, forming the medial
umbilical fold. The last part of the artery is a ligament, because it is a remnant of the embryonic
umbilical artery (no function in adult). From the first part of the artery, which is a functioning artery,
branches go to the urinary bladder called the superior vesical arteries.
Inferior vesical artery.
Middle rectal artery.
Uterine artery, which supplies the uterus and the Fallopian tube. It also partially supplies the vagina
and ovary. It reaches the uterus at the isthmus, and before reaching the uterus, it is crossed by the
ureter (at the lateral fornix of the vagina). The uterine artery runs in the parametrium, along side of
the body of the ureter. It is a wavy artery because during pregnancy, it must become longer.
In males, the analog of the uterine artery is the arteria ductus deferens (very tiny).
91
URINARY BLADDER
The urinary bladder is located in the lesser pelvis behind and below the symphysis if empty. If full, it is
elevated and sometimes goes even up to the umbilicus. It has a capacity of 300-500 ml. The bladder has
an apex and a base. From the apex, there is a ligament called the median umbilical ligament. It is attached
to the anterior abdominal wall toward the umbilicus, forming a fold called the median umbilical fold. This
ligament is a remnant of the urachus (reduced portion of the allantois between the apex of the bladder and
the umbilicus). The bladder also has anterior and posterior surfaces. The posterior is more convex than
the anterior. The peritoneum covers only the apex and just the superior part of the posterior surface, so it is
an infraperitoneal organ (see Douglas cavity).
The anterior surface of the urinary bladder is fixed to the symphysis by a ligament called the pubovesical
ligament (F) or the puboprostatic ligament (M- reaching and fixing the prostate gland).
The bladder is related to the vesicula seminalis, the prostate gland, and the ductus deferens. The
seminal vesicle is located on the posterior surface of the urinary bladder and is fixed with the bladder by a
fascia called the retrovesical fascia. The prostate gland is below, and it is attached to the bladder. The
ductus deferens runs on the posterior surface of the bladder and has a crossing with the ureter. The ampulla
of the ductus deferens is strongly related to the bladder, medial to the vesicula seminalis.
In females, the urinary bladder is related to the uterus, which is behind and to the superior part of the
vagina.
SUPPORT:
The urinary bladder is fixed to the symphysis pubis by the pubovesical (F) or puboprostatic (M) ligament.
The most important support of the bladder is through the prostate gland (M) by the pelvic fascia. The
levator anni muscle, forming the pelvic diaphragm, has a fascia on the superior surface which is called fascia
diaphragmatis pelvis superior (or pelvic fascia), layering the levator anni muscle superior. It reflects onto
the prostate gland by two layers and surrounds the gland. As the prostate gland is attached to the urinary
bladder, the bladder is supported with the pelvic fascia through the prostate gland. In females, the pelvic
fascia reflects onto the urinary bladder, then to the vagina and uterus. It forms the most important support
for the bladder.
URETHRA
The urethra starts from the urinary bladder by the orificium urethrae internum. The ureter enters the
urinary bladder by the orificium ureteris. So, the three openings (inlet of 2 ureters and outlet of the urethra)
form a triangle (trigonum vesicae). Its mucous membrane is smooth because it develops from mesoderm,
but the other parts of the urinary bladder develop from the endoderm (see embryology).
Between the two orificium urethrae is a transverse fold which is called plica interureterica.
The ureter pierces through the wall of the urinary bladder from posterior and lateral to anterior and
medial. This oblique direction is important because the mucous membrane will form a fold inside that
covers the ostium of the ureter and prevents the backflow of the urine into the ureter. The pressure inside
the urinary bladder is higher than the ureter, so by the fold, it prevents the backflow of the urine.
MALE URETHRA
It starts from the urinary bladder. At its beginning, it has the internal sphincter muscle which is
composed of smooth muscle. Coming out through the urinary bladder, it pierces through the prostate gland
(prostatic part of the urethra). The prostatic part has a small elevation called the coliculus seminalis
("verumontanum") where the ejaculatory ducts and the main ducts of the prostate gland empty into the
urethra.
92
The uvula vesicalis is above the coliculus seminalis, and below lies a vesical fold called crista urethralis.
These two make the insertion of a catheter more difficult. Until the catheter reaches the prostate, it inserts
quite easily. Inside the urethra, there is a deep red area above the two ejaculatory ducts called the utriculus
prostaticus or male vagina because it is the remnant of the vaginal plate (developing into the vagina in
females).
Emerging from the prostate gland, the urethra pierces the urogenital diaphragm (or membrane), and this
short portion (3 mm) is called pars membranacea urethrae (membranous part). Here, we have the external
sphincter muscle of the urethra, composed of skeletal muscle.
The next portion is the spongy part, piercing the bulbus penis on the dorsal surface of the bulb and a little
in front of the end of the bulbus. So, it is dorsal and anterior to the end of the bulbus. There are two
important flexures here. The urethra emerges from the urogenital diaphragm and goes into the spongy part
of the penis to form a flexure which turns anteriorly, called the perineal flexure. Running through the
spongy penis, it has another flexure which is from the anterior direction to the inferior direction. This
flexure is below the symphysis and is called the pubic flexure. It can be straightened, in contrast with the
perineal flexure which cannot. It is important to know these flexures when inserting catheter to get the
urine. How to do it: the pubic flexure must be straightened first (so we lift the penis) and after,
approximately 10-15 cm. When reaching the perineal flexure, direct the catheter upward.
The last part of the urethra has a dilated portion which is called fossa navicularis (where the epithelium
changes). The urethra terminates in the gland penis as the orificium externum urethrae. The first change
of the epithelium is at the level of the coliculus seminalis where it changes from urothelium (transitional
epithelium) to stratified columnar epithelium. The second change is at the navicular fossa where it changes
from stratified columnar to stratified squamous non-keratinized epithelium.
In the urogenital membrane, there are glands, called bulbourethral glands, which have ducts opening into
the spongy part of the urethra, passing through the bulbus.
Prostate glands, bulbourethral glands, Littre's glands (glandulae urethrales masculinae), endoepithelial
glands, vesicula seminalis, spermatozoa: all together, they form the ejaculatory fluid through the urethra.
MALE GENITAL ORGANS
Testis
Epididymis
Ductus deferens
Vesicula seminalis
Prostate gland
Penis
TESTIS
They are located in the scrotum. They are oval glands, approximately 4-5 cm long, with medial and
lateral surfaces and superior and inferior poles. They are surrounded by the tunica albuginea. Outside the
tunica, the tunica vaginalis testis is the continuation of the peritoneum. As the testis develops in the lumbar
part of the abdominal cavity, it descends during the embryonic life, through the inguinal canal, to the
scrotum. This position is kept during development. The testes were retroperitoneal organs during
development. After descent, this position is kept.
First, a tiny process of the peritoneum develops which is called the processus vaginalis in front of the
testes. After that, they descend through the inguinal canal into the scrotum. Finally, in front of the testis
and surrounding the surfaces, is the serous membrane. So, it is a retroperitoneal organ.
The tunica vaginalis has two layers: a visceral layer which covers the testis, and a parietal layer. The
two layers reflect to each other on the posterior surface of the testis. Here at the reflection, the mediastinum
testis carries the blood vessels of the testis. When the visceral layer reflects into the parietal layer, there is a
very tiny stripe for the entrance of the blood vessels into the testis.
93
EPIDIDYMIS
On the posterior (or a little posterolateral) surface of the testis, lies the epididymis. It has a head, body,
and tail (cauda). The epididymis is approximately 4-5 cm long. It is attached to the testis by two
ligaments: superior and inferior epididymic ligaments. It is also layered by peritoneum, so it is a
retroperitoneal organ. The epididymis is connected to the testis not only by the two ligaments, but also by
the ducts inside the testis; tubuli seminiferi contorti. The convoluted tubules inside the testis continue into
the straight tubules which form a network called the RETE TESTIS. The rete testis continue into the ductuli
efferenti testis, that belong to the epididymis. The ductuli efferenti testis open into the ductus epididymidis.
The testis is connected to the scrotum by the gubernaculum testis, the remnant of a ligament. It
connects the inferior pole of the testis to the torus genitalis (a protrusion on the abdominal wall from where
the scrotum develops). So, it is a long connective tissue ligament connecting the torus genitalis with the
inferior pole of the testis through the inguinal ligament. This relatively loose connective-tissue ligament
guides the descent of the testis. So, the testis descends along side of this ligament into the scrotum.
Finally, a very short ligament remains as gubernaculum testis between the inferior pole of the testis and the
scrotum.
[The cavity of the tunica vaginalis is not continuous with the abdominal cavity because the vestigium
processus vaginalis is closed]
There is a tiny appendage on the superior pole of the testis which is the remnant of the Müllerian duct.
There is another tiny appendage on the epididymis called appendix epididymidis and is the remnant of the
mesonephros.
Layers of the scrotum:
Tunica vaginalis (visceral and parietal layers). Between the layers, there is a serous fluid which is
analogous to the serous fluid in the abdominal cavity.
Fascia spermatica. It layers the cremaster muscle on the inner surface. This fascia is the
continuation of the fascia transversalis.
Cremaster muscle. It is the continuation of the transverse abdominis muscle and internal oblique
muscle.
Fascia cremasterica. It is the continuation of the aponeurosis of the external oblique muscle.
This fascia is sometimes called external spermatic fascia. The spermatica is then called internal
spermatic fascia.
Tunica dartos. It is a skin muscle (smooth muscle inside the skin). This smooth muscle is responsible for the folding of the skin of the scrotum (for example, in cold weather). The tunica
dartos is the continuation of the superficial abdominal fascia (the fascia doesn't have smooth muscle
- only the tunica dartos).
Skin.
DUCTUS DEFERENS
The tail of the epididymis continues into the ductus deferens. The first part of the ductus deferens,
running parallel to the epididymis, is called the epididymic portion of the ductus deferens. The next portion,
the funicular portion, runs inside the funiculus spermaticus. The third portion is the inguinal portion,
passing through the inguinal canal. The last portion is the pelvic portion, running on the lateral wall of the
pelvis, covered by the peritoneum. It runs medial to the vesicula seminalis, forming the ampulla. The
ampulla joins the excretory duct (duct of vesicula seminalis), and the two together form the ejaculatory duct
which opens into the prostatic urethra.
VESICULA SEMINALIS
It is located on the posterior surface of the urinary bladder and is a very curved duct system, surrounded
by connective tissue. The duct of the vesiclus seminalis is called the excretory duct. The vesicula is
connected to the urinary bladder by the retrovesical fascia. It is infraperitoneal: the peritoneum reflects
onto the rectum above the vesicula.
It is related to the ampulla of the ductus deferens, which is medial to it. It is related to the urinary
bladder, and backward is related to the rectum.
94
PROSTATE GLAND
The gland is located below the urinary bladder. It has a base and an apex. The urethra pierces through
the gland and also the ejaculatory duct. The two ejaculatory ducts and the urethra separate a pyramidshaped area, from the prostate gland, which is called the isthmus (above the ejaculatory duct and behind the
urethra).
The gland is fixed by the pelvic fascia. It is related to the rectum (posteriorly) and is palpated through
the rectum. It is connected to the pubic symphysis by the puboprostatic ligament.
A very rich venous plexus surrounds the prostate gland which is called the plexus prostaticus, draining
into the internal pudendal vein.
PENIS
The penis has two main parts: corpus cavernosum and corpus spongiosum. They are separated from
each other by a connective tissue septum which is called septum pectiniforme. The corpus cavernosum
divides into two crura at the root of the penis. These two crura are attached to the ramus ossis ischii and the
fallic crest (it is at the border between the ramus pubis inferior and the ramus ossis ischii). Inside the
corpus cavernosum, we have the deep penile arteries which are responsible for the erection. The corpus
cavernosum is composed of the lacunae separated by trabeculae (connective tissue and smooth muscle).
The lacunae are layered by endothelium because blood is inside. The corpus spongiosum has three main
parts: 1 Bulbus penis, 2 Corpus (body), 3 Glans penis.
The bulbus penis is pierced by the urethra which then passes through the inferior part of the glans and the
corpus spongiosum. The lacunae of the corpus spongiosum are finer and smaller than the lacunae of the
corpus cavernosum, and they are not surrounded by tunica albuginea. The corpus cavernosum is. Both
are connected together by the fascia penis (connective tissue fascia). The two corpi can be separated from
each other, leaving a sulcus on the inferior surface of the corpus cavernosum.
The glans itself has a corona on the base, called the corona glandis, and a sulcus glandis. It also has an
apex. The penis is covered by the skin of the penis which forms the praeputium penis covering the glans.
It is attached to the sulcus coronarius and to the inferior surface of the penis by the frenulum preputii.
The crura penis are covered by a muscle called ischiocavernosus muscle. The bulbus penis is covered
by the bulbospongiosum muscle.
The penis itself is fixed to the pubis symphysis by the ligamentum suspensorium penis.
BLOOD SUPPLY:
Dorsal and deep penile arteries. These arteries have different branches (coiled) and during the
erection, the blood from these arteries enters the lacunae. They dilate, and the veins which drain the blood
from the penis compress, because they start from the peripheral part of the corpus cavernosum, right beneath
the tunica albuginea. The veins are compressed by the lacunae against the tunica albuginea, blocking
venous drainage during erection. The arterial blood flow increasses into the lacunae. This is by the
parasympathetic innervation. After the parasympathetic stimulation, the blood vessels dilate. After
sympathetic stimulation, they are constricted.
After ejaculation, the veins are released from the pressure, and the blood flow starts to work from the
periphery. The penis becomes flaccid again.
If the deep penile arteries are closed, the penis is always flaccid (no erection). If they are open, blood
can flow to cause an erection.
NERVE SUPPLY:
Dorsal penis nerve (from the pudendal nerve). It receives both sympathetic and parasympathetic fibers.
Parasympathetic fibers are from the sacral part through the visceral branches of the pudendohemoroid nerve.
Sympathetic fibers are from the lumbar part of the spinal cord (lumbar sympathetic trunk through the
hypogastric plexus or nerve).
95
FEMALE GENITAL ORGANS
Ovaries
Uterus
Fallopian tube
Vagina
External genitalia
OVARIES
They are located in the lesser pelvis at the division of the common iliac arteries. The ovary is 3 cm
long, 2 cm width, and 1 cm thick. It has a lateral surface, medial surface, and superior and inferior
extremities. It also has anterior and posterior margins.
The lateral surface is related to the division, but as the iliac blood vessels are retroperitoneal, the ovary is
separated from the blood vessels by the peritoneum. This lateral surface is also related to the ureter, which
is also separated from the ovary by the peritoneum (ureter is retroperitoneal).
Only a small anterior stripe and the anterior margin are covered by peritoneum, which are called the
margo mesovarium.
The medial surface of the ovary is related to the small intestine.
The superior pole is called extremitas tubarius because the Fallopian tube terminates here.
The inferior pole is called extremitas uterina because it is connected to the uterus by the proper ovarian
ligament (ligamentum proprium ovariae). This ligament continues into the teres uteri ligament (round
ligament of the uterus) which is inserted into the labia majora. These ligaments are analogous to the
gubernaculum testis in males.
The ovary is connected to the broad ligament by the mesovarium or mesovary. This anterior margin,
which is reached by the mesovary, is called margo mesovaricus. The posterior margin is free, not layered
by peritoneum, and is called margo liber (free border).
The lateral and medial surfaces are not layered by peritoneum (main part of them), so are extra peritoneal.
The line where the peritoneum terminates on the ovary is called Farre line.
The surface is layered by simple cuboidal epithelium..
Blood Supply:
From the ovarian artery coming from the abdominal aorta (paired visceral branches). The ovarian
artery reaches the ovary at the superior extremity, and these blood vessels (ovarian artery and vein) form a
fold on the posterior abdominal wall, which is called the ligamentum suspensorium ovarii (not a real
ligament, but a fold of the peritoneum formed by the two blood vessels). The ovarian artery reaches the
ovary through the mesovary and supplies it. It has tubal branches for the Fallopian tube (is also supplied
from the uterine artery that anastomoses with the ovarian artery). The Fallopian tube is very well supplied,
so well that a blastocyst can implant, eventually causing rupture of the tube. This is called extrauterine
gravidity (implantation is in the Fallopian tube).
96
Venous Drainage:
From the ovarian vein. The left ovary drains into the renal vein, and the right ovary drains into the
inferior vena cava.
UTERUS
The uterus is located in the lesser pelvis between the urinary bladder and the rectum. The peritoneum
comes from the anterior abdominal wall, covers the urinary bladder (apex and a small superior part of the
posterior wall), and is reflected onto the anterior wall of the uterus, forming the excavatio vesicouterina.
This reflection is between the cervix and the body, so the anterior surface of the cervix is not layered by
peritoneum. Then, the peritoneum reflects onto the posterior fornix of the vagina and to the rectum. This
reflection is called the Douglas cavity (or excavatio rectouterina) and is the lowest point of the abdominal
cavity. The uterus is an intraperitoneal organ, except the vaginal portion which is infraperitoneal (below the
peritoneum).
