* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Infectious Disease Improving Prenatal Care in Vermont Best Practice Provider Toolkit
Behçet's disease wikipedia , lookup
Vaccination wikipedia , lookup
Germ theory of disease wikipedia , lookup
Transmission (medicine) wikipedia , lookup
Hepatitis B wikipedia , lookup
Globalization and disease wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Multiple sclerosis research wikipedia , lookup
Infection control wikipedia , lookup
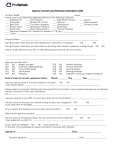
Improving Prenatal Care in Vermont Best Practice Provider Toolkit Infectious Disease Infectious Disease Improvement Checklist Goals (created in 2006 based on best practice guidelines, HP 2010, and/or planning committee consensus) 1. 100% of pregnant women will be offered testing for Gonorrhea and Chlamydia. 2. 100% of pregnant women who are at-risk (either through social factors or positive test) will be offered re-screening/ re-testing for Gonorrhea and Chlamydia by 34 weeks. 3. 100% of pregnant women will be screened for HIV 4. 100% of pregnant women will be offered a flu vaccination while pregnant. 5. 100% of pregnant women will be examined for Periodontal Disease. 6. 90% of pregnant women identified as possibly having Periodontal Disease will be referred for dental care, if available in community. The dental piece was newer for us…Though we always did our exam for dentition, now we’re more interested in following up on that and saying, “Okay, what can we do about this?” (midwife, rural OB practice) We’ve always screened for STDs in the first trimester. The difference now is that we re-screen in second trimester. (midwife, rural OB practice) Sexually Transmitted Infections (Chlamydia, Gonorrhea, Syphilis) The Preventive Screening Task Force and ACOG guidelines recommend screening all pregnant women for common, generally asymptomatic, sexually transmitted