* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Our Lady`s Hospice, Harold`s Cross
Infection control wikipedia , lookup
Neonatal intensive care unit wikipedia , lookup
Medical ethics wikipedia , lookup
Patient safety wikipedia , lookup
Adherence (medicine) wikipedia , lookup
Mass drug administration wikipedia , lookup
Nurse anesthetist wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Nurse–client relationship wikipedia , lookup
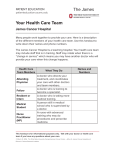
Agency Orientation to Extended Care Unit: Introduction Mary Aikenhead had pursued her vocation by opening the doors to care for the poor and the dying of Dublin in 1879. Today we continue that legacy of care to those who can no longer remain at home (Extended Care Unit / ECU). The emphasis of care is also on those who may remain at home with the support of a reablement programme (Community Reablement Unit / CRU). Our Mission Statement: ‘Our Lady’s Hospice founded in 1879 by the Sisters of Charity strives through a team approach and in an atmosphere of loving care to promote wholeness of body, mind and spirit.’ We strive to provide healthcare services that foster our core values: Dignity Compassion Justice Quality Advocacy Emergency Response: Dial extension 633 (this is an emergency-only extension located at reception), give your name, department/location and nature of problem e.g location of fire or serious injury requiring urgent or immediate attention. Staff panic alarm are available for use by staff members while on duty on all ward areas and should be worn at all times. Matron’s Office Cover: Support service available 24 hours through matron’s office. To contact please call extension/bleep 827. Health And Safety: It is the duty of all Agency Nurses to: Read, understand and cooperate with a Department Safety Statement. Read and understand all relevant OLH, Nursing, Organisational and Drug Safety Policies. Seek clarification of any issues that they do not understand within all relevant OLH Policies relating to the ward areas. Report any unsafe condition, practice, substance, equipment or situation as soon as reasonably practicable to the CNM2 or Person in charge Properly use any resources made available to them. Report any accident/incident or near miss to the CNM2 or Person in charge as soon as possible. Ensure they receive initial training in Manual Handling and attend 2yearly refreshers therafter Extended Care Unit (ECU), which is in the original Hospice building offers Gerontological expertise and care to frail older people and people with chronic illness. The philosophy of the Extended Care Unit is: ‘Founded on the belief that each person in our care is a unique human being who is complex, interdependent, physical, psychological, spiritual and has social needs. It is the philosophy of Extended Care that each patient is an individual entitled to appropriate multi-disciplinary care and where possible freedom of choice in that care.’ Within ECU there are six long stay wards and the Community Reablement Unit (CRU) and they are as follows: 1. St Camillus Ward, home to 10 male residents. Clinical Nurse Manager II - Mary T Carroll Clinical Nurse Manager I - Catriona Whitty 2. St Charles’ & St Paul’s Ward, home to 22 male and female residents Clinical Nurse Manager II - Nora O’Connor Clinical Nurse Manager I - Jenny Sullivan Taiwo Ogunyemi Happiness Aku 3. St Mary’s & St Joseph’s Ward, 10 female ward. Clinical Nurse Manager II Clinical Nurse Manager I - Patricia Lardner 4. St Patrick’s – Nursing Development Unit, home to 14 residents. Clinical Nurse Manager II - Chris Dalton Clinical Nurse Manager 1 – Helen Lowry 5. St Michael’s Ward, is situated in Anna Gaynor House and is home to 25 male and female residents. Clinical Nurse Manager II - Aurie O’Sullivan Clinical Nurse Manager I - Eleanor Cunnane Mary Cunningham 6. St Benedict’s Ward, is also situated in Anna Gaynor House , home to 25 male and female residents. A/Clinical Nurse Manager II - Catriona Whitty Clinical Nurse Manager I - May Wright Mildred Advincula Priorities of Care: Provide assistance with residents’ Activities of Daily Living in a patient centered approach Assessments, implementation and