The uterus is in anteverted and anteflexed position. The anteversion means that the axis of the vagina
and the axis of the cervix form an angle. The axis of the cervix is anteverted approximately 70°-80° from
the axis of the vagina. The anteflexion means that the axis of the body of the uterus is bent anteriorly to the
axis of the cervix, forming an angle.
The uterus has a fundus (the free, upper part), a body, and a cervix. The first, narrower part of the
cervix (just below the body) is called the isthmus.
The lumen of the uterus has three main parts. In the body, there is a triangular cavity called the cavum
uteri (cavity of the uterus). The three apecies of this triangle are the ostium uterinum tubae (2) and the
ostium internum uteri. The internal orifice is between the cavum and the isthmus. The cavum uteri
continues into the canalis isthmi (small, constricted portion of the cervix). The isthmic canal continues into
the dilated canalis cervicis, which opens out on the vaginal portion of the cervix by the ostium externum
uteri.
The mucous membrane of the isthmus functionally belongs to the mucous membrane of the cavity (cavum
uteri). This mucous membrane is involved in the changes of the menstrual cycle and pregnancy. The
cavum, therefore, can be said to extend to the border between the isthmus and canalis cervicis. The canalis
cervicis doesn't go through the changes of the pregnancy. Functionally, the isthmus belongs to the cavity,
but morphologically is inside the cervix.
The innermost layer of the uterus is called the ENDOMETRIUM (mucous membrane), the middle layer is
called MYOMETRIUM (smooth muscle), and the outer layer is the PERIMETRIUM (serous layer mesothelium).
The length of the uterus is about 7-8 cm, but the length depends on whether it is before or after the first
pregnancy. The length of the cervix is 2.5 cm, and is standard.
Relations:
Anteriorly, it is related to the urinary bladder (the vesicouterine pouch separates them). Posteriorly, it is
related to the small intestine, and the Douglas cavity separates it from the rectum. It is related to the vagina
(vagina is attached to the uterus by anterior, posterior, and lateral fornices). The Fallopian tube starts from
the uterus, thus is related.
Support:
The uterus is supported by the urogenital membrane and pelvic diaphragm. The vagina pierces
through the urogenital membrane and is attached to it, thereby supporting the uterus. The superior fascia of
the pelvic diaphragm reflects onto the vagina and the cervix, fixing them to the diaphragm.
A connective tissue system surrounds the uterus at the level of the cervix and continues into the two
layers of the broad ligament (parametrium), then forms connections to the pubic symphysis and backward to
the sacrum. Thus, from the pubic symphysis, there is a ligament to the urinary bladder, and from the urinary
bladder to the cervix of the uterus. The first is called the pubovesical ligament, and the second is the
vesicouterine ligament.
The connective tissue system has also a transverse ligament from the cervix of the uterus to the lateral
wall of the lesser pelvis. This ligament is called ligamentum cardinale uteri or transversum. All this
connective tissue system together is called RETINACULUM UTERI.
97
The third support of the uterus is the broad ligament (ligamentum latum uteri). The uterus is layered
by the peritoneum. The anterior and posterior layers meet each other lateral to the uterus, forming a double
layer (broad ligament) connecting the uterus to the lateral wall of the lesser pelvis where it reflects onto the
parietal peritoneum.
The broad ligament has different parts. At the superior border of the broad ligament, the Fallopian tube
is also layered by peritoneum. This double layer, below the tube itself, is called the mesosalpinx. The
double layer which connects the ovary to the broad ligament is called mesovarium. The broad ligament is in
the frontal plane. As the ovary is behind the broad ligament, this mesovary is between the frontal and
horizontal planes. The mesovary terminates on the anterior margin of the ovary. The posterior margin is
not covered. Below the mesovarium, lies the mesometrium, the largest part of the broad ligament.
Between the two layers of the broad ligament, there is loose connective tissue parallel to the uterus.
This connective tissue is called parametrium. Inside this parametrium, the uterine artery reaches the uterus
at the isthmus. From the isthmus, it runs upward as a wavy artery, along side the uterus in the parametrium.
It gives tubal branches for the Fallopian tube, and the endbranch gives ovarian branches for the ovary.
When it reaches the isthmus of the uterus, it gives a descending branch for the vagina called the vaginal
artery (or vaginal ramus of the uterine artery).
LYMPHATIC DRAINAGE OF THE UTERUS:
There are three courses of lymphatic drainage:
1
One from the fundus of the uterus along side the round ligament, through the inguinal canal into the
inguinal lymph nodes (parallel to the inguinal ligament).
2
From the body of the uterus, along side the uterine artery, to the nodi lymphatici interiliaci (along side
the internal iliac artery). From these nodes, they go along side the common iliac lymph nodes
(along side the common iliac artery) and from there, to the paraaortic lymph nodes (parallel to the
abdominal aorta). The paraaortic nodes go through the lumbar trunk to the cisterna chyli.
3
From the cervix, there are two courses. One is the same as for the body (aside the uterine artery).
The other is through the posterior fornix of the vagina into the sacral lymph nodes on the pelvic
surface of the sacrum. From the sacral nodes, lymph goes directly up to the paraaortic nodes.
Medical importance: if enlarged inguinal lymph nodes are discovered, it means that the whole
lower limb, perineal region, anal opening, gluteal region, and external genitalia must be
examined. If no problem is found there, tumors of the uterus (fundus of
the uterus) may be indicated. Usually in the case of the uterine cancer, the paraaortic and
iliac lymph nodes are enlarged.
Lymph Vessels:
They are found in the parametrium, running along side the uterine artery.
If the patient has parametritis (inflammation), it is spreading in the loose connective tissue.
The part of the cervix which is located in the vagina is called vaginal portion. The remaining portion is
the supravaginal portion. The vaginal portion of the uterus is very important because gynecologists examine
this portion through the vagina by a colposcope. This portion is also important during delivery because the
baby comes out from here.
The external orifice, being on this portion, is an oval opening. Sometimes, erosions (wounds) are found
there.
98
FALLOPIAN TUBE (or uterine tube)
It starts from the uterus by the uterine ostium and continues into the isthmus (approximately 3-4 cm long).
After that, the Fallopian tube is getting dilated and continues into the ampulla, terminating by the fimbriae
around the superior extremity of the ovary. The whole tube is about 10-12 cm long. The first part, coming
from the uterus, is transverse. The next part turns backward and terminates on the ovary. The fimbriae are
called ovarian fimbriae (fimbriae ovariea).
The Fallopian tube is supplied by both the ovarian and uterine arteries that anastomose in the
mesosalpinx. The blood supply of the tube is very rich.
The mesosalpinx connects the Fallopian tube to the broad ligament.
VAGINA
The vagina is approximately 7-8 cm long, and is attached to the uterus by anterior-posterior and lateral
fornices.
The inlet of the vagina is in the vestibulum vaginae where it is surrounded by the bulbus vestibulae on
both sides. The bulbus vestibulae is analogous to the bulbus penis in males, but the structure is a little
different. The bulbus vestibulae is a rich venous plexus surrounded by connective tissue capsule, but the
bulbus penis has a spongy structure.
The axis of the vagina is 30° posterior from the vertical. In the upper part, we have the vaginal portion
of the uterus.
The vagina is related to the rectum posteriorly, but it is separated from the rectum by the rectovaginal
septum, a thick connective tissue septum. The inferior part of the rectum, which has the perineal flexure, is
far from the vagina, because the septum is very thick. Anteriorly, it is related to the urethra. There is
another a septum here, which is called the urethrovaginal septum. This septum is not so thick as the
posterior one.
The lateral fornix of the vagina has a very important relation. It is related to the ureter, because the
ureter runs forward to the urinary bladder from the posterior abdominal wall. It must pass lateral to the
uterus and lateral to the fornix of the vagina. Here, it has the crossing with the uterine artery. This is
important: to operate on the uterus, the artery should be ligated and cut, but there is danger of cutting the
ureter by accident.
The vagina has the so-called rugae vaginalis (transverse folds).
The epithelium of the vagina is stratified squamous (pale because of the removal of the glycogen; cells
look empty).
The vestibulum of the vagina receives the external ostium of the urethra, in front of the ostium of the
vagina. The vestibule is surrounded by the labia minora. It receives the secretion of the glandula
vestibulae major (or Bartolini gland), which is analogous to the bulbourethral gland in males. This gland is
located at the lateral border of the urogenital membrane.
EXTERNAL GENITALS
The labia majora are analogous to the scrotum. The labia minora surround the vestibulae vaginae, and
they continue into each other behind, forming the fossa vestibulae vaginae. In front, they are connected to
the clitoris and continue into the preputium of the clitoris. In the inferior surface of the clitoris, the
frenulum clitoridis continues into the labia minora.
The clitoris is analogous to the glans penis. There is no analogous structure of the labia minora in
males.
MIDSAGITTAL SECTION OF THE FEMALE PELVIS
There is a big preparation in the dissecting room with a midsagittal section of the female pelvis with the
uterus, urinary bladder, and rectum. This may be given as the "organ" in the final exam. In addition to the
individual organs as described above, there are some general considerations.
Anteriorly, we will see the pubic symphysis. Posteriorly, we find the sacrum.
Posterior to the pubic symphysis, lie the uterus and vagina, then the rectum with the sacral and the
perineal flexures (S-shaped).
In this preparation, the course of the peritoneum is always asked. This includes the pouches.
99
Be prepared to speak about the anteversion and anteflexion of the uterus. The round ligament keeps the
uterus in the anteverted and anteflexed position.
If the urogenital membrane and pelvic diaphragm become loose (in women of older age), the uterus
descends and may appear even in the vestibulum vaginae. This can be corrected by operation (suture of the
urogenital membrane and pelvic diaphragm).
DIAPHRAGMS OF THE LESSER PELVIS
Two diaphragms close the outlet of the lesser pelvis.
These are the pelvic and urogenital diaphragms.
PELVIC DIAPHRAGM
The pelvic diaphragm is composed of a muscle, the levator anni muscle, and two fascia. One fascia is
above the levator anni, and one is below. The superior fascia is called fascia diaphragmatis pelvis superior
(also called the pelvic fascia). The inferior fascia is the fascia diaphragmatis pelvis inferior.
Origin of the levator anni muscle:
The first part (anterior part) arises from the pubic bone, lateral to the pubic symphysis. These fibers
run straight backward and cross each other in the midline, forming a U-shaped hiatus called the
urogenital hiatus (or genital hiatus). These crossed fibers meet each other again, surrounding a round
hiatus called the anal hiatus (for the anal opening). These fibers are attached to the coccyx and to the
lower part of the sacrum. So, this anterior part of the muscle is called PUBOCOCCYGEAL MUSCLE.
The second part arises from the arcus tendineus fasciae pelvis, which bridges the obturator internus
muscles (covers the obturator foramen from the inner surface). This part of the muscle is called
ILIOCOCCYGEAL PART. These fibers are also attached to the coccyx and to the inferior part of the sacrum.
The third part of the muscle arises from the spina ischiadica and from the sacrospinous ligament.
This part is called the ISCHIOCOCCYGEAL PART, attached to the coccyx and the sacrum. This part is also
called musculus coccygeus.
All the muscle fibers form a funnel-shaped muscle which is more narrow inferior.
UROGENITAL DIAPHRAGM
The urogenital hiatus is covered by another diaphragm below, which is called the urogenital diaphragm.
This diaphragm is also composed of three layers: one muscle and two fasciae. The muscle is the deep
transverse perineal muscle, which arises from the inferior ramus of the pubic bone and from the ramus of the
sciatic bone (ramus ossis ischii). It is a transverse muscle between the inferior rami of the pubis bones.
It has a fascia below, which is called the fascia diaphragmatis urogenitalis inferior and a fascia above
which is called fascia diaphragmatis urogenitalis superior. This fascia is pierced by the urethra (in front)
and by the vagina (behind). In males, only the urethra pierces.
Between the two diaphragms, there is a space called the deep perineal space.
The urogenital diaphragm is layered by a fascia, which is called the fascia perinei superficialis.
Between this fascia and the diaphragm is another space called the superficial perineal space. This space
contains the following muscles: ischiocavernosus, bulbospongiosus, and the superficial transverse perineal
muscle. These muscles form a triangular shaped structure.
The third space is above the pelvic diaphragm. Above the pelvic diaphragm, the peritoneum reflects
onto the different organs (urinary bladder, uterus, and rectum). Between the peritoneum and the pelvic
diaphragm, lies the subperitoneal space. This space contains connective tissue and the blood vessels and
nerves for the organs of the lesser pelvis.
The fossa ischiorectalis is at the same level as the deep perineal space. It is open below because it isn't
covered by the urogenital diaphragm. It is covered only by the superficial perineal fascia. The contents of
this fossa are the pudendal nerve, internal pudendal artery and vein. These structures run in a canal called
the pudendal canal or Alcock's canal. This canal is along side the lateral wall of the fossa ischiorectalis,
100
formed by the obturator internus muscles, covered by the fascia obturatoria (reduplication of this fascia
forms the canal). The structures of the pudendal canal arising into the perineal region divide into branches.
The walls of the fossa ischiorectalis are: Levator anni muscle and inferior pelvic fascia (MEDIAL); Obturator
internus muscle covered by the obturator fascia (LATERAL).
The deep perineal space is pierced by the vagina and by the urethra. The subperitoneal space contains
loose connective tissue, blood vessels, and nerves. The superficial perineal space contains the
bulbospongiosus, ischiocavernosus, and superficial transverse perineal muscle.
PERINEAL REGION
This region includes the pelvic and perineal diaphragms and the branches of the pudendal nerve and
internal pudendal artery.
The urogenital diaphragm lies deep to the skin. The muscles of the superficial perineal space are found
on the diaphragm. You can also find the structures of the pudendal canal and their branches.
Branches of the internal pudendal artery have been previously discussed.
Branches of the pudendal nerve:
1
Muscular branch,
2
Nerve for the penis (dorsal penile nerve).
These branches are located through the ischiorectal fossa or on the surface of the urogenital diaphragm,
but one branch runs through the deep perineal space (dorsal penile artery and nerve) until the symphysis. It
comes through a hiatus between the symphysis and anterior border of the urogenital diaphragm, called the
subarcuate hiatus. It is so named for the arcuate ligament on the inferior surface of the pubis.
In this region, we will also find the external genitals.
Between the vestibulum vaginae and the rectum, we have the so called centrum tendineum or the perineal
body. This is a connective tissue center between the vagina and the rectum (F) or between the bulbus
spongiosus and rectum (M).
Right Iliac Fossa:
Cecum, appendix, terminal ileum (where it joins the cecum), the lumbar plexus
(behind the peritoneum).
Left Iliac Fossa:
Sigmoid colon. Lumbar plexus behind peritoneum
101
SPINAL CORD
The spinal cord is approximately 50 cm long and is found in the vertebral canal. It begins at the level of
the foramen magnum and terminates at the level of the first or second lumbar vertebra. Below this level, the
cord divides into the cauda equina ("horse tail"), formed by spinal roots from the "sacral segments" of the
cord and by the filum terminale of the pia matter. The lumbar and sacral parts of the spinal cord are found
at the level of the thoracic vertebrae [the rule of Chipault is a system relating spinal segments to the level of
the vertebrae, but it isn't necessary to know for the exam]. To reach their appropriate lumbar vertebrae and
sacral foramina, the spinal roots must descend inside the vertebral canal. The termination of the spinal cord
at this level is called the conus medullaris (or conus terminalis) for its cone-like shape.
On the spinal cord, there are enlargements due to a larger number of neuron cell bodies for innervating
the upper and lower limbs. The origins of the cervical and brachial plexi are the lower cervical portion, so
there is an enlargement called the intumescentia cervicalis. There is a similar enlargement in the lumbar
cord where the lumbar and sacral plexi arise (intumescentia lumbosacralis).
On cross section, neuron cell bodies form the grey matter of the spinal cord, having a butterfly-shaped
appearance. Surrounding the grey matter is the white matter, composed of the axons of the neurons. These
axons form ascending and descending tracts throughout the spinal cord.
On the anterior surface is a deep fissure called fissura mediana anterior. On the posterior surface is a
sulcus called the sulcus medianus posterior. These features allow us to distinguish anterior from posterior
on the cord as does the wider anterior horn of the grey matter.
The grey matter forms anterior, posterior, and lateral horns. The lateral horns exist only in the thoracolumbar part of the spinal cord and contain the sympathetic neuron cell bodies.
The spinal cord gives rise to two anterior (ventral) roots and two posterior (dorsal) roots. These roots
unite to form the spinal nerve. The spinal nerve is very short, dividing into ventral and dorsal rami. The
roots are inside the vertebral canal, the spinal nerve is inside the intervertebral foramen, and the rami of the
spinal nerve are outside the vertebral canal.
