* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Overview of Palliative Care - Scioto County Medical Society
Survey
Document related concepts
Transcript
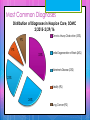
Overview of Palliative Care Suzann Bonzo, MD The Greatest Barrier The greatest barrier to end of life care is Clinicians Due to the lack of confidence in their ability to talk about EOL issues and poor delivery of “bad news” End of Life The last 18 months of life often encompass the longest and most frequent hospitalizations and the most cost. During the last 18 months of life, studies show that patients and families desire to stay home with less aggressive interventions. Today Today is to help us: Understand why Palliative Care originated Be able to discuss the benefits of Palliative Care Be aware of barriers to Palliative Care Understand challenges of Palliative Care Palliative Care in Hospice Initially Hospice and Palliative Care were essentially the same Need to think of a continuum of care Longer period of time Many life limiting diseases End of life is not clearly defined Components of High Quality Palliative Care Pain will be adequately treated Avoid inappropriate prolongation of life Obtain a sense of control Relieving burden Strengthen relationships with loved ones National Consensus Project Quality Palliative Care developed guidelines Structure and process of care Physical aspects Psychological and psychiatric aspects Social aspects Spiritual, religious, and existential aspects Cultural aspects Care of the imminently dying patient Ethical and legal aspects Preferred Practices for Palliative and Hospice Care Handout Make up of the Palliative Care Team The National Consensus Project for Quality Palliative Care recommends that the interdisciplinary palliative care team include palliative care professionals with the appropriate patient- populationspecific education, credentialing, and experience and ability to meet the physical, psychological, social, and spiritual needs of both patient and family. Referrals from PCP to Hospice PCP works directly with Interdisciplinary team of RN, SW, Counselors Manage symptoms and medications Certification for PC/ Hospice Sign death certificates Palliative Care Involves: Trust Overcoming barriers to care and symptom relief Compassionate communication Accurate prognostic information Maintaining hope Eliciting symptoms Decisions regarding curative and palliative treatments Dealing with varying emotions Educating when unrealistic goals are being sought Most Common Diagnoses Distribution of Diagnoses in Hospice Care, 2010 2% 1% 2% 1% 4% Cancer (36%) 0% Heart Disease (14%) Debility, unspecified (13%) 9% 38% Dementia (including Alzheimer's disease) (13%) Lung disease (8%) Stroke or coma (4%) 14% Kidney Disease (2%) Motor neuron diseases (non-ALS) (1%) Liver disease (2%) 14% 15% Amyotrophic lateral sclerosis (0.4%) HIV/AIDS (0.3%) Most Common Diagnoses Distribution of Diagnoses in Hospice Care, SOMC 2/2015-2/29/16 Chronic Airway Obstruction (33%) 9% 9% 33% Senile Degeneration of Brain (26%) Alzheimer's Disease (23%) 23% Debility (9%) 26% Lung Cancer (9%) Benefits of Palliative Care at the End of Life Quality of life Satisfaction with care End of life outcome Family and care-giver perceptions of end of life care Survival advantage (especially in CHF) Cost-effectiveness Challenges in Palliative Care Lack of trained professionals Reimbursement issues Difficulty in prognosis Knowledge and attitude of patients, families, and healthcare providers Comparison: Palliative Care and Hospice Handout Admission Criteria Handout Palliative Care Appropriate Screening Tool Communication in the End of Life Setting One of the most important skills for providers: Disease process Prognosis Likely symptoms and how they will be managed Treatment options and effect on quality of life and length of life Answer difficult questions regarding the dying process Advance care planning Timing of Palliative Care Discussion Earlier than later