evaluation of care needs of individual patients. To liase with other members of the multidisciplinary team To keep accurate and legible records/documentations Implement appropriate practices in line with the policies of Our Lady’s Hospice Limited e.g. Drug Administration Policy, Infection Control Respect the dignity and confidentiality of each patient at all times and serve as an advocate Medical Conditions Affecting ECU Patients Dementia Stroke Parkinson’s Disease Bipolar Affective Disorder Multiple Sclerosis Diabetes Mellitus Syringomyelia Hypertension / Hypotension History of Falls Osteoarthritis Renal Impairment Diverticular Disease Depression Motor Neuron Disease Common Medications Used: Analgesics – paracetamol/codeine/morphine Prophylaxis for MI/Stroke – Nu-Seals 75 ( aspirin), Plavix, Hypertension – Adalat, Zestril, Tritace, Tenormin, Meldopa, Istin, Inderal, Isoptin, Emcor, Dilzem, Coversyl, Betaloc, Atecor, Aldomet, Adalat Angina – Atecor, Dilzem, Imdur, Inderal, Isoptiin, Istin, Nitrolingual spray, Tildiem, tenormin, transiderm-Nitro patch Diuretics– Fruco, Frumil Laxatives Anxiety disorders– Ativan, Anxicalm, Calmax, Citrol Epilepsy/Seizures – Epanutin, Epilim, Neurontin, Tegretol Senior Members of the Multidisciplinary Team: Director of Nursing: Assistant Director of Nursing Practice Development Nurse Admin Sister Night Sisters Resource Nurse Clinical Nurse Manager(s) Medical Team Medical Director Medical Officer Occupational Therapy Physiotherapy Social Worker Pharmacist Chaplain RC C of I Sr Helena McGilly (ext/bleep 825) Linda Kearns (ext/bleep 826) Rowena Cueto (ext 827/793, bleep 174) Ana Cuerpo (ext 827/793, bleep 827) Mary Tierney (bleep 368) Marie Whitty Sr Rose O’Rourke (bleep 389) as listed above Dr Dennis Donohoe Dr George Robles Dr Sheila Parumal Carol Reynolds Andreya Kelly Margaret Healy Kathleen Keaveney Miriam Sanfey Sheila Sullivan Gabrielle Corbette Sheron Toolan Roisin Adams Fr John Craven Sr Rita Keegan Liz Coyle Rev Canon Neil McEndoo 7. St Anne’s Community Reablement Unit, Which is a pilot programme for the country, offers a step up intermediate programme package of care specific to elderly people to which will enable them to continue living at home. CRU facilitates 24 patients who each in turn have a multi-disciplinary review and intensive therapy. Liaison Nurse - Cecilia O’Malley Clinical Nurse Manager II - Karen McElwaine Clinical Nurse Manager I - Marguerite Crowe Kay Byrne Medical Director - Dr. Dennis Donohoe Consultant Geriatrician - Dr. Miriam Casey (SJH) Specialist Registrar - Dr. Joe Browne (SJH) SHO - Dr. George Robles / Dr Sarah Dowling Social Worker - Aine Flynn Physiotherapist - Mary Weakliam Emily Adamson Occupational Therapist Pharmacist Dietician Unit Secretary David White Sheila Ryan - Gill McHugh Aoife Synnott - Aine frewen - Michael Maher - Avril Halligan Medical Conditions Affecting CRU Patients Parkinson History of Falls Asthma Hypertension / Hypotension Depression Aneamia Bronchitis Stroke Osteoarthritis Osteoporosis Fracture Rheumatoid Arthritis PTB Renal Impairment Diverticulities TIA Common Medications Used: Analgesia – Solpadeine, Solpadol, Panadol, Lyrica, Dicolfenac, Dona, Neurontin Bisophossonates – alendronate, Actonel, forsteo inj, Bonvera Vitamin Supplement – calcichew, One-Alpha, Centrum, Galfer, Folic Acid Proton Pump Inhibitor – Zoton, Nexium Diuretic – Fruco, Lasix Cardiac – Nu-seal Aspirin 75, Plavix, Zanidip, Ramipril, Emcor, Warfarin, Coversyl, Digoxin Laxatives – Lactulose, Senokot, Milpar, Movicol Antidepressant – Cipramil, Lormetazepam, Sertraline Sedatives – Zopliclone, Zolpiderm Cholesterol – Pravastin, Lipitor All Reablement clients are for full treatment / resuscitation Our Lady’s Hospice, Harold’s Cross: Drug Administration Guidelines General Principles and Responsibilities: The prescription or medications order should be verified that it is correct, prior to the administration of any product. Clarification of any questions regarding the medication order should be conducted at this time with the appropriate health care professional. The Five Rights of Medication Administration should be applied to each patient encounter. The five rights are: 1. Right medication. 