The dorsal root is purely sensory, and the ventral root is purely motor. The spinal nerve and its rami are
mixed.
On the dorsal root is the DORSAL ROOT GANGLION (or spinal ganglion, or intervertebral ganglion).
Inside are the sensory neuron cell bodies. These are pseudounipolar neurons (a cell body with one axon
which divides into two right after the origin). Functionally, it is bipolar, but morphologically, it appears to
be unipolar, hence the name.
The central axon of this neuron cell body enters the spinal cord and terminates inside the spinal cord or
ascends in one of the dorsal column pathways. The peripheral process of this pseudounipolar cell body runs
out to the periphery and termiates in a receptor. The direction of the impulse inside the dorsal root is
therefore afferent.
The ventral root is pure motor, meaning it has axons originating from the lateral or ventral horn of the
spinal cord grey matter. Axons running out to the periphery terminate in a skeletal muscle, smooth muscle,
or gland. The direction of the impulse is efferent.
The spinal cord is composed of 1-2 cm long sections, each belonging to one pair of spinal nerves. These
are the spinal-cord segments. The spinal cord is continuous, so these segments are not visible. The cord
has 8 cervical segments. The ventral rami of the first four cervical segments form the cervical plexus, while
the dorsal rami remain segmented. The ventral rami of spinal nerves C5-T1 form the brachial plexus,
innervating the upper limb, while the dorsal rami remain segmented. There are 12 thoracic segments. The
ventral rami of the thoracic spinal nerves remain segmental and form the intercostal nerves. There are 5
lumbar segments. The ventral rami of the first four form the lumbar plexus, while the dorsal rami remain
102
segmented. Ventral rami of nerves below L4 form the sacral plexus which can be divided into the sciatic
plexus and the pudendohemoroid plexus. Dorsal rami remain segmental.
The dorsal rami innervate muscles of the nuchal region, deep muscles of the back, and the overlying skin.
The dorsal rami of the first, second, and third cervical segments form the suboccipital, greater occipital, and
tertiary occipital nerves, respectively. The dorsal rami of the first three lumbar nerves form the superior
cluneal nerves. The dorsal rami of the first three sacral nerves form the medial cluneal nerves. Only these
segments of the dorsal rami have names, but the dorsal rami always remain segmented.
MEMBRANES OF THE SPINAL CORD
The spinal cord has three membranes: the dura mater (outermost), arachnoidea (middle), and the pia
mater (innermost).
The dura mater has two layers that start at the level of the foramen magnum. Above the foramen
magnum (in the skull), the dura mater has only one layer. In the vertebral canal, the outer layer is the
endorachis (periosteum of the vertebrae, continuous through the entire length of the spinal column), and the
inner layer is the dura mater proper. Between them is a rich venous plexus, called plexus venosus
vertebralis internus which drains into the p.v.v. externus. This space is called the epidural space (cavum
epidurale).
The arachnoid membrane is a very thin connective tissue membrane, so thin as to resemble the web of a
spider (hence the name). Between the dura mater and the arachnoid membrane, we identify a so-called
subdural space, but it isn't a real space.
The pia mater follows the surface of the spinal cord everywhere. Between the arachnoid layer and the
pia mater, there is a real space called the subarachnoid space, filled by cerebrospinal fluid. Between the
arachnoid and pia mater are tiny ligaments called denticulate ligaments. These ligaments are not continuous
they are found only at the level of the spinal nerves. The denticulate ligaments arise from the pia mater
and are attached through the arachnoidea to the dura mater, providing support for the spinal cord. The dura
mater is fixed to the foramen magnum, further fixing and supporting the spinal cord.
The cerebrospinal fluid provides buoyant support for the spinal cord, thus reducing its effective weight
inside the vertebral column.
The dural sac terminates at the level of segment S2. Below the termination of the spinal cord, the cauda
equina is surrounded by the arachnoidea and the cerebrospinal fluid (in the subarachnoid space). We can
drain fluid from the subarachnoid space by the lumbar puncture. This puncture should be done below L2 to
avoid injury to the spinal cord. The 1 supraspinous ligament, 2 interspinous ligament, and the 3 dura mater
must be pierced.
The dura mater follows the spinal roots until the intervertebral level and here is attached to the intervertebral foramen.
BLOOD SUPPLY OF THE SPINAL CORD
The spinal cord is supplied by the spinal arteries (one anterior and two posterior). The spinal arteries
arise from the vertebral arteries. The basilar artery arises as the union of the two vertebral arteries at the
level of the medulla and pons.
The vertebral arteries give rise to two anterior spinal arteries which reunite to form a single ventral spinal
artery, running down the fissura mediana anterior. Two dorsal spinal arteries also arise from the vertebral
arteries, but these remain separate. Thus, there are two dorsal and one ventral. The dorsal arteries are
located lateral to the fila radicularia.
The ventral and dorsal radices leave the spinal cord through tiny filaments called the radicular filaments.
The ventral filaments leave the spinal cord lateral to the anterior median fissure from the small ventrolateral
103
sulcus. The dorsal fila radicularia leave through another fissure called the dorsolateral fissure. The dorsal
(posterior) spinal artery is lateral to the fila radicularia next to the dorsolateral sulcus.
There is an anastomosis ring between the three arteries which is called ramus arcuatus. These arteries
are enriched by the radicular branches of the segmental arteries. Along the side of the ventral and dorsal
radix are the radicular arteries which arise from the segmental arteries.
The grey matter of the spinal cord is supplied by the anterior spinal artery through tiny arteries called the
arterias fissurai medianai anterioris. These arteries reach the grey matter through the fissure and supply
the grey matter (80%). The arcuate branches supply the white matter (from the posterior spinal artery).
VENOUS DRAINAGE is given by the plexus venosus vertebralis internus (anterior and posterior), draining
to the p.v.v. externus (anterior and posterior), then to the azygos, vertebral, or lumbar vein.
GREY MATTER
The grey matter has ventral, dorsal, and lateral (thoracolumbar region only) horns as discussed
previously.
The ventral horn contains the motor neurons innervating limb and trunk muscles. Inside the ventral
horn, we can identify different regions or groups of neurons. The ventrolateral group innervates the limb
muscles, and the ventromedial group innervates the trunk muscles. In some levels, there is an intermediate
group between the first two. For example, in the spinal segments C3-C4 is the nucleus of the phrenic nerve.
Above this is the spinal nucleus of the accessory nerve.
The lateral horn contains the intermediolateral nucleus, containing the sympathetic neuron cell bodies
(on the thoracolumbar part) or the parasympathetic neuron cell bodies (in the sacral part).
The dorsal horn can be divided into vertical layers called laminae by the Rexed system. The grey
matter is thus divided into ten regions with the first six forming dorsal horn laminae. Books which a clinical
focus rather than an emphasis on research opt for a system of nuclei rather than the Rexed laminae system.
I
In the dorsal horn, the first lamina is the marginal zone of Waldeyer.
II
Rolando's substantia gelatinosa.
III
Intermediate zone.
IV
This has a nucleus in the medial part of the lamina called Clarke's nucleus, or the nucleus
dorsalis. It is found only in the thoracolumbar region. Its cells give rise to the axons of the dorsal
spinocerebellar tract.
V
This lamina is called the head of the dorsal horn or the nucleus proprius.
VI
The root of the dorsal horn; it also contains the Clarke's nucleus.
VII
This is the intermediate zone of the grey matter. In the lateral part is the intermediolateral
nucleus and another, tiny nucleus called the intermediomedial nucleus.
VIII The medial part of the ventral horn. It was once called the commissural lamina, because it was
thought that some fibers crossing through the ventral commissure.
IX
The lateral part of the ventral horn.
X
Surrounding the central canal; contains interneurons.
CENTRAL CANAL: The cavity of the spinal cord is called the canalis centralis. It is the continuation of the
ventricles of the brain. It is layered by a special type of glial cells called ependyma (morphologically, it
appears to be simple columnar epithelium with a process on each cell). The canal has a small amount of
cerebrospinal fluid continuous with that of the ventricles of the brain.
WHITE MATTER
It is divided by the grey matter into anterior, lateral, and dorsal (posterior) columns. The anterior
column is located between the anterior median fissure and the anterior root. The lateral column is located
between the anterior and posterior root. The posterior column is between the posterior root and the sulcus
104
medianus posterior. From the sulcus medianus posterior, there is a septum which separates the two sides of
the posterior column (not an absolute separation, just a septum).
These columns contain the ascending and descending fibers of the spinal cord. In the dorsal column are
two fascicles called fasciculus gracilis (of Goll) and fasciculus cuneatus (of Burdach). These fascicles
contain the ascending fibers of the sensory neuron cell bodies located in the spinal ganglia. These fibers
terminate in the like-named nuclei in the medulla oblongata. Fibers from the nuclei continue along another
pathway called the lemniscus medialis and carry impulses from the periphery, namely vibration, position
sense, touch, pressure, and discrimination sense.
The fibers of Goll's fascicle (medial) are longer than those of Burdach's fascicle (lateral). The fibers
which carry impulses from the little finger are the longest. The shortest fibers arise in the C1-C2 segments.
Both Goll and Burdach fascicles can be found in a cross section of the spinal cord in the cervical region,
but if the section is made in the thoracic level, only the Goll fascicle is found. Inside these fascicles is a
comma-shaped fascicle called Schultze's comma fascicle. This contains the descending fibers of the Goll
and Burdach tracts. A collateral of the main ascending fibers descends just 2 or 3 segments to form
interconnecting fibers (between the segments of the spinal cord).
Both descending and ascending pathways are found in the lateral column. The most important
descending pathway is the corticospinal tract or the crossed corticospinal tract (tractus corticospinalis
cruciatus). That means that the fibers arising from the motor cortex descend through the brain stem down to
the spinal cord, then 90% of these fibers cross each other at the level of the medulla, while the other 10%
remain uncrossed. The crossed fibers run in the lateral column, and the uncrossed fibers run in the ventral
column. The crossed corticospinal tract (pyramidal tract) terminates on the motor neurons of the ninth
lamina, innervating skeletal muscles of the limbs. This pathway forms the so-called supranuclear
innervation for the motor neurons of the ninth lamina. If you cut the pyramidal tract, the result is paralysis.
This pathway is responsible for voluntary movements.
The uncrossed pyramidal tract innervates the trunk muscles. These fibers also cross; not at the level of
the medulla, but at the level of the spinal cord (at the same level of the motor neurons they innervate). For
example, the fiber which descends to the L3 level (origin of the femoral nerve) crosses to the other side at
that level. Thus, all the corticospinal fibers cross eventually, either in the medulla or in the spinal cord.
There is another descending tract called the rubrospinal tract. It originates from the nucleus ruber of the
mesencephalon and terminates on the same motor neurons as the pyramidal tract fibers, but this tract belongs
to the so-called extrapyramidal system. All descending tracts not among the pyramidal tracts belong the
extrapyramidal system. This system coordinates and initiates voluntary movements. Handwriting and
manual dexterity belong to this system. If injured, such movements are possible, but neither continuous nor
coordinated.
In the lateral column are ascending tracts called anterior (Gower's) and posterior (Flechsig's) spinocerebellar tracts. Flechsig's tract arises from the Clarke's column and is uncrossed. Gower's tract arises
from the nucleus proprius and is crossed. These tracts terminate in the cerebellum and carry information
from the limbs (mainly about position sense).
Another ascending tract here is called the spinothalamic tract. It terminates in the thalamus, a large
structure of the diencephalon. It is crossed (through the white commissure, or commissura anterior) and
originates in the dorsal horn, mainly from layers I and IV. It carries information from the protopathic
senses, including pain, temperature, and superficial touch. All of them come from the superficial receptors.
If you cut these tracts, pain cannot be felt below the level of the transection on the opposite side. The
spinothalamic tract also extends into the anterior column.
The anterior column contains the uncrossed pyramidal tract plus several extrapyramidal pathways:
vestibulospinal, tectospinal, and olivospinal tracts, and the fasciculus longitudinalis medialis. All these
tracts arise from the medulla or the mesencephalon and terminate on the motor neurons of the spinal cord.
The extrapyramidal system includes all motor fibers of the spinal cord outside the pyramidal system.
The pyramidal and extrapyramidal systems terminate on interneurons which in turn terminate on the
motor neurons. Finally, these interneurons collect all information from both systems. The end result on
the motor neurons depends on differing descending impulses.
LONG FIBERS ARE ALWAYS SUPERFICIAL TO THE SHORT FIBERS
105
SPINAL REFLEXES
There are three important reflexes which are close in the spinal cord (and don't require the brain to
function). These are 1 Proprioceptive (or myostatic or stretch reflex), 2 Nociceptive (or crossed flexorextensor reflex), 3Vegetative.
PROPRIOCEPTIVE: it means that it is the proper reflex of the muscle. The receptor and the effector are
in the same muscle. The receptor takes the stimulus and the effector contracts the muscle. This reflex
works against gravitation. There are many receptors of this kind in the antigravity muscles (i.e. flexor
muscles of the upper limb). Generally, a reflex is composed of three main parts: the receptor (receiving the
stimulus), the central synapse (between afferent fiber and efferent cell), and the effector (inside the muscle or
gland and affects it). The fiber between the receptor and the center is called afferent. The fiber arising
from the center is the efferent fiber, going to the effector.
The stimulus of the proprioceptive reflex is stretching of the muscle, detected by a receptor organ called
the muscle spindle. The gamma neuron originates from the lamina IX of the spinal cord. It terminates at
the end of the muscle spindle and can influence its activity. By contracting the intrafusal fibers, it sends
signals to the muscle spindle. The effect of the gamma neuron on the muscle spindle is the same as the
effect of stretch on the muscle fibers. These gamma neurons are influenced by the descending,
extrapyramidal pathways.
They can modify the impulse of the muscle spindle even if the muscle is contracted. In this case, they
won't be so sensitive to the stretching. The gamma neurons also receive fibers from the collateral
(periphery). So, receiving fibers from the center and from the collateral, they can modify the sensitivity of
the muscle spindle. It is a servo-mechanism which modifies the proprioceptive reflex (making the muscle
spindle more sensitive).
Gamma neurons terminate in the muscle spindle end portions. The muscle spindle is found in the
intrafusal fibers. These are surrounded by the Ia type thick fiber belonging to the pseudo-unipolar neuron in
the spinal ganglion. This fiber enters the spinal cord and synapses with the large motor neurons in lamina
IX. The motor neurons terminate in the extrafusal fibers, stimulating muscle contraction. This course of
the fibers is called the gamma loop. The proprioceptive reflex keeps the normal muscle tone.
NOCICEPTIVE: the root word "noxa" means the stimulus causes tissue damage. For example, if you
suffer a burn on the finger, the sense of the reflex is to move away from the source of the heat while the other
hand moves to try to distance the body from it. This reflex is also called the flexor cross-extensor reflex.
Reflex arch: The afferent neuron belongs to the dorsal root ganglion. These neuron cell bodies are
usually smaller than the neurons cell bodies of the proprioceptive reflex. Thus, inside the dorsal root
ganglion are large, pseudounipolar cells and smaller cells. The large neurons have thick, myelinated axons,
and the small neurons have thin myelinated or non-myelinated axons.
The receptor which is reached by the peripheral process of this neuron is usually a free nerve ending in
the skin, receiving pain or temperature signals (protopathic).
The central axon of this neuron terminates in the gelatinous substance of the dorsal horn of the spinalcord grey matter. This region is composed of very small neurons which transmit the impulse to motor
neurons in the lamina IX (ventral horn). Impulses from the somatomotor neurons travel along the axons
which leave the spinal cord through the ventral root and terminate in the flexor muscles of the limb
experiencing the stimulus. Another fiber crosses the midline to the contralateral lamina IX. These motor
neurons innervate the extensor muscles of the opposite limb (not the stimulated limb). For example, if the
right foot is burned, the right flexor muscles retract the limb while the left extensor muscles push the body
away from the source of injury.
The crossing fibers do so through the grey and white commissures. Here, some of the fibers form an
ascending tract in the ventral and lateral column called the spinothalamic tract. You will feel the pain
sensation because an impulse is sent to the brain along this tract. Thus, there is a connection between the
spinal-cord reflex and the conscious sensation of the stimulus. Only a strong pain stimulus will send a
106
signal up the spinothalamic tract. A smaller stimulus will trigger the reflex without a perceived sensation of
pain.
Just posterolateral to the dorsal horn (appearing to surround the "tip" of it) is the Lissauer tract. This
tract contains fibers which interconnect adjacent segments. Pain sensory impulses can be carried to adjacent
segments for the multi-level reflex responses involving flexors and extensors of multiple joints.
Head zone: The skin which is innervated by the same segment as the muscle (or the viscera) is called
the head zone. Painful stimuli to a muscle or organ can cause a sensation of pain in the corresponding
region of skin. For example, in cases of cholecystitis (inflammation of the gall bladder), the skin overlying
the gall bladder becomes hypersensitive to touch.
There is one head zone which doesn't cover the muscle innervated by the same segment. This is the C4
segment (phrenic nerve). The head zone is at the topographical level of C4, but the muscle innervated is the
diaphragm. Thus, painful stimuli to the diaphragm will cause a secondary pain sensation in the skin of the
neck.
The neurons that are activated by these pain fibers are innervated by the thick, myelinated fibers. These
fibers synapse with the inhibiting interneurons which block the pain sensation. For example, if you press
the hand at the same time a painful stimulus is applied, the sensation of pain will be decreased. This results
from activation of the thick fibers from the deep tissue receptors (such as muscle receptors) synapsing to the
interneurons. This inhibits the synapse of the pain fibers to the spinothalamic neurons, thus inhibiting the
pain sensation.
In the spinal cord level, the pain sensation could be influenced by other sensations (from deep receptors
or from descending tracts terminating on the inhibitory interneurons. Some people are more sensitive to
pain and some are less, depending on the organization of the spinal cord or mesencephalon.
VEGETATIVE: The vegetative (or autonomic) reflex is so called because it originates from the organs
(the viscera). The receptors of this reflex are called interoceptors, being inside the body. Of these are 1
chemoreceptors, 2 baroreceptors, and 3 pressoreceptors.
The sensory neuron is located in the spinal ganglion. The central processes of these dorsal root ganglion
cells enter the spinal cord through the dorsal root and terminate on an interneurons which synapse with the
lateral horn vegetative neurons (in the intermediolateral nucleus). The efferent part of the reflex belongs to
this vegetative neuron, giving axon fibers through the ventral root, spinal nerve, and terminating in the
ganglion. These are the preganglionic fibers. The ganglion could be paravertebral or prevertebral. These
fibers reach the paravertebral ganglion as rami communicantis albi. If they synapse inside, grey
communicating fibers (postganglionic) emerge that return to the spinal nerve and pass out to the different
organs (pseudomotor, pilomotor, vasomotor). If the preganglionic fibers pass through the ganglion without
synapsing, they form the SPLANCHNIC NERVES (T6-9: Greater Splanchnic nerve, T10-12: Lesser Splanchnic
nerve) and reach the prevertebral ganglia, where they synapse. From there, postganglionic fibers arise and
reach the target organs (smooth muscle and various glands).
The receptors (chemo-, baro-, presso-) can be also pain receptors in the case when the vegetative reflex
and the proprioceptive reflex mix. For example, in an inflammation of the gall bladder, the interoceptor is a
pain receptor of the peritoneum. The peritoneum is rich in pain receptors.
Sometimes, the vegetative and proprioceptive reflexes are connected with each other. For example, if a
patient has appendicitis, the abdominal muscles may be stimulated to contract, creating a clinical sign for the
examining doctor. This contraction is a reflex stimulated by an afferent stimulus from the viscera. The
afferent part is the vegetative reflex, while the efferent part is the proprioceptive reflex (causing the
contraction of the muscles).
Summary: For each reflex, you should identify the following elements: 1 receptor, 2 afferent neuron, 3
central part, 4 efferent neuron, 5 effector (termination).
Viscerovisceral reflex: originated from the viscera and acts on the viscera.
Viscerosomatic reflex: receptor is in the viscera, the effector is in a skeletal muscle.
107
Functionally, we can divide the grey matter into: ventral horn (somatomotor), lateral horn
(vegetative/visceromotor/autonomic), dorsal horn (sensory).
Three types of neuron cell bodies can be found in the grey matter. According to the course of the
axons, we classify them so:
Funicular: the axon of the neuron leaves the grey matter and ascends or descends in the white
matter, forming a "funicle" (column) of the white matter. For example, axons from cells in Clarke's
column form the spinocerebellar tract.
Radicular: the axon fiber forms a root (ventral root). For example, all the neurons in lamina IX
belong to this type because their axons pass through the ventral root and go out to the skeletal
muscle.
Interneurons: interconnecting two neurons (sensory and motor). The interneurons remain in the
same segment and don't go beyond the grey matter.
108
CEREBRUM
BLOOD SUPPLY
The vertebral and internal carotid arteries give the blood supply for the brain.
The two vertebral arteries enter the skull through the foramen magnum and unite between the medulla
and pons to form the basilar artery (running in the basilar sulcus of the pons). The basilar artery divides into
two posterior cerebral arteries at the anterior border of the pons.
The internal carotid artery comes into the skull through the carotid canal and divides into two branches:
the middle cerebral artery and the anterior cerebral artery. The anterior cerebral artery runs toward the
longitudinal fissure (between the two hemispheres) and turns onto the dorsal surface of the corpus callosum,
running backward on it. This artery supplies the medial surface of the hemispheres plus a one-finger-width
stripe along the side of the longitudinal fissure. The end branches of the artery run out from the fissure onto
the convex surface.
The middle cerebral artery runs into the lateral sulcus, on the insula (giving branches which run onto the
insula). This artery supplies the convex surface of the brain with the following exceptions: the previously
mentioned stripe, the occipital lobe, and the inferior surface of the temporal lobe. It supplies the internal
capsule, basal ganglia, nucleus lentiformis, nucleus caudatus, and thalamus by the thalamostriate and
lenticulostriate arteries (the middle cerebral artery and these two branches are the most common sites of
intercranial hemorrhage leading to a stroke).
The internal capsule is a very important white-matter tract of the brain which contains the so-called
projection tracts-- the long fibers which ascend to the cortex or descend from the cortex. Another relatively
frequent site of hemorrhage is the internal capsular artery (from the middle cerebral artery).
The middle cerebral also gives an artery for the choroid plexus of the lateral ventricle. This choroid
plexus produces the cerebrospinal fluid. The plexus has a very rich arterial plexus inside plus an epithelial
lamina and the pia matter. The epithelial lamina invaginates near the pia mater (which is rich in blood
vessels) to form the choroid plexus. This is a single epithelial layer, remaining from the original neural
tube.
The posterior cerebral artery supplies the occipital lobe and the inferior surface of the temporal lobe. It
gives choroid arteries for the choroid plexus of the third ventricle (posterior choroid artery).
Between the posterior cerebral and internal carotid arteries (or sometimes middle cerebral artery) is a
communicating artery called the posterior communicating artery.
There is another communicating artery between the two anterior cerebral arteries called the anterior
communicating artery. This completes an arterial circle surrounding the hypothalamus and the optic
chiasma. This is called the circulus arteriosus cerebri (circle of Willis). This circle can be used to easily
locate the hypothalamus (a frequently asked question!).
We are able to ligate one vertebral artery without ill effect because the whole brain will be supplied by
the other. Blood supply remains almost completely intact with only a slight decrease in blood pressure). If
you ligate an artery after the circle, the corresponding part of the brain will necrotize.
The basilar artery gives branches for the pons (rami adponte) and an artery to the cerebellum (by its
division into the two posterior arteries) called the superior cerebellar artery. It also gives another artery for
the cerebellum called the inferior anterior cerebellar artery. The inferior posterior cerebellar artery arises
from the vertebral artery. The basilar artery has one more branch called the labyrinthine artery supplying
the inner ear. (Branches of the basilar artery is a frequently asked question).
The vertebral artery gives the anterior spinal artery (by two roots), the two posterior spinal arteries, and
the inferior posterior cerebellar artery (for the cerebellum and the choroid plexus of the fourth ventricle).
109
DURAL SINUSES
The dura mater has one layer in the skull, called the dura mater encephali, surrounding the entire brain.
It forms a double layer between the two hemispheres called the falx cerebri. The falx cerebri starts from the
crista galli anteriorly and is attached to the internal occipital protuberance posteriorly. In the superior
border is a sinus (the main venous sinus of the brain) called the superior sagittal sinus. This sinus flows into
the confluens sinuum at the level of the internal occipital protuberance.
In the inferior margin of the falx is the inferior sagittal sinus, found above the corpus callosum. This
sinus continues into the straight sinus (sinus rectus) which runs between the falx cerebri and tentorium
cerebelli.
The tentorium cerebelli is another double layer, separating the cerebellum from the occipital lobe. It is
attached to the superior border of the pyramidal bone and along the sulcus sinus transversi. In the midline,
it has an opening called insisura tentorii for the brain stem.
There is another small sinus in the posterior margin of the falx cerebelli because between the two
cerebellar hemispheres is another tiny falx. This sinus also drains into the confluence.
These sinuses are the so-called inflowing sinuses of the brain. The outflowing sinuses (which drain the
blood from the confluens sinuum) are the transverse sinuses which continue into the sigmoid sinus and from
there into the internal jugular vein.
These dural sinuses are visible on the dural cap. In addition, there are the sinus cavernosus, superior
and inferior petros sinuses, and the sphenoparietal sinus. To see these sinuses, the brain must be removed.
All these sinuses should be mentioned in the exam.
SINUSES IN THE BASE OF THE SKULL
The most important sinus in the base of the skull is the SINUS CAVERNOSUS, located at the two sides of
the sella turcica. The double layer of the dura mater divides, surrounding this sinus. It has medial and
lateral lamina. The medial lamina is attached to the body of the sphenoid bone, and the lateral lamina is
between the anterior and posterior clinoid processes. The lateral and medial walls are continuations of the
tentorium cerebelle. The free border of the tentorium cerebelle forms the tentorial notch and continues into
the lateral wall of the cavernous sinus. The part of the tentorium which is attached to the superior border of
the pyramidal bone continues into the medial wall of the cavernous sinus. So, the two parts cross each other
before forming the lateral and medial laminae of the cavernous sinus.
Through the cavernous sinus, the following structures pass:
Internal carotid artery (the most medial structure– here is a curvature called carotid siphon)
Oculomotor nerve (next to the internal carotid artery)
Trochlear nerve (lateral to and behind the oculomotor)
Ophthalmic nerve (more lateral)
Abducent nerve (it comes from behind).
The last four structures enter the superior orbital fissure and the orbital cavity. Any infection or
thrombosis in the cavernous sinus may result in paralysis of the eye.
The two cavernous sinuses are connected by the anterior and posterior intercavernous sinuses, found
anterior and posterior to the pituitary gland. This creates a venous circle around the pituitary gland.
The inflowing sinuses of the cavernous sinus are the sphenoparietal sinus, running along the posterior
edge of the ala minor, and the superior ophthalmic vein.
The outflowing sinuses of the cavernous sinus are the superior and inferior petrous sinuses. The
superior takes the blood between the transverse and sigmoid sinuses. The inferior takes the blood into the
sigmoid sinus.
There are superior cerebral veins (from the outer surface of the hemispheres) which run into the superior
sagittal sinus. There are inferior cerebral veins which drain into the sinus cavernosus. The largest of these
is the superficial cerebral vein, running in the sulcus lateralis cerebri.
110
There are also the basal veins of Rosenthal running at the lateral side of the hypothalamus and
mesencephalon on the basal surface of the brain stem and hypothalamus. Basal veins are drained into the
sinus rectus.
The cerebellar veins drain to the sinus rectus.
The most important vein of the brain is the vena cerebri magna which drains below the splenium corpori
calosi and comes from the two internal cerebral veins. The two internal cerebral veins arise from the
thalamostriate vein, choroid vein (from lateral and third ventricles), vena septi pellucidi.
The thalamostriate vein, veins of the choroid plexi, and the vena cerebri magna and interni are visible in
the brain.
CIRCULATION OF CEREBROSPINAL FLUID
Cerebrospinal fluid is produced by the choroid plexi of the ventricles. The main source is the plexus of
the lateral ventricle. From the lateral ventricle, the liquid circulates into the third ventricle through the
interventricular foramen of Monro. From the third ventricle, it circulates to the aqueductus cerebri of the
mesencephalon. From there, to the fourth ventricle (there is also choroid plexus here) and from the fourth
ventricle, it circulates out into the outer liquor space. Thus, there is an inner space for the liquor (ventricles)
and an outer space (outside the brain, in the subarachnoid space). Fluid is produced in the ventricles and
absorbed from the outer space.
The openings from the fourth ventricle to the subarachnoid space are the Luschka openings or the lateral
apertures of the fourth ventricle (apertura lateralis ventriculi quarti). The median opening is called the
apertura mediani ventriculi quarti (or the Magendi foramen). Through these foramina, the cerebrospinal
fluid circulates from the fourth ventricle into the subarachnoid space and into the cisternae (dilations in the
space). The Magendi foramen opens into the cisterna magna between the cerebellum and the medulla (also
called the cisterna cerebellomedullaris). The Luschka foramina open into the cisterna ambiens.
From the cisternae of the subarachnoid space, the fluid circulates onto the entire surface of the brain and
downward onto the spinal cord (still in the subarachnoid space). The fluid flows down the dorsal surface of
the spinal cord, circulates between the denticulate ligaments, and recirculates upward toward the brain. It is
a very slow fluid circulation, providing protection for the CNS.
If this circulation is blocked (for example, by a pressure on the medulla), the pressure inside the skull
(and therefore inside the ventricles) will increase.
The absorption of this fluid is done by the arachnoid villi. The arachnoid membrane has granulations
with villi on the surface, located in the subarachnoid space. These villi absorb the fluid from the space into
the sinuses (venous blood). Most of the granulations are along side the sinus sagittalis superioris, the main
drainage of the cerebrospinal fluid.
CONVEX SURFACE OF THE CEREBRUM
The best starting point is the central sulcus. The central sulcus is a transverse sulcus on the parietal
lobe. It is bordered by anterior and posterior transversely running gyri called precentral and postcentral gyri
respectively. The postcentral gyrus is the main ("primary") sensory cortex. The precentral gyrus is the
main motor cortex (giving rise to the fibers of the pyramidal tract). The central sulcus also separates the
frontal lobe from the parietal lobe, thus placing the two gyri in different lobes.
FRONTAL LOBE: In front of the precentral gyrus, longitudinal fissures (ant. to post.) separate the frontal
gyri from each other. These are the superior frontal sulcus (separating the superior and middle frontal gyri)
and the inferior frontal sulcus (separating the middle and inferior frontal gyri). The inferior frontal gyrus
can be further divided. In front is a triangular-shaped area called pars triangularis. Behind this is the pars
opercularis which covers the insula (like the "operculum" covering the gills of a fish).
111
On the basal surface of the frontal lobe, the longitudinal fissure lies in the midline, dividing the cerebral
hemispheres. From the midline going laterally: the straight gyrus (gyrus rectus), the olfactory tract, and
the orbital gyri (above the orbit).
PARIETAL LOBE: The lobus parietalis has a sulcus in the middle called the sulcus intraparietalis,
running anterior to posterior. It separates the superior and inferior parietal lobules. The inferior parietal
lobule has two parts: the supramarginal gyrus and the angular gyrus. The supramarginal gyrus can be found
easily by placing a finger into the sulcus lateralis cerebri the gyrus will slip around the finger. By placing
the finger into the superior temporal sulcus, the angular gyrus will slip around it.
On the medial surface of the brain is the precuneus which belongs to the parietal lobe. The precentral
lobule lies in front. The precentral lobule belongs to both the frontal and parietal lobes. It slips around a
finger placed in the central sulcus.
OCCIPITAL LOBE: The occipital lobe is separated from the parietal lobe by the parietooccipital sulcus.
It can be found in the medial surface of the brain by moving apart the occipital and parietal gyri. It is the
only deep sulcus visible on the medial surface of the brain. This sulcus is joined by another sulcus called
the sulcus calcarinus, surrounding triangular area called the cuneus. The cuneus belongs to the occipital
lobe. The calcarine sulcus is near the main visual cortex.
The gyri of the occipital lobe on the convex surface are just called the occipital gyri.
TEMPORAL LOBE: The temporal lobe is separated from the parietal and frontal lobes by the sulcus
lateralis cerebri. There are three sulci inside the lobe, separating it into three temporal gyri. The superior
temporal sulcus separates the superior and middle temporal gyri. The middle temporal sulcus separates the
middle and inferior temporal gyri. The inferior temporal sulcus separates the inferior temporal and
occipitotemporal gyri (the latter belonging both to the occipital and temporal lobes).
There is another sulcus on the basal surface of the brain called the collateral sulcus, separating the
occipitotemporal and parahippocampal gyri. Finally, the parahippocampal gyrus is separated from the brain
stem by the sulcus hippocampi. In front of the parahippocampal gyrus is an angle-like structure called the
UNCUS. There is another gyrus called the cingulate gyrus which belongs to the limbic system, together with
the uncus. This gyrus surrounds the corpus callosum.
VENTRICLES
There are four ventricles. The first and second are called the lateral ventricles because they are
symmetrical and equal. Between them (in the midline) is the third ventricle. The interventricular foramen
(Monro's foramen) forms a communication between the lateral ventricles and the third ventricle. The third
ventricle continues into the cavity of the mesencephalon, the aqueductus cerebri. This, in turn, continues to
the fourth ventricle, the cavity of the rhombencephalon.