2. Right patient / client, the nurse should be certain of the identity of the person. 3. Right dose. 4. Correct form of the medication, route and administration method as prescribed. 5. Right time. The expiry date of the medication should be checked prior to administration. Expired medications should not be administered. All MDA drugs and drugs for parenteral administration, must be checked by a second nurse. Oral medication (except MDA drugs) may be administered by a single nurse. The preparation and administration, of a medical product must be performed by the same nurse. The principles of aseptic technique and appropriate precautions should be observed during the preparation and administration of the medical product. The assessment and evaluation of administered medication should encompass the following observations: vital signs, laboratory values, effectiveness method and of administered medical product; medication allergies, side effects, adverse reactions, toxicity, interactions and contraindications. The administered medical product and the patient / client response should be adequately documented. Educational information should be provided to patients / clients as appropriate and as required. It is appropriate to exercise professional judgement to withhold a medical product if indicated. Consult a peer, medical practitioner, pharmacist or nurse manager as applicable. Transcribing of medication orders (by the nurse) should not occur in any setting where health care is provided. This is the responsibility of a medical practitioner. A medical product prescription provided by fax, by a medical practitioner for a patient / client under his supervision should be signed by the practitioner. The nurse will sign date and time of the administration on the fax prescription sheet, which will be photocopied, and the two copies inserted in the patients notes. The prescription will be written into the patient’s drug chart if subsequently administration are required. The only acceptable time a verbal or telephone order should be taken from a medical practitioner is in an emergency situation, where there is an immediate unplanned patient / client need. Guidelines for MDA Dugs : An Overview 1. MDA Drugs MDA drugs are controlled drugs, classified in five schedules, under the Misuse of Drugs Act, 1977 (No. 12) and the Misuse of Drugs Act, 1984 (No 18), (DP 06) MDA CD2 drugs are the most relevant to nursing practice, and include most opoid drugs. It is the nurse’s responsibility to become familiar with and to follow Our Lady’s Hospice Policies, Procedures and Guidelines in relation to the safe acquisition, storage, checking procedure and administration of MDA drugs. 2. Pharmacy Ordering Procedure A requisition must be signed (in duplicate), in the Controlled Drugs Register, by the CNM / nurse in charge, (DP 02) The requisition is signed by a pharmacist to indicate that the drugs have been supplied. A Registered Nurse must go to the pharmacy to order and collect MDA drugs, (DP 02). 3. Safe Storage of MDA Drugs On return, the order is checked with another Registered Nurse, and stored into the suitably locked cupboard to which access is restricted (DP 03) Controlled drugs (MDA’s) must be stored in an (MDA cabinet), Misuse of Drugs (Safe Custody) Regulation 1982. It must be a locked cabinet, within a locked cabinet, the keys of which are kept on the person of a Registered Nurse only (DP 03). At no time can MDA drugs be stored on the regular drugs trolley, (DP 03) A discrepancy in the count must be reported to the Clinical Nurse Manager, to the Pharmacist and to Nursing Administration immediately, (DP 03) If / when new patients bring in own medications, including MDA drugs; where possible, these are sent home. Otherwise, they are clearly labelled and stored (in a separate locked press) away from the ward stock drugs until the patient is going home, (DP 03). 4. Checking of MDA C2 Drugs The Controlled Drugs Register is updated, each time an MDA drug is administered and signed by both the administering RGN and the checking RGN, (DP 07 & DP 08). A stock balance check will be carried out on all MDA drugs; at each individual transaction, & twice daily in all units, (ECU, RRU, CRU & PCU) in Our Lady’s Hospice complex, by two Registered General Nurse, (DP 06, DP 07, DP 08). 