LATERAL VENTRICLE
The lateral ventricle is the cavity of the telencephalon (cerebral hemispheres). It has an anterior horn
in the frontal lobe, a central part in the parietal lobe, a posterior horn in the occipital lobe, and an inferior
horn in the temporal lobe.
First, the temporal and parietal lobes develop as a single horn which forms an elongation from anterior to
posterior. The frontal and occipital lobes develop secondarily. This difference is reflected in the presence
or absence of choroid plexus. Choroid plexus is found in the regions of primary lobe development (central
part and inferior horn) but not in the regions of secondary development (anterior and posterior horns).
The walls of the anterior horn are:
MEDIAL WALL: Septum pellucidum (separating the two anterior horns from each other).
LATERAL WALL: Caput nuclei caudati.
112
ANTERIOR & SUPERIOR: Forceps (anterior fibers) of the corpus callosum.
The anterior horn continues posteriorly into the central part. The borderline between them is the
foramen interventriculare Monroi. This foramen is between the columna fornicis and the thalamus. The
fornix starts from the hippocampus and terminates in the mamillary bodies. This pathway has the two crura
behind, coming from the two hippocampus. These two crura join each other, forming the corpus on the
thalamus (on its dorsal surface). Then, the corpus divides into two columns anteriorly (columna fornicis),
terminating inferiorly to the mamillary bodies. The fornix is an associated pathway connecting the
hippocampus with the mamillary body, called the Papez circle. The portion of the fornix descending in
front of the thalamus surrounds the foramen. Thus, we can say that the anterior border is the columna
fornicis and the inferoposterior border is the thalamus.
The central part is posterior to the anterior horn. The lateral wall of the central part is the body of the
caudate nucleus (corpus nuclei caudati). The floor is the dorsal surface of the thalamus which is layered by
the lamina affixa (single epithelial layer belonging to the telencephalon vesicle) where the diencephalon and
telencephalon are connected. The medial wall is the body of the fornix. The superior wall is the corpus
callosum.
The choroid plexus attaches to the thalamus by the tenia choroidea (a "tenia" is the torn edge of cerebral
wall which remains when a plexus is removed). The other attachment of the choroid plexus is the limb of
the fornix (tenia fornicis). Between these attachments is the choroid plexus inside the lateral ventricle.
The teniae can be seen by moving it out of the way.
The calcarine sulcus is adjacent to the visual cortex (Brodmman 17-18).
The central part divides to form the posterior and inferior horns. The inferior wall of the posterior horn
is the trigonum collaterale (a triangular shaped emminence formed by the collateral sulcus aka. "collateral
emminence"). The superior and lateral walls are formed by the corpus callosum.
The collateral emminence continues to form the lateral part of the floor of the inferior horn. The medial
part of the floor is a large elevation called the hippocampus. The hippocampus has the pes hippocampi in
front and the fimbria hippocampi behind. The fimbria hippocampi is the beginning of the fornix. The
tenia (tenia fornicis in the central part) continues down into the inferior horn to form the tenia fimbriae on the
fimbria hippocampi.
The tenia choroidea (in the central part of the thalamus) also continues into the inferior horn, being on the
superior wall of the inferior horn on the striae terminalis. Here, it is called the tenia terminalis.
The lateral wall of the inferior horn is the tapetum, a bundle of fibers from the corpus callosum which
descend to the temporal lobe, covering the inferior horn laterally.
THIRD VENTRICLE
This is the cavity of the diencephalon. The superior wall is the tela choroida ventriculi tertii which
forms a plexus and forms attachments to the thalamus, called the tenia thalami.
There is a surface which doesn't belong to any ventricle and is therefore called the extraventricular
surface. The fornix is located on this surface, and if removed, you will see this stripe.
The lateral wall is the medial surface of the thalamus. The inferior wall is the hypothalamus. Between
them is the hypothalamic sulcus (visible on the median sagittal section of the brain). It begins at the
foramen Monroi and terminates in the aqueductus cerebri. The hypothalamus is located below this sulcus.
Inside are the parvocellular and magnocellular nuclei.
The anterior wall is formed by the lamina terminalis the original anterior wall of the prosencephalon
vesicle. All the structures lying in front of this vesicle belong to the telencephalon. Between the two
hemispheres is a commissural pathway called the anterior commisure. Above this commissure is the
triangular recess of the anterior wall.
The columna fornicis continues into the mamillary body, into the hypothalamus (pars recta) and a little
laterally (not a midline structure).
Posteriorly, it continues into the aqueductus cerebri. Above the aqueduct, the posterior wall is
surrounded by the epithalamic structures. The commissura posterior cerebri lies above the aqueduct, and
above this commissura is the commissura habenularum (connecting the two habenulae). Above this is the
pineal recess, then the lamina epithelialis (attached to the habenulae). It continues to the other side, tenia
113
thalami, through the commissura habenularum. Between the epithelial lamina (between the choroid tela of
the third ventricle and the pineal gland) is the supra-pineal recess.
There are two recesses in the inferior wall. The anterior one is the opticopreoptic recess in front of the
optic chiasma, between the lamina terminalis and optic chiasma. The second one is the infundibular recess,
found behind the optic chiasma in the pituitary stalk.
FOURTH VENTRICLE
This is the cavity of the rhombencephalon. This ventricle is something like a tent. It has a base
(rhomboid fossa); superior, anterior, cranial wall (velum medullare superior); inferior part of the roof (velum
medullare inferior). Between the two veli is the fastigium (upper sharp angle). Below the v.m.inferior, the
epithelial lamina of the choroid plexus forms the wall of the fourth ventricle. On this tela, there is an
opening (in the midline) called the Magendie foramen (apertura mediana ventriculi quarti). This foramen
opens into the cerebellomedular cistern (or cysterna magna).
The cerebellum covers the fourth ventricle superiorly. The floor is the rhomboid fossa.
RHOMBOID FOSSA: It is bordered anteriorly by the pedunculus cerebellaris superior. There are three
cerebellar peduncles, connecting the mesencephalon (superior), pons (middle), and medulla (inferior) to the
cerebellum.
The inferior or caudal two walls of the rhombus are the teniae of the choroid plexus. This tenia starts
from the obex and runs through the pedunculus cerebellaris inferior (continuation of funiculus lateralis).
Here, the tenia continues into the pedunculus flocculi and to the vellum medullare inferioris. The fossa is
formed by the dorsal surface of the pons and the dorsal surface of the medulla.
Inferior triangle: In the midline is the sulcus medianus. It separates the fossa into two symmetric
triangles. The superior triangle belongs to the pons. The inferior triangle belongs to the medulla (open
part).
Lateral to the sulcus medianus is the emminentia medialis. Lateral to the emminence is the sulcus
limitans. The two triangles are separated from each other (pons and medulla) by the striae medullare (also
called striae acusticae, for the pathway belonging to the acoustic system). In the inferior triangle, next to
the midline, the hypoglossal triangles overlie the motor nuclei of the hypoglossal nerves.
Lateral to the trigonum nervi hypoglosi lie the trigonum nervi vagi or the dorsal nucleus of the vagus
nerve or medial ala cinerea. This is the vegetative nucleus of the vagus nerve which innervates the
abdominal organs (preganglionic fibers). The vagus has another vegetative nucleus (ventral).
The area postrema (chemical vomiting center) is lateral to the trigonum nervi vagi.
Superior triangle: Right above the striae medullaris is the colliculus facialis (nucleus of the abducens
nerve). Because the fibers originating from the facial nucleus hook around the abducens, this elevation is
called the facial collicle (internal genu of the facial nerve). The external genu of the facial nerve is in the
pyramis.
Above and lateral to this is the locus ceruleus (meaning "blue" because the neurons are pigmented here).
At the level of the locus ceruleus is the trigeminal nuclei. The medial one is the motor nucleus, and the
lateral nucleus is the principle sensory nucleus.
The lateral recess is called the vestibular recess because the vestibular nuclei (Bechterew-superior;
Schwalbe-medial; Deiters-lateral; and the inferior), giving rise to the vestibular nerve, are found here.
In the inferior cerebellar peduncle, there are two nuclei belonging to the cochlear nerve-- anterior and
posterior-- both sensory. The vestibulocochlear nerve is the only pure sensory cranial nerve. The olfactory
and optic "nerves" are also sensory, but they are not true cranial nerves, just pathways.
FLECHSIG'S CUT
This is an oblique cut of the hemisphere. This cut is made from the corpus callosum to the sulcus
lateralis cerebri with the knife at a 45 angle. If the top half of the hemisphere has been removed (to dissect
114
the lateral ventricle), we can place the knife directly on the corpus callosum. Otherwise, the cut must be
made from the sulcus.
This cut is used to show the basal ganglia (the main subcortical nuclei belonging to the telencephalon).
These are the nucleus caudatus, nucleus lentiformis, and the claustrum. The thalamus is also visible with
this cut, but it belongs to the diencephalon, not to the basal ganglia. Between these nuclei are three whitematter structures called the internal, external, and extreme capsules.
The internal capsule is a "V"-shaped tract between the thalamus, caudate nucleus, and lentiform nucleus.
It has an anterior crus, a posterior crus, and a genu. The anterior crus is between the caudate nucleus and
the lentiform nucleus. The posterior crus is between the thalamus and lentiform nucleus.
The internal capsule contains the projecting fibers (ascending and descending). The ascending fibers
terminate in the cortex, and the descending fibers arise from the cortex. Thus, these are the "long fibers".
Lateral to the lentiform nucleus is the claustrum, a mass of grey matter surrounded by white matter
("claustrum" means a closed structure). Lateral to the claustrum is the cortex of the insula. Between the
lentiform nucleus and the claustrum is the external capsule, while the extreme capsule is between the
claustrum and the insula.
TRACTS OF THE INTERNAL CAPSULE
In the anterior limb is a descending tract called the Arnold tract (or tractus frontopontinus). This tract
originates from the frontal cortex and terminates on the pontine nuclei. Another tract, the pontocerebellar
tract, starts from the pontine nuclei and crosses through the midline on its way to the cerebellum. In this
way, one hemisphere (one cerebral cortex) communicates with the contralateral cerebellar cortex).
In the posterior limb, the Türck tract carries fibers from the parietal-temporal and occipital cortex down
to the pontine nuclei (therefore, another name for the tract is the parietotemporo-occipitopontine tract; the
three lobes may be named in different orders in different books and sets of notes). Thus, all cortical regions
have tracts to the pontine nuclei. The Arnold and Türck tracts are collectively known as corticopontine
tracts. Both tracts are descending.
There is another important descending tract in the anterior limb, close to the genu. This is the combined
corticomesencephalic and corticobulbar tracts, or the corticonuclear tract. This is the upper part of the
pyramidal tract. The fibers which originate from the motor cortex descend to the different parts of the brain
stem, terminating on the motor nuclei of the cranial nerves. The shortest fibers are anterior, and the longest
fibers are posterior. The shortest fibers terminate on the oculomotor nuclei (in the mesencephalon).
Posteriorly, they terminate on cranial nerves IV-XII.
The motor nuclei of the cranial nerves receive the supranuclear fibers. This tract is called the
corticonuclear tract, belonging to the pyramidal tract.
Behind the corticonuclear tract (in the genu and posterior limb) is the corticospinal tract. The shorter
fibers are anterior and the longer fibers are posterior. The anterior fibers terminate on the cervical part of
the spinal cord (on the motor neurons).
Ascending tracts from the thalamus (the main relay of ascending pathways) to the cerebral cortex are
collectively called the thalamocortical fibers (or the thalamocortical radiation). This has different parts
("peduncles" or "radiations") running to the different lobes. In the anterior limb, just posterior to Arnold's
tract, the ANTERIOR THALAMIC RADIATION (peduncle) carries fibers from the thalamus to the frontal lobe.
From the thalamus, all sensory tracts ascend to the sensory cortex. Pain fibers go mainly to the frontal
cortex, and all other sensory fibers go to the postcentral gyrus (main-primary sensory cortex) and to the
secondary sensory cortex.
Important ascending tracts of the posterior limb are the POSTERIOR THALAMIC RADIATION (in the
retrolentiform area) and the MIDDLE THALAMIC RADIATION. The SUPERIOR THALAMIC RADIATION, ascending to
the parietal cortex, is more anterior, closer to the genu. The INFERIOR THALAMIC RADIATION is in the
sublentiform part (so can't be seen in this cut) and runs to the temporal cortex. As with the anterior thalamic
radiation, the sensory fibers from the thalamus ascend to the postcentral gyrus and the secondary sensory
cortex. These sensory fibers are also called the thalamic peduncle.
There are two additional sensory tracts in the posterior limb: the RADIATIO ACUSTICA and the RADIATIO
OPTICA. The optic radiation runs backward to the calcarine fissure of the occipital lobe (Brodmman's 1718), the main visual cortex. The acoustic radiation terminates lateral to the temporal cortex in the superior
115
temporal gyrus (or operculum temporale that part of the superior temporal gyrus that covers the insula). It
has transverse gyri called Hescle gyri (not so important).
Different sources assign different relationships betweent the posterior thalamic radiation and the optic radiaiton as they both run
to the occipital cortex. They might be described as separate, identical, different but overlapping, or that
the optic is a subportion of the posterior. The same may be said of the inferior thalamic radiation and the acoustic ra
diation, as they both run to the temporal lobe. Ask your lab instrictor for clarity here.
Ask also about the "middle thalamic
radiation"- it doesn't appear in many sources.
The blood supply of the internal capsule and basal ganglia is given by the middle cerebral artery.
The anterior limb of the internal capsule has the grey striations. They connect the caudate nucleus to the
lentiform nucleus. The caudate nucleus, lentiform nucleus, and grey striations (through the internal capsule)
are called the striate body (corpus striatum).
THALAMUS
Macroscopic description. It is the main nucleus derived from the diencephalon. It has medial, dorsal,
lateral, inferior, and anterior surfaces. The MEDIAL SURFACE forms the lateral wall of the third ventricle.
The DORSAL SURFACE has two parts: lateroventricular surface, forming the floor of the central part of the
lateral ventricle (layered by the lamina affixa), extraventricular surface, not belonging to any ventricle
(covered by the fornix). The LATERAL SURFACE forms the medial wall of the internal capsule. The
INFERIOR SURFACE is attached to the hypothalamus (the borderline is the sulcus hypothalamicus). The
ANTERIOR SURFACE is related to the head of the caudate nucleus and to the columna fornicis (between them,
the lamina terminalis). Between the thalamus and columna fornicis is an opening called Monro's foramen
(the opening where the telencephalic vesicles evaginated from the prosencephalon). The caudate nucleus is
located on the dorsolateral surface. Between them is a sulcus called the stria terminalis (having the
thalamostriate vena terminalis). The stria terminalis is not just for the vein. There is also a tract called
stria terminalis, connecting the amygdaloid nucleus with the hypothalamus (the stria terminalis belongs to
the limbic system).
There are two teniae ("band-like" structures) on the thalamus: the tenia choroidea (attachment of the
choroid plexus) and the tenia thalami (attachment of the epithelial roof of the third ventricle). Between
these two is the extraventricular surface. From a superior view, the stria terminalis is the most lateral, then
the lamina affixa, the tenia choroidea, and the tenia thalami. The tenia thalami has a pathway called the
stria medullaris (also belonging to the limbic system). The hypothalamic nuclei are connected with the
habenular nuclei by this pathway.
Microscopic structure. The thalamus has three main parts: anterior, medial, and lateral. They are
separated by a Y-shaped white matter called the lamina medullari (internal medullary lamina). .
The
ANTERIOR PART contains the anterior thalamic nuclei, the termination of the mamillothalamic tract. The
corpus mamillare receives the fornix, and from the mamillary bodies, the mamillothalamic tract terminates in
the anterior nucleus. This tract belongs to the limbic system (as do the fornix and hippocampus).
The largest nuclei of the MEDIAL GROUP are the dorsomedial nucleus, the centrum medianum, and the
parafascicular nucleus. The dorsomedial nucleus receives pain sensory fibers from the mesencephalon
through the spinothalamic tract and trigeminal lemniscus. The pain sensory fibers of the spinothalamic
tract and medial lemniscus leave the tract at the level of the mesencephalon, and some fibers terminate in the
central grey of the mesencephalon. From the central grey, they run through the hypothalamus to the
dorsomedial nucleus or to the centrum medianum and the other intralaminar nuclei of the thalamus. The
pain sensory fibers ascend to the frontal cortex through the anterior limb of the internal capsule.
The LATERAL PART can be divided into posterior, dorsal (or simply "lateral"), and ventral groups. The
posterior group is the pulvinar thalami (visible macroscopically as the lateral posterior nucleus). The dorsal
group includes the lateral dorsal and lateral posterior nuclei. These three nuclei don't have subcortical
connections. They are connected just with the cortex (afferent and efferent connections).
The ventral group has three nuclei. Anteriorly, there are ventral anterior (VA) and ventral
lateral (VL) nuclei. They belong to the extrapyramidal system (the main anatomical structure of the
116
extrapyramidal system is the basal ganglia). As the efferent pathway from the globus pallidus terminates in
the VA nucleus, the VL nucleus is the main termination of the extrapyramidal system and the cerebellar
system. From the VA-VL, the efferent pathway terminates in the motor cortex. Thus, both the cerebellum
and the basal ganglia influence the motor cortex. Posteriorly, the ventral posterior nucleus can be further
subdivided. The VPL and VPM (ventral posterolateral and ventral posteromedial) are very important relay
nuclei of the sensory pathways (spinothalamic - medial lemniscus - trigeminal lemniscus). The VPM
receives fibers from the trigeminal lemniscus (mainly from the face), and the VPL receives fibers from the
medial lemniscus and spinothalamic tract.
HYPOTHALAMUS
The hypothalamus develops from the diencephalon and is located below the thalamus. The basal
surface of the brain shows the hypothalamus behind the optic chiasma. The two main structures are the
tuber cinereum and the mamillary bodies. Superiorly, the hypothalamus has the hypothalamic sulcus,
connecting the foramen Monroi to the aqueductus cerebri.
There are anterior, middle, and posterior nuclei. Another method of classification divides the nuclei into
magnocellular and parvocellular nuclei. The anterior group has the suprachiasmatic nucleus and the
preoptic area (sometimes called the preoptic nucleus). The middle group has medial and lateral nuclei.
The medial nuclei are the arcuate nucleus (or infundibular nucleus, as it surrounds the infundibulum on both
sides), the ventromedial nucleus, and the dorsomedial nucleus. The lateral area of the middle group is
called the lateral area of the hypothalamus.
Between the anterior and middle group, there are two magnocellular nuclei the paraventricuclar and
supraoptic nuclei. Some books lists them among the middle group. They produce vasopressin and
oxytocin.
The posterior group has the posterior nucleus and the mamillary body.
The hypothalamus has many different functions. It is related to the limbic system through the fornix
(mamillary bodies, hippocampus). It is also connected with the amygdaloid body through the stria
terminalis and through the amygdalofusal pathways. It is connected with the habenular nuclei through the
stria medullaris.
It is related to the olfactory system (receiving afferentation) through the medial forebrain bundle that
connects the medial forebrain (the area of the anterior perforating substance + the area superodorsal to it until
the anterior commissure). For the medial forebrain, the medial forebrain bundle passes through the
hypothalamus and makes afferentation for the hypothalamus and connects it with the olfactory system.
The suprachiasmatic nucleus receives afferentation from the retina. This way, some light and dark
stimuli influence the endocrine system. It also receives afferentation through the spinothalamic tract (painsensory) and gives efferentation to the dorsomedial nucleus of the thalamus.
The hypothalamus has a very wide variety of afferentation, but olfactory, limbic, and visual systems are
the most important.
Limbic system. This is the ancient cortex (the paleocortex). It has four layers. The structures
belonging to the limbic system are the hippocampus, parahippocampal gyrus, uncus, dentate gyrus, cingulate
gyrus, stria terminalis, fornix, and the amygdaloid nucleus complex. In humans, the olfactory cortex is the
uncus of the parahippocampal gyrus, the amygdaloid system, plus the substantia perforanta anterior. The
secondary olfactory system is the orbital gyri.
Efferentation. The mamillothalamic tract and the mamillotegmental tract (descending to the tegmentum of the mesencephalon) originate from the mamillary bodies.
In the posterior and lateral hypothalamic areas, there are the sleeping center, drinking center, and the
eating center (all are vegetative centers). These centers influence the vegetative functions through the
117
descending pathways (ex: fasciculus longitudinalis dorsalis) terminating on the vegetative nuclei of the
spinal nerves. Some tracts terminate on these nuclei through the reticular formation.
ENDOCRINE SYSTEM
The main function of the hypothalamus is to regulate the endocrine glands.
There are parvocellular and magnocellular nuclei. The magnocellular nuclei are the supraoptic and
paraventricular nuclei, producing vasopressin and oxytocin. These hormones are transported to the
posterior lobe of the pituitary through the supraopticoparaventriculohypophyseal tract, along side the axon
fibers with some carrier molecules. These hormones are released into the blood vessels of the posterior
pituitary and are stored there. Vasopressin, also called anti-diuretic hormone (ADH), allows the
hypothalamus to regulate the water reabsorption from the distal nephron of the kidney. The name
vasopressin comes from its effect of increasing the blood pressure.
Oxytocin causes contraction of the smooth muscle of the uterus and the myoepithelial cells of the
mammary glands. This assists delivery of the baby by contraction of the uterus. Oxytocin can be given by
injection if the patient's production is insufficient. The excretion of the milk after delivery is also under the
effect of oxytocin. The production of the milk itself is stimulated by prolactin.
This process of neuron cell bodies secreting hormones is called neurosecretion. This is done by
supraoptic and paraventricular nuclei plus the parvocellular group. The releasing and inhibiting hormones
exert their effect on the trophic hormones through the portal system. The tract that comes from the
parvocellular nuclei and terminates on the blood vessels of the pituitary stalk is called the tuberoinfundibular
tract. These hormones will be released into the capillaries of the pituitary stalk which come from the
superior hypophyseal artery. These capillaries are very coiled and are collected into the portal vein.
These portal veins form the sinusoids of the pituitary gland (adenohypophysis).
The hormones produced by the parvocellular cells act at the level of the pituitary cells which produce the
trophic hormones (LH, FSH, GH, prolactin, TSH, ACTH). Both the synthesis and release of these trophic
hormones are regulated by the releasing hormones (LHRH, TRH, ACTH, GHRH, Somatostatin) through the
portal system. These hormones are found in high concentration in the portal capillaries, but not in the
periphery.
There is a feedback connection between the hormones produced by the target glands and the
hypothalamus. If the level of the hormones produced by the thyroid gland or ovary is too high, the high
hormone levels act on the hypothalamus by a negative feedback system to decrease the level of the releasing
hormones. But, they also act at the level of the pituitary by a negative or positive feedback (if the peripheral
level is too low).
BRAIN STEM
CRANIAL NERVES
The first cranial nerve is the olfactory nerve (not a real cranial nerve, but just a pathway located on the
surface of the brain). The bulbus olfactorius is taken as the exit of the nerve. The exit from the skull is
through the lamina cribrosa.
The optic nerve is also a pathway. The exit from the brain is the optic chiasma, and the exit from the
skull is the optic canal. The tract is inside the brain, and the nerve is outside.
The oculomotor nerve comes out from the brain through the interpeduncular fossa (mesencephalon).
The interpeduncular fossa is between the two crus cerebri.
The trochlear nerve is the only nerve that comes out from the dorsal surface of the brain, lateral to the
frenulum veli medullaris superius.
118
The trigeminal nerve exits between the pons and the brachium pontis, in front of the brachium. The
pons is connected laterally to the cerebellum. This connection resembles a bridge (ponts). The trigeminal
nerve has two roots: sensory and motor.
The abducent nerve exits between the pons and the medulla, or between the pons and the pyramids.
The facial nerve and glossopharyngeal nerve exit between the pons and medulla and the cerebellum
(pontocerebellar angle).
The glossopharyngeal, vagus, and accessory nerves exit through the sulcus paraolivaris lateralis.
The hypoglossal nerve exits through the medial paraolivaris sulcus.
The accessory nerve has a cranial origin and a spinal origin. The spinal origin comes from the upper
four cervical segments, ascends in the foramen magnum into the skull, and joins the cranial origin. The two
together leave the skull through the jugular foramen.
At the inferior level of the medulla is the decussation of the pyramidal tract. 90% of the fibers cross
each other, then run down the lateral column. The other 10% of the fibers remain in the anterior column.
The brain stem has three main parts: 1) Medulla, 2) Pons, 3)Mesencephalon.
MEDULLA
This is the continuation of the spinal cord above the foramen magnum. It has two main parts: an open
(cranial) part and a closed (caudal) part. The open part is so named because it communicates with the fourth
ventricle, while the closed part communicates with the central canal.
Ventral surface. On the anterior surface of the medulla oblongata, there is a deep fissure which is
continuous with the anterior median fissure of the spinal cord. Lateral to this fissure is the pyramis
medullae oblongatae, a pyramid-shaped structure. This contains the corticospinal tract. There are fibers
crossing the midline which form the pyramidal decussation. 90% of the fibers decussate here while the
remaining 10% descend uncrossed. Lateral to the pyramis is an oval shaped structure called the olive.
Inside is the inferior olivary nucleus. Medial to the olive (between it and the pyramis) is the medial
paraolivary sulcus (exit of the XII cranial nerve). Lateral to the olive is the lateral paraolivary sulcus (exit
of IX, X, XI cranial nerves). Lateral to the lateral sulcus is the inferior cerebellar peduncle, the continuation
of the lateral column of the spinal cord. This peduncle takes the ventral spinocerebellar and olivocerebellar
tracts to the cerebellum. The ascending fibers to the cerebellum are running inside the inferior cerebellar
peduncle to the cerebellum.
Dorsal surface. The dorsal surface of the medulla has a midline sulcus called the sulcus medianus
posterior, the continuation of the sulcus from the spinal cord. There are two tubercles lateral to the sulcus:
tuberculum nuclei gracilis (medial) and tuberculum nuclei cuneati (lateral). These tubercles are formed by
the nuclei of the same name, and the nuclei are the termination of the posterior column. Lateral to the
tuberculum nuclei cuneati is the funiculus lateralis which continues into the inferior cerebellar peduncle.
The open part of the medulla has the rhomboid fossa. The inferior triangle of the rhomboid fossa
belongs to the medulla. The inferior angle of the rhomboid fossa is the obex. Two teniae run from the
obex to the lateral recess, and these are the teniae choroidea ventriculi quarti. Above the obex is the
midline sulcus medianus (see "Fourth Ventricle").
Microscopic structures. On the dorsal surface are the Goll and Burdach nuclei. The tract arising
from these two is called the medial lemniscus. These fibers cross over the midline to form the decussatio
lemniscorum. The fibers then ascend into the thalamus (ventral posterolateral nucleus). The grey matter is
a little different from the grey matter of the spinal cord because the dorsal horns are located ventrally. The
original ventral and dorsal horns are more lateral and medial here. The ventral horn develops from the basal
plate, and the dorsal horn from the alar plate of the neural tube. Between them is the sulcus limitans.
The motor nuclei of cranial nerves XI and XII are found in the ventral horn. The hypoglossal nucleus is
in the dorsomedial motor column, and the accessory nucleus is in the ventrolateral motor column. So, in the
original ventral horn, the two nuclei are separated from each other by the lemniscal decussation and by he
119
pyramidal decussation. These nuclei form a column in the brain stem. The nuclei belonging to these
motor columns are the mixed cranial nerves (ventrolateral) which supply the branchial arches and the pure
motor cranial nerves (dorsomedial). The motor nucleus of the medulla giving fibers to the
glossopharyngeal, vagus, and accessory nerves is called the nucleus ambiguus. In the dorsomedial motor
column is the hypoglossal nucleus. More superior in this column (in the pons) is the motor nucleus of the
abducent nerve. In the mesencephalon, the dorsomedial motor column forms the trochlear and oculomotor
nuclei.
There is an exception in each of these groups. The oculomotor nerve is not a pure motor nerve, as it has
a vegetative nucleus as well. The trigeminal nerve does not have one.
There is a sensory nucleus in the dorsal horn called the nucleus tractus spinalis nervi trigemini (sensory
nucleus of CN V, IX, X). It is called spinal because it is the continuation of the substantia gelatinosa of the
spinal cord. It receives the termination of the pain and temperature fibers of the substantia gelatinosa.
These fibers originate in the face (trigeminal area) and other areas.
The fibers which terminate in this nucleus run in a tract lateral to it: the tractus spinalis nervi trigemini.
These are descending fibers because the trigeminal nerve enters the brain between the pons and brachium
ponti. The nucleus is located in the medulla, so the fibers must descend from the pons to the medulla.
There is another nucleus dorsal to the central canal called the nucleus tractus solitarii (special
viscerosensory nucleus of the mixed cranial nerves-- VII, IX, X).
There is another nucleus in the anterior part of the medulla, lateral to the pyramis, called the inferior
olivary nucleus. A tract starts from this nucleus called the olivocerebellar tract (the most important
afferentation for the cerebellum). The nucleus receives afferentation from the spinal cord (spinoolivary
tract) and from the nucleus ruber and thalamus through the fasciculus tegmentalis centralis.
The tracts pass through the medulla oblongata and the spinal cord. The pyramidal tract is anterior, the
spinothalamic tract is lateral to the olivary nucleus. Anterior spinocerebellar tract (Gower's tract), posterior
spinocerebellar tract (Flechsig's tract).
The open part of the medulla opens into the fourth ventricle. The floor of the fourth ventricle is the
rhomboid fossa. Next to the midline is the trigonum nervi hypoglossi (motor nucleus of the hypoglossal
nerve-- dorsomedial motor column). Lateral to this is the trigonum nervi vagi (one of the vegetative nuclei
of the vagus nerve). This nucleus gives the preganglionic fibers to the abdominal organs. It is also called
the dorsal nucleus of the vagus. The ventral nucleus of the vagus is located dorsolateral to the nucleus
ambiguus. It gives the preganglionic fibers to the thoracic organs. The dorsal nucleus is also called the
medial ala cinerea.
Lateral to the trigonum nervi vagi is the lateral ala cinerea. Inside this lateral ala cinerea is the tractus
solitarius. The fibers running in this tract terminate in the nucleus tractus solitarius (same as the nucleus
tractus spinalis and tractus spinalis). This nucleus is the viscerosensory nucleus of the mixed cranial nerves
(VII, IX, X). It is the taste-sensory nucleus of the facial and glossopharyngeal nerves and the general
viscerosensory nucleus for the glossopharyngeal and vagus nerves.
The nucleus ambiguus is found in the ventrolateral motor column. The medulla also contains the
nucleus tractus spinalis nervi trigemini and tractus spinalis nervi trigemini, the nuclei of Goll and Burdach,
the olivocerebellar tract, and vestibular nuclei.
In the white matter, the fasciculus longitudinalis medialis, tectospinal tract, spinothalamic tract, posterior
spinocerebellar tract, pyramidal tract, and the anterior spinocerebellar tract are found.
PONS
It has a ventral or basal surface and a dorsal surface. The ventral surface is convex forward. In the
midline, there is a groove called the sulcus basilaris (for the basilar artery). The dorsal surface forms the
floor of the fourth ventricle or the upper triangle of the rhomboid fossa.
The pons is separated into two main parts: the base and the tegmentum. The corpus trapezoideum,
having the nucleus corporis trapezoidei, separates them. The base is ventral to the nucleus, and the
120
tegmentum is dorsal to it. The tegmentum of the pons is continuous with the tegmentum of the
mesencephalon. It is the denser part of the pons and has many tracts passing through it.
The base contains the pontine nuclei. The pyramidal tract runs between these nuclei. This tract is not
a single, dense tract in the pons. Rather, it is separated into many bundles among the pontine nuclei. The
frontopontine tract of Arnold and the parietotemporooccippitopontine tract of Türck terminate in these
nuclei after descending through the internal capsule from the cortex. The tract that originates from these
nuclei is the pontocerebellar tract (a crossed tract).
In the ventrolateral motor group is the nucleus of the trigeminal nerve. In the dorsomedial motor group
is the nucleus of the abducens.
A cross section between the pons and medulla (at the border) should show the nucleus of the facial nerve
and the nucleus of the abducens nerve. If the section is made above (in the pons), you should find the
trigeminal nuclei below the locus ceruleus. It doesn't form an elevation because it is in the ventrolateral
motor column. The sulcus limitans separates the motor nuclei from the sensory nuclei of the trigeminal
nerve.
The superior salivatory nucleus (the vegetative nucleus of the facial nerve) is found between the nuclei of
the facial and trigeminal nerves. This is the uppermost level of this nucleus. The preganglionic fibers
from this nucleus terminate in the submandibular ganglion.
The sensory nuclei of the vestibulocochlear nerve (namely the superior-Bechterew and lateral-Deiters)
are found here, in the lateral recess.
The tegmentum contains tracts: fasciculus longitudinalis medialis, tectospinal tract, spinothalamic tract,
medial lemniscus, and the fasciculus tegmentalis. The fasciculus (or tractus) tegmentalis centralis is
located in the center of the tegmentum. This tract originates from the thalamus and nucleus ruber of the
mesencephalon and descends to the inferior olivary nucleus of the medulla. It is an interconnecting tract of
the extrapyramidal system.
The RETICULAR FORMATION is found throughout the brain stem. The reticulospinal tract originates from
this formation and belongs to the extrapyramidal system.