5. Administration of MDA CD2 Drugs Two Registered Nurses / Registered Nurse & Medical Practitioner, must check the MDA C2 drug, one of whom must administer the drug immediately, (DP 07 & DP 08). Always follow the ‘five rights’ when administering MDA drugs, (DP 04, 07 & 08). Check out MDA drugs and administer to each patient individually, (DP 06). When an MDA C2 drug is administered, the details are recorded in Controlled Drugs Register, in the patient’s drug chart& in the nursing notes, (DP 04, DP 07 & DP 08). It is the nurse’s responsibility to acquire and maintain competency regarding the safe storage, checking and administration of MDA Drugs. If in any doubt, check with an experienced / senior colleague before you proceed. References Our Lady’s Hosice Policy Folder An Bord Altranais (2000), code of Professional Conduct for each Nurse and Midwife An Bord Altranais (2000), Scope of Nursing Practice An Bord Altranais (2003), Guidelines to Nurses and Midwives on Medication Management Infection Control Guidelines Control of infection within the Hospice is the responsibility of all personnel in order to minimise the risk of patient and staff. Standard Precautions apply to: 1. 2. Blood All body fluids, excretions and secretions except sweat regardless of wether they contain visible body fluids Non intact skin Mucous membranes 3. 4. Standard precautions are designed to reduce the risk of transmission of microorganisms for both recognised and unrecognised sources of infection and they are as follows: Handwashing – the single most important measure to reduce the risk of transmitting micro-organisms from one person to another and from one site to another on the same patient. Handwashing thoroughly between patient contact and after contact with blood, body fluid, secretions and excretions and equipment or articles contaminated is an important component of infection control. The principle of handwashing is primarily that of the removal of dirt and micro-organism by using running water, sudsing, vigorous friction for at least 15 seconds and thorough rinsing. Hand wash procedures are available at most of the washing facilities within the Hospice. Gloves – are worn to reduce the risk of the possibility that the hospital personnel will transmit their own micro-organisms to patients. I t is also to reduce the risk of hospital personnel transmitting micro-organism from one patient to another. It is to reduce the risk of hospital personnel becoming infected with micro-organisms that are present in the patients bodily fluids. Use gloves when doing procedures involving contact with bodily fluids, mucous membranes while tending to patient care, soiled linens and cleaning up spills containing blood or bodily fluids. Wash hands thoroughly prior to wearing and on removal of gloves Protective Clothing – Various types of masks, goggles and face shields are worn alone or in combination to provide barrier protection by assessing the risk of splashing. A mask that covers both the nose and mouth and goggles or a face shield are worn during procedures and patient care activities that are likely to generate splashes or sprays of blood, body fluids, excretions or secretions. Gowns/Plastic aprons are worn to provide barrier protection and reduce opportunities for transmission of microorganisms. They are worn to prevent contamination of clothing and protect the skin of personnel from blood and body fluid exposure and must be removed before leaving the patients environment and hands are washed. Safe Handling of Spillage – Blood should always be handled with the personal “no touch” attitude instinctively adopted for urine and faeces. Care should be taken to contain spills by prompt attention to disposal. Gloves and protective clothings are to be worn. Most items to clear spillage may be obtained from ward sluice room. Hypochlorite granules (Titan) are available for localised spills, granules are sprinkled freely over the spill and after two minutes a gel should form, the gel may then be transferred to a yellow bag. Discard gloves and apron same and wash hands thoroughly. Sharps – Wherever possible syringes and needles should be discarded as one unit. Needles should NOT be resheathed. There should be sufficient numbers of sharps containers within the ward and should be sealed when three quarters full. Gloves should be worn during procedures. In the event of Accidental Needle Stick Injury immediately: 1. Encourage bleeding of the wound under running water. 