The vestibulocochlear nerve has two parts: vestibular and cochlear. The vestibular part has four nuclei
(superior, medial, inferior, lateral) located in the vestibular area. The cochlear has two nuclei (ventral and
dorsal) located in the inferior cerebellar peduncle. (Discussed further in "THE EAR").
MESENCEPHALON
It develops from the midbrain vesicle. The cavity of the mesencephalon is the aqueductus cerebri.
Dorsal to the aqueduct is the lamina tecti (or lamina quadrigemina), having the superior and inferior
colliculi. The superior colliculus is connected to the corpus geniculatum laterale. [The metathalamus has
the geniculate bodies (medial & lateral). They are located behind and below the thalamus.] The medial
one is connected to the inferior colliculus of the mesencephalon by a brachium called brachium colliculi
inferioris. These structures together belong to the acoustic system (functionally). The lateral geniculate,
together with the superior colliculus, belong to the visual system. If you follow the optic tract, you can
easily find the lateral geniculate body.
Between the two inferior colliculi is the frenulum of the vellum medullare superius. Lateral to this
frenulum, the trochlear nerve exits the brain.
The ventral surface of the mesencephalon is composed of the crus cerebri. Between the two crura
cerebri is the interpeduncular fossa. The crus cerebri is also called the pedunculus cerebri. In the crus is
the pyramidal tract, the Arnold tract, and the Türck tract. Between the crus and the tegmentum is a dark
area called the substantia nigra. The nucleus ruber is located above this. The medial lemniscus passes
through the mesencephalon ventrolaterally to these structures.
The central grey matter (substantia grisea centralis) surrounds the aqueductus cerebri and contains the
different nuclei. In the ventral part, there are the motor nuclei of the oculomotor and trochlear nerves. The
vegetative nucleus of the oculomotor nerve (Edinger-Westphal nucleus) lies dorsal to its motor nucleus.
The Edinger-Westphal nucleus sends preganglionic fibers to the ciliary ganglion. The ciliary's
121
postganglionic fibers innervate the musculus sphincter pupillae and the ciliaris muscle (therefore, the nucleus
is responsible for the pupillar reflex).
In the dorsal part of the central grey is a sensory nucleus of the trigeminal nerve, called the nucleus
tractus mesencephali nervi trigemini (3rd sensory nucleus of the trigeminal nerve). This is the proprioceptive sensory nucleus. It contains pseudounipolar neurons as do the spinal ganglia. This is the only
case in the body where central sensory neurons originate inside the brain. The peripheral processes of
these neurons run out to the muscle spindle of the masseter and temporalis muscles. The central process
descends in the tractus mesencephali to the motor nucleus of the trigeminal nerve (in the pons) and synapses
with the motor neurons there. The fibers from the motor neurons run to the masseter and temporalis
muscles, innervating them and providing the pathway for the proprioceptive reflex of the masseter. It is a
simple monosynaptic, bineuronal reflex.
There are important vegetative centers here. A pathway descends from them to the vegetative nuclei of
the brain stem and spinal cord called the Schütz tract of fasciculus longitudinalis dorsalis.
122
CEREBELLUM
In the dissecting room, the tonsil is frequently discussed. Its medical importance: in the case of the
increased pressure in the skull, the medulla and tonsil are invaginated into the foramen magnum and can
press the medulla against the basilar bone. The medulla contains important vegetative centers which can be
compromised. Other important features are the hemispheres, vermis, folia, lingula (first lobe of the vermis located on the velum
The SUPERIOR CEREBELLAR PEDUNCLE connects the mesencephalon with the cerebellum. It has the
main efferent pathway from the cerebellum to the nucleus ruber (cerebellorubral tract) and to the ventral
anterior and ventral lateral nuclei of the thalamus.
All efferent tracts originate from the Purkinje cells. The fibers from these cells terminate in the
intracerebellar nuclei (dentate nucleus, nucleus globosus, nucleus emboliformis, nucleus fastigii). It is only
necessary to show the dentate nucleus (in the white matter of the hemispheres), giving rise to the
dentatothalamic tract. Some fibers of the efferent tract do not terminate in the intracerebellar nuclei, but
terminate in the vestibular lateral nucleus (Deiters). The rest continue to the nucleus ruber and the
thalamus. The superior cerebellar peduncle has one afferent tract called the anterior spinocerebellar tract
and another called the tectocerebellar tract to the tectum of the mesencephalon.
The MIDDLE CEREBELLAR PEDUNCLE has the pontocerebellar tract and the reticulocerebellar tract.
The INFERIOR CEREBELLAR PEDUNCLE has the posterior spinocerebellar tract, the vestibulocerebellar
tract, and the olivocerebellar tract. There are additional tracts with less importance: cuneocerebellar and
trigeminocerebellar tracts. Its efferent tract is the cerebellovestibular tract.
According to the histology of the cerebellum, the termination of these tracts should be known. The
olivocerebellar tract is the only tract that terminates by climbing fibers on the Purkinje cells. All other tracts
terminate by mossy fibers which synapse with the granulosa cells.
The cerebellum functionally has three main parts: vestibulocerebellum, spinocerebellum, pontocerebellum. The vestibulocerebellar fibers terminate in the vestibulocerebellum which influences the movements of the vestibular system. We can walk toward something without seeing because the vestibular
system sends afferents to the vestibulocerebellum, which in turn coordinates our movements through the
vestibular nuclei, and through these nuclei to the vestibulospinal tract and to the fasciculus longitudinalis
medialis.
The flocculus, pedunculus flocculi, and nodulus belong to the vestibulocerebellum (the oldest part of the
cerebellum is also called the archicerebellum.
The anterior lobe, pyramis, uvula, and the connecting part of the hemispheres belong to the spinocerebellum (paleocerebellum). The spinocerebellar tract terminates here. The fibers run out to the
intracerebellar nuclei, and from there to the nucleus ruber and the thalamus, controlling the voluntary
movements through the extrapyramidal tract.
The pontocerebellum is the middle (largest) part of the cerebellum. It is the phylogenically newest part
(neocerebellum). The pontocerebellar tract terminates in this part as well as the spinocerebellar tract (one of
its two terminations).
123
EYE
EXTRAOCULAR MUSCLES
There are six extraocular muscles plus the levator palpebri superioris. These muscles surround the eye,
forming something like a cone. The origin of the muscles is the annulus tendineus which surrounds the
optic canal. From this tendinous ring, all the muscles arise except the inferior oblique muscle, which arises
from behind the posterior lacrimal spine (posterior border of the lacrimal sac). The muscles are: superior,
inferior, medial, and lateral recti; superior and inferior obliques.
The eye is divided into eight octants: the equator divides the eye into anterior and posterior halves. A
sagittal plane divides it into medial and lateral halves. The horizontal plane separates it into superior and
inferior halves. So, the three planes together divide the eye into eight octants. These are named superioranterior-medial, superior-anterior-lateral, posterior-superior-medial, etc.
FASCIAL SHEATHS OF THE EYEBALL
Periosteum of the orbital bone (periorbita forms the lacrimal sac, cochlear spine)
Orbital fat (corpus adiposum orbitae)
Fascia bulbi Tenon's fascia
Sclera
The septum orbitale connects the palpebra with the bone of the orbit. Like a diaphragm, it stands
frontally before the eye (it closes when we close our eyes).
The superior and inferior recti are attached to the anterior octants in the middle of the eye. The axis of
these muscles diverges a medially from the axis of the eye a little (~23). This way, the superior rectus
elevates the eye, adducts it, and rotates it medially. The inferior rectus depresses the eye, abducts it, and
rotates it laterally.
The medial and lateral rectus muscles are in the horizontal plane, and they are attached to the lateral and
medial surfaces of the eye in the anterior octants. This way, the medial rectus adducts, and the lateral rectus
abducts.
The actions of the oblique muscles contradict their names in the elevation and depression of the eyeball.
The superior oblique muscle makes depression, abduction, and medial rotation. The tendon of the superior
oblique hooks around the trochlear spine (on the frontal process of the maxilla), then runs posteriorly and
laterally. Finally, it is attached to the lateral-posterior-superior octant of the eye. This way, it elevates the
posterior half of the eye and depresses the anterior half. So, what we see is depression. The inferior
oblique muscle is also attached to the lateral-posterior-inferior octant. It makes elevation, abduction, and
lateral rotation.
All superiors make medial rotation, and all inferiors make lateral rotation. Oblique muscles make
abduction. The oblique muscles work against their name in the elevation and depression.
Only the lateral superior rectus and superior, inferior oblique are visible in the preparation with the
muscles (frequently given in the exam).
Innervation: the oculomotor nerve innervates the superior, medial, and inferior recti; and the inferior
oblique. The trochlear nerve innervates the superior oblique. The abducens nerve innervates the rectus
lateralis. [LR6SO4 - the rest from CN III]. The oculomotor nerve also innervates the levator palpebrae
124
superioris. It arises from the same tendinous ring as the others and is inserted to the superior palpebra.
function is to elevate the superior palpebra.
Its
The eye has three membranes: tunica externa (fibrosa), tunica media (vasculosa), tunica interna
(mucosa – neuroepithelium).
The tunica externa is composed of the cornea (anterior 1/5) and the sclera (posterior 4/5). The middle
tunic is composed of three parts: choroidea (posterior 2/3), ciliary body (middle), iris (anterior). The tunica
interna is composed of the retina which has two parts: the optic part (posterior) and the blind part (anterior).
The borderline between them is the ora serrata.
The posterior part of the retina which layers the choroidea is the optic part. The anterior part layers the
ciliary body and iris (the pars ceca retinae). In the pars ceca, the retina is just a double layer of pigment
epithelium. The optic part has 10 layers:
1) Stratum pigmentosum retinae
2) Stratum bacillorum et conorum
3) Membrana limitans externa
4) Stratum granulosum externum
5) Stratum plexiforme externum
6) Stratum granulosum internum
7) Stratum plexiforme internum
8) Stratum ganglionosum
9) Stratum opticum (layer of optic fibers)
10) Membrana limitans interna.
LENS
The lens is a biconvex lens having a diameter of approximately 9mm and thickness of 4.5mm. It has
anterior and posterior surfaces with the anterior surface having a greater radius of curvature (flatter) than the
posterior. It has anterior and posterior poles. It is surrounded by a capsule. Simple cuboidal epithelium
lines the anterior surface just under the capsule, but not the posterior surface.
The lens has two main parts: the gelatinous cortex and the inner, denser nucleus. The structure is
composed of the lens fiber which develops from the posterior epithelium of the lens. The epithelium
(originating from the placode) is changed to elongated cells forming fibers. These fibers are attached to the
anterior surface, forming an upside-down, Y-shaped raphe. The fibers form a right-side-up, Y-shaped raphe
on the posterior surface.
The lens is attached to the ciliary body by the zonulae ciliaris (zonular fibers). These fibers are attached
to the orbiculus ciliaris (the root - peripheral, posterior part of the ciliary body) and to the folds between the
ciliary process. The ciliary body has two main parts: Orbiculus ciliaris (outer, peripheral part) and Corona
ciliaris (inner, anterior part). From the corona, the ciliary processes protrude into the posterior eye chamber.
So, the zonular fibers arise from the orbiculus and form the corona between the ciliary processes. The fibers
which arise from posterior are attached to the anterior surface of the lens. The fibers arising from anterior
are attached to the posterior surface of the lens. This way, the fibers cross each other.
ACCOMMODATION
If the eye is fixed to the horizon, the zonulary fibers are tense, and the lens is stretched (less curved). If
you look at a close object ("accommodate"), the ciliary muscle contracts. This way, the zonular fibers
become looser as the origin and attachment approach each other. The lens becomes more curved by its own
elasticity. If you cut out the lens, it will contract.
This accommodation is a reflex which is connected to the oculomotor nerve nucleus (mainly the EdingerWestphal). This reflex is closed in the cortex. The afferent part of the reflex is inside the visual pathway:
Optic nerve optic chiasma optic tract lateral geniculate body optic radiation visual
cortex. From the visual cortex, another fiber runs to the motor eyefields of the frontal lobe. From this
motor eyefield, another fiber runs to the oculomotor nuclei (visceromotor and somatomotor). Preganglionic
125
fibers from the Edinger-Westphal nucleus run to the ciliary ganglion, and postganglionic fibers go to the
ciliaris muscle and the sphincter pupillae muscle. At the same time, the motor nucleus of the oculomotor
nerve sends fibers to the rectus medialis. Together with the accommodation, the two eyes converge.
CHAMBERS OF THE EYE
The aqueous humor is secreted by the processus ciliaris into the posterior eye chamber.
Borders of the posterior eye chamber:
Anterior: iris
Posterior: lens, zonulary fibers, corpus vitreum
Lateral:
ciliary body
The corpus vitreum is between the lens and the zonulus fibers.
From the posterior chamber, humor aquosus circulates into the anterior chamber through the pupil.
Borders of the anterior eye chamber:
Anterior: cornea
Posterior: iris
The absorption of the humor is from the anterior chamber through the ciliary canals (spaces at the
iridocorneal angle) which are called Fontana's spatia anguli iridocornealis. From these spaces, the
Schlemm canal, the sinus venosus sclerae, drains the humor. From the Schlemm canal, the aquous veins
take the humor to the episcleral veins anterior ciliary vein superior ophthalmic vein.
The function of this aquous humor is similar to that of the cerebrospinal fluid. It maintains the normal
pressure in the eye. If the circulation is stopped, pressure in the eye will increase (glaucoma).
THE VISUAL PATHWAY
The visual pathway starts from the retina. The first three neuron cell bodies of the visual pathway are
inside the retina. The cones and rods form the first neuron cell body. The bipolar neuron is the second.
The ganglionic cells are the third. The fibers of the ganglionic cells form the optic nerve. The fibers cross
each other partly in the optic chiasma. The nasal fibers (fibers arising from the nasal half of the retina)
cross in the optic chiasma, but the fibers arising from the temporal half of the retina don't cross. Finally, the
optic tract contains fibers from the contralateral nasal half and the ipsilateral temporal retina. The
contralateral nasal retina and ipsilateral temporal retina means the contralateral visual field. The temporal
retina receives light waves from the nasal visual field. The nasal retina receives light waves from the
temporal visual field. In the optic tract, there are fibers from the ipsilateral temporal retina as well as fibers
from the contralateral nasal retina.
The fibers terminate in the lateral geniculate body. From this body, the fourth neuron forms the optic
radiation, terminating in the calcarine fissure of the visual cortex (Brodmann 17). This optic radiation has
two parts: retrolenticular and sublenticular parts. The optic radiation runs through the posterior limb of
the internal capsule, so the majority of these fibers form the retrolenticular part of the internal capsule, behind
the lentiform nucleus. The optic radiaiton hooks around the inferior horn of the lateral ventricle, and these
fibers are called Mayer's loop. The dorsal fibers run dorsal to the lateral ventricle. These fibers run from
the inferior half of the retina and the dorsal fibers from the superior half of the retina, but it means the
inferior visual field. Superior fibers of the retina are from the inferior visual field.
The lateral geniculate body has six layers. Three of them receive fibers from the contralateral eye, and
three from the ipsilateral retina. In the geniculate level, these fibers are not mixed because they terminate at
different layers. In the cortex, they converge on the same cell. So, the picture from the two eyes will be
one picture just in the cortex.
126
PUPIL LIGHT REFLEX
Some fibers leave the optic tract before the lateral geniculate body (or from the l.g.b.). These fibers
terminate in the pretectal nuclei which are in the anterior part of the superior colliculus. Fibers from these
nuclei cross over the midline and terminate in the contralateral Edinger-Westphal nucleus, and without
crossing in the ipsilateral E-W nucleus. These fibers between the geniculate body and E-W nucleus are
running in the fasciculus longitudinalis medialis. Preganglionic fibers from the E-W nucleus run in the
oculomotor nerve to the ciliary ganglion, and from the ciliary ganglion to the sphincter pupilae muscle.
Because the pretectal region sends fibers to both contralateral and ipsilateral E-W nucleus, the reflex is
consensual. This means both pupils will constrict in response to light shone in one eye.
What is the difference if the optic nerve is damaged or if the optic radiation is damaged?
If the optic radiation is damaged, the pupillary light reflex will be intact. In the case of optic nerve
damage, the reflex is also damaged. The fibers from the pretectal region cross over in the midline and
terminate both to the E-W nucleus. This crossing over is in the posterior commissure.
What is the result of damage to the oculomotor nerve?
Only depression and abduction can be done by the eye.
What happens if we use light to the damaged (CN III) eye and examine both eyes?
The other eye will display an intact pupillary reflex, while the damaged eye will not.
If the oculomotor nerve is damaged, the palpebra superioris will be dropped (ptosis). So, in this case, the
following symptoms will be seen:
a) palpebra is dropped
b) pupillary reflex will not work
c) the eye is abducted and depressed.
THE LACRIMAL APPARATUS
The lacrimal gland is located in the lacrimal fossa of the orbital cavity (superolateral region). The
lacrimal gland is a serous gland similar to the parotid, but it has a slightly larger lumen. Also, lymphatic
tissue can be found here.