2. Wash the wound thoroughly under running water using hibiscrub or betadine. 3. Cover the wound with a waterproof dressing. 4. Report the incident to the Senior person present for further management. 5. An Incident Form must be completed. Please refer to Infection Control Manual and Policy Folders available in the wards. Reminder Uniforms may not be worn to and from Our Lady’s Hospice, changing room facilities are provided for your use. Abbreviation’s Listings for Nurses Notes (2006 - 2007) The following list consists of the only abbreviations to be used in nursing documentation of Our Lady’s Hospice. A. fib: Atrial Fibrillation A.D.L’s: Activities of daily living ADON: Assistant Director of Nursing A.I.D.S.: Acquired Immune Deficiency Syndrome ABGs: Arterial Blood Gases AGH: Anna Gaynor House AMNCH: Adelaide & Meath Hospitals incorporating the National Children’s Hospital APTT: Activated Partial Thromboplastin Time B.B.T.: Berg Balance Test B.D.: Bis Die (twice daily) B.O. : Bowel Open B.P.: Blood Pressure C&S: Culture and sensitivity C.A.B.G: Coronary Artery Bypass Graft C.C.F: Congestive Cardiac Failure C.N.M. 1, 2, 3: Clinical Nurse Manager C.O.P.D: Chronic obstructive pulmonary disease C.S.U.: Catheter specimen of urine C.X.R.: Chest X Ray CA: Care Assistant CRU: Community Rehabilitation Unit CT: Computed Tomography Imaging DON: Director of Nursing Dx: Diagnosis E.C.G.: Electrocardiograph E.M.S.: Eldery Mobility Scale ECU: Extended Care Unit ESR: Erythrocyte Sedimentation Rate F.O.B.: Faecal Occult Blood G.I: Gastrointestinal G.U.: Genitourinary GP: General Practitioner H.D.L.: High Density Lipids H.I.V: Human Immunodeficiency Virus Hb: Haemoglobin Hx: History I.D.D.M.: Insulin Dependent Diabetes Mellitus I.H.F.: Ischaemic Heart Failure I.M.: Intramuscularly I.N.R.: International Normalised Ratio I.V.: Intravenously JCMH: James Connolly Memorial Hospital L.D.L.: Low Density Lipids L.F.Ts: Liver Function Tests Lfts: Liver Function tests M.M.S.E.: Mini Mental Score exam M.N.D.: Motor Neuron Disease M.S.U. : Mid Stream Urine specimen M.S.W.: Medical Social Worker MDT: Multi disciplinary team MMUH: Mater Misericordiae University Hospital MRI: Magnetic Resonance Imaging M.R.S.A : Methicillin Resistant Staphylococcus Aureus N.I.D.D.M.: Non Insulin Dependent Diabetes Mellitus N.S.A.I.D.s: Non steroidal anti inflammatory drugs NAD: Nothing Abnormal Detected NFR: Not for ressussitation NPO: Nil per oral Nocte: At night O.A.: Osteoarthritis O.D.: Once daily O.T: Occupational Therapist Obs: Observation chart OLH: Our Lady’s Hospice OLHSC: Our Lady’s Hospital for Sick Children P.E.G.: Percutaneous Endoscopic Gastrostomy P.H.N.: Public Health Nurse P.O: Orally P.R.: Rectally P.R.N.: Pro re nata (when required) P.U.D.: Peptic Ulcer Disease P.V.: Vaginally P.V.D.: Peripheral Vascular Disease P: Pulse PCU: Palliative Care Unit Physio: Physiotherapist Plts: Platelets PSA: Prostatic Specific Antigen PTO: Please turn over Pts: Patients PTT: Partial Thromboplastin Time Q.D.S.: Quarter die sumendus (four times daily) R.A.: Rheumatoid arthritis R.R.: Respiration Rate RGN: Registered General Nurse RRU: Rheumatology Rehabilitation Unit Rx: Treatment S.C.: Subcutaneously S.H.O.: Senior House Officer S.L.: Sublingually S.L.T.: Speech and Language therapy SJH: St James Hospital SLH: St Luke’s Hospital SN: Staff Nurse S.O.P.: Standard Operating Procedure SVPH: St. Vincent’s Private Hospital SVUH: St. Vincent’s University Hospital T.D.S.: Ter die sumendus (three times daily) T.I.A.: Transient Ischaemic Attack T.U.R.P.: Transurethral resection of the prostate Temp: Temperature Tfts: Thyroid Function Tests U&E: Urea and Electrolytes U.R.T.I.: Upper Respiratory Tract Infection U.T.I.: Urinary Tract Infection WCC: White Cell Count