It has two lobes: superior and inferior. The lacrimal ducts open into the superior fornix of the
conjuctiva in one row next to each other. The tears cover the whole eye by blinking (from the superior
fornix of the palpebra). The absorption of the tears is through the lacrimal punctum (2) in the inferior,
medial end of the inferior palpebra and in the superior, medial end of the superior palpebra. The punctum
lacrimale starts from the lacus lacrimalis (lacrimal lake) in the medial angle of the eye, covering the
caruncula lacrimalis. The punctum lacrimalis leads to the canaliculus lacrimalis (superior and inferior).
First, these two canals run upward and downward. Then, they continue into the transverse part, converging
and draining into the lacrimal sac (in the fossa saci lacrimalis). From the lacrimal sac, the ductus
nasolacrimalis drains the tears into the inferior nasal meatus.
The wall of the lacrimal sac has the lacrimal part of the orbicularis oculi muscle that moves the lateral
wall of the lacrimal sac laterally, making a vacuum which forces the draining of the tears into the inferior
nasal cavity. We can act to this muscle if we blink to fast the majority of the tears will go to the nasal
cavity.
The tear production is under the effect of the facial nerve from the superior salivary nucleus to the
pterygopalatine ganglion by the greater petrosal nerve (preganglionic fibers). Postganglionic fibers go
through the zygomatic nerve lacrimal nerve lacrimal gland. Sensory innervation is given by the
lacrimal nerve (from the ophthalmic).
127
EAR
There is a small yellow structure that has the three ossicles inside. This structure is frequently given in
the exam, together with another preparation of the temporal bone and the pyramidal bone (opened to see
internal structures).
THE BONES
Malleus. The malleus has a head, neck, and manubrium malei. The head is connected to the incus,
forming the incudomalleolar joint. The manubrium is attached to the tympanic membrane, making the stria
mallearis on the outer surface of the tympanic membrane. The lower point of the stria mallearis makes the
umbo, the manubrium itself makes the stria mallearis and the lateral process (termination - upper end of the
manubrium) forms the prominentia mallearis.
Incus. The incus has a body (corpus incudis), a long crus and a short crus. The long crus has a
process at the end called the lenticular process which forms a joint with the head of the stapes: the incudostapedis joint. The short crus is connected to the posterior wall of the tympanic cavity by the posterior
incudis ligament. Both the malleus and the incus have a superior ligament which connects them to the
superior wall of the tympanic cavity. The malleus also has the lateral mallear ligament from the neck of the
malleus to the tympanic notch of the temporal bone. This ligament is parallel to the lateral process of the
incus.
Between the prominentia mallearis and the tympanic notch is the flexid part of the tympanic membrane.
The flexid part, lateral mallear ligament, and the neck surround an area which is called Prussak's space
(infection is sometimes closed there - very hard to cure).
The anterior mallear ligament is a process in the newborn and young children. This ligament in adults
connects the malleus to the petrotympanic fissure (Glader's fissure).
Stapes. It has a joint with the incus (incudostapedis joint). The stapes has a head, anterior crus,
posterior crus, and basis stapedis. The basis is connected to the oval window by the annular ligament of the
stapes.
The tympanic cavity has three main parts. The upper part is called the epitympanon (recessus
epitympanicus) which is above the tympanic membrane. The middle part is called the mesotympanon
(along side the tympanic membrane). The final part is the hypotympanon (a small recess).
The stapes is below and more medial (related to the medial wall of the tympanic cavity: labyrinthic wall).
The stapes covers/closes the oval window of the inner ear. So, the sound waves coming from the air
transmit the resonancy in the tympanic membrane. From the tympanic membrane, through the manubrium
mallei, through the incus and stapes to the oval window into the liquid phase. Medial to the oval window,
there is the scala vestibuli of the perilymph. The perilymph starts at the level of the oval window and the
sound waves go through the scala vestibuli, helicotrema (in the apex of the cochlea), scala tympani, and
finally to the secondary tympanic membrane (crosses the round window - end of scala tympani).
The course of sound waves from the tympanic membrane to the receptor organs is commonly asked
together with the ossicles.
Bone makes up the structures of the bony labyrinth. It includes the vestibulum, the semicircular canals,
and the cochlea. Soft tissues within this structure compose the membranous labyrinth. The space between
the two systems is filled by perilymph.
128
The receptor organ is in the endolymph, in the cochlear duct. This duct is separated from the perilymph
by membranes only (vestibular and basilar membranes). The waves passing through the perilymph make the
stimulus for the Corti organ through the endolymph. This way, the resonance will be transmitted to the
basilar membrane of the Corti organ which has the membrane tectoria. This membrane reaches the hair
cells which receive the stimulus of the sound.
Where the scala vestibuli and the scala tympani communicate with each other in the apex of the cochlea
(cupula of the cochlea) is called the helicotrema.
MUSCLES OF THE OSSICLES
The ossicles have two muscles: the tensor tympani and the stapedius. The tensor tympani tenses the
tympanic membrane and arises from the anterior wall of the tympanic cavity (paries caroticus). The
anterior wall is open above and closed below. Above, the tympanic ostium of the auditory tube opens here.
The tensor tympani runs backward and hooks around the cochleariform process (on the medial wall). From
this point, it runs laterally and attaches to the manubrium malei. So, it moves the manubrium malei
medially (this way, tenses the tympanic membrane) and prevents the inner ear from very intense sounds.
Innervation is given by the mandibular nerve. The tensor tympani develops from the first pharyngeal arch.
The stapedius muscle develops from the second pharyngeal arch and is innervated by the facial nerve. It
arises from the posterior wall of the tympanic cavity. It is a very small muscle. It is attached to the head
(base) of the stapes and moves it backward. This way, it decreases the surface between the stapes and the
perilymph. It also protects the inner ear from loud sounds.
THE TYMPANIC CAVITY
The tympanic cavity has six walls. The lateral wall is the paries membranaceus (tympanic membrane,
stria mallearis, umbo, prominentia mallearis). From the prominentia mallearis, there are two tiny folds
going to the anterior and posterior ends of the tympanic notch. These folds are called plica mallearis
anterior and posterior, bordering the flexid part of the tympanic membrane. The small, superior part is the
pars flexida. The remaining portion is the dense part (pars densa). The tympanic membrane is attached to
the temporal bone by an annulus fibrocartilagineous. It is a funnel-shaped membrane. The plane of this
membrane is oblique (superolateral to inferomedial). So finally, there is a sharp angle between th tympanic
membrane and the external auditory canal, anterior and below. The funnel faces medially.
The medial wall is the paries labyrinthi because it faces the labyrinth (toward the inner ear). On this
wall is the promontory, an elevation made by the first turn of the cochlea (basal curve of the cochlea). The
promontory has a nervous plexus called the tympanic plexus. It arises from the tympanic nerve of the
glossopharyngeal, entering the tympanic cavity between the inferior and medial walls (passing through the
medial wall) and leaving between the superior and medal wall as the nervus petrosus minimus. We also
have sympathetic fibers through the anterior wall of the tympanic cavity, through the coliculi
caroticotympanici (along side the internal carotid artery). The sympathetic fibers and the tympanic nerve
form the plexus.
Behind and above the promontory is the oval window (fenestra vestibuli), covered by the base of the
stapes. This is the beginning of the scala vestibuli. Below the promontory is the round window (fenestra
cochlei) which is the termination of the scala tympani. On the medial wall is the cochleariform process.
The tensor tympani hooks around this process.
The facial canal forms another prominence. The canal is out of the tympanic cavity, but runs between
its medial and superior walls. The descending part of the canal runs between the medial and posterior walls.
This flexure of the canal forms a prominence on the medial wall called prominentia canalis facialis. Above
this prominence, the lateral semicircular canal forms another prominence called prominentia canalis
semicircularis lateralis.
129
The anterior wall is the paries caroticus. The superior part is open, forming the opening of the
tympanic ostium of the Eustachian tube. The tensor tympani muscle is above this.
The inferior wall is the paries jugularis, named for the adjacent internal jugular vein. Between the
inferior and medial walls, the tympanic nerve enters the tympanic cavity.
The posterior wall is called the paries mastoidea because it communicates with the air cells of the
mastoid process through the antrum mastoidea. From the posterior wall, the stapedius muscle arises. The
chorda tympani enters the tympanic cavity from the descending part of the facial canal. It passes through
the tympanic cavity between the malleus and incus and leaves through the petrotympanic fissure. The
chorda runs in the anterior and posterior mallear folds. The anterior ligament of the malleus is inside the
anterior fold.
The superior wall is the paries tegmentalis (tegmen tympani), a very thin wall. Infection is easily
spread through it.
THE AUDITORY TUBE
The auditory tube connects the nasopharynx with the tympanic cavity by two ostia: the ostium
tympanicum and the ostium pharyngeum. The tympanic part is bony, formed by the canalis musculotubarius (inferior part). The next portion, toward the pharyngeal opening, is cartilaginous (composed of
lateral and medial cartilages). Between the two cartilages, there is a space filled by the membanous part of
the auditory tube. The medial lamina is a little larger than the narrower, lateral lamina.
The pharyngeal opening is surrounded by the salpingopalatine and salpingopharyngeal folds. The most
important function of this tube is to equalize the pressure outside and inside the tympanic membrane.
Normally, the pharyngeal opening is closed, but it opens during swallowing.
Infection spreads through the Eustachian tube into the tympanic cavity from the pharynx, resulting in
otitis media.
THE BONY AND MEMBRANOUS LABYRINTH
Cochlea. The cochlea is anterior, inferior, and medial to the semicircular canals. Between them is the
vestibulum. The apex of the cochlea faces laterally. The modiolus is the axis of the cochlea.
The cochlea has 2¾ turns and starts from the recessus sphericus. The apex is called the cupula of the
trochlea. The basal curve (turn) makes the promontory of the medial wall of the tympanic cavity. The
modiolus is inside the cochlea in its axis. A spiral lamina from the modiolus makes the 2¾ turns. The
lamina spiralis ossea separates the bony cochlea into inferior and superior parts. The inferior part is the
scala tympani, and the superior part is the scala vestibuli. In the membranous cochlea, they are separated by
the cochlear duct.
The spiral ganglion is the sensory ganglion of the cochlear nerve. It is found in the lamina spiralis ossea
and contains bipolar neurons.
Inside the bony cochlea is the cochlear duct which has two blind ends. One end is in the cupula (cecum
cupulare), and the other end is in the vestibule (cecum vestibulare).
Vestibulum. It has two parts: the recessus sphericus, and the recessus elipticus. These two recesses
are separated by a bony crest from inside. The semicircular canals arise from the recessus elipticus. The
cochlea starts from the recessus sphericus. The scala vestibuli starts from the oval window on the vestibule.
Inside the vestibulum, we have the sacculus and the utriculus (the two membranous parts of the
vestibule). The sacculus is connected with the cochlear duct by the ductus reuniens and with the utriculus
by the utriculosaccular duct. From the utriculus, the semicircular canals open out. There is another
membranous duct which starts from the utriculosaccular duct called the ductus endolymphaticus, having a sac
at the end. This sac is believed to be the site of absorption of endolymph.
130
Semicircular canals. There are three semicircular canals. Two of them are in the vertical plane
(anterior and posterior). The axis of the anterior canal is vertical to the axis of the pyramid. The axis of
the posterior is parallel to the axis of the pyramid. The lateral semicircular canal is in the horizontal plane.
These three canals have six ends. Each has a crus simplex and an ampullar crus. The two crura simplexes
of the anterior and posterior semicircular canals are fused, forming the crus commune. Finally, the canals
open into the vestibule by five openings instead of six.
Each of the three main planes has a canal which is sensitive for angular acceleration of the head. In the
ampulla, there is a receptor called the crista ampullare. These crests are sensitive to the angular movement.
If the head turns, one of these receptors is highly sensitive to this angular acceleration. The receptors in the
utriculus and sacculus are called macula utriculi and macula sacculi respectively, and they are flat elevations.
These maculae are sensitive to the linear acceleration, such as that which happens in an elevator ascending or
descending. These receptors are in the endolymph, inside the membranous duct.
In the cochlea is the cochlear duct which has the Corti organ as a receptor inside. In the cochlear duct,
the basilar membrane arises from the lamina spiralis ossea. This lamina has two limbs: limbus
tympanicum and limbus vestibulare. The tympanic limb has a membrane which is the basilar membrane.
It separates the scala tympani from the ductus cochlearis. The vestibular limb has the vestibular membrane
which separates the cochlear duct from the scala vestibuli.
THE VESTIBULOCOCHLEAR NERVE
The vestibulocochlear nerve has two parts: the vestibular nerve and the cochlear nerve. These go
through the porus acusticus internus into the meatus acusticus internus. In the fundus, there are four
quadrants with five openings. The facial nerve passes through the superior-anterior quadrant. The
cochlear nerve passes through the inferior-anterior quadrant. The utriculoampullar nerve passes through the
superior-posterior quadrant. The saccular and posterior ampullar nerves pass through the inferior-posterior
quadrant.
Vestibular nerve. The vestibular nerve has different branches:
Utriculoampullar nerve (giving the utricular n. and anterior and lateral ampullar ns.)
Saccular nerve
Posterior ampullar nerve.
These nerves enter the vestibule through the different cribriform areas of the vestibule and terminate at
the different receptors (macula sacculi, macula utriculi, crista ampullaris).
The ganglion of the vestibular nerve is the vestibular ganglion, located in the meatus acusticus internus.
The peripheral processes of these neurons terminate in the vestibular nuclei, mainly in the superior, medial,
and inferior (less so in the lateral). From these nuclei, there are ascending and descending pathways. The
ascending pathways terminate on the oculomotor, trochlear, and abducens nuclei (motor nuclei of the eye).
The descending fibers terminate on the motor nuclei of the spinal nerves innervating muscles of the head and
neck.
The lateral vestibular nucleus is related to the cerebellum, so efferent pathways from the cerebellum and
vestibulospinal starts from here controlling the motor movements.
The vestibular receptors are sensitive to the circulation of the endolymph. In the anterior and posterior
semicircular canals, the ampullofusal (away from the ampulla)is the exact stimulus. In the lateral canal,
the ampullopetal (toward the ampulla) is the stimulus.
Cochlear nerve. The cochlear system is composed of five neurons. The FIRST order neuron is in the
cochlear ganglion (or spiral ganglion) in the lamina spiralis ossea. The peripheral processes terminate in
the receptor in the Corti organ around the hair cells. The central process terminates in the ventral and dorsal
cochlear nuclei.
The SECOND order neuron from the dorsal cochlear nuclei crosses over the midline and terminates in the
contralateral superior olivary nucleus. This crossing forms the striae acusticae or striae medullaris
separating the pons from the medulla. The fibers arising in the ventral cochlear nucleus terminate mainly in
the ipsilateral superior olivary nucleus and nucleus corporis trapezoidei. From there, they cross over the
131
midline and ascend as the lateral lemniscus. The fibers in the lateral lemniscus are from the THIRD order
neurons. These fibers ascend to the inferior colliculus, synapse there, and the FOURTH order neurons from
the inferior colliculus send ascending axons to the medial geniculate body through the brachium colliculi
inferioris. The FIFTH order neuron arises from the medial geniculate body up to the acoustic (auditory)
cortex.
The lateral lemniscus is a superficial pathway which is sometimes visible on the brain. The medial and
lateral lemnisci pass through the tegmentum, the pons, and the mesencephalon. Between them is the
spinothalamic tract.
132
Index:
1.0 Upper Limb
1.11 Pectoral region 1-3
1.12 Axilary region 3
1.13 Anterior brachial region 3 -4
1.14 Anterior cubital region 4
1.15 Anterior antebracjial region 5
1.16 Volar carpal region 5-6
1.17 Palmar region 6-7
1.18 Deltoid region 8
1.19 Posterior brachial region 9
1.20 Posterior cubital region 9
1.21 Posterior antecubital region 9-10
1.22 Foveola radialis 10
1.23 Dorsalis manus region 11
1.24 Dorsalis scapular region 11-12
2.0 Lower Limb
2.11 Gluteal region 13-14
2.12 Posterior femoral region 14-15
2.13 Pupliteal region 15-16
2.14 Posterior crura region 16-17
2.15 Medial maleular region 17
2.16 Lateral maleular gegion 17
2.17 Dorsal pedis region 18
2.18 Sub-inguinal region 19-20
2.19 Anterior femoral region 21
2.20 Anterior grnicular region 22
2.21 Anterior crural region 22-23
2.22 Plantar region 23-24
3.0 Skull
3.11 Skull 25-28
3.12 External surface of the skull 28-30
3.13 Mandible 31
3.14 Orbital cavity 31-32
3.15 Nasal cavity 33
3.16 Oral cavity 34
3.17 Pterigopalatine fossa 34
3.18 Temporo-mandibular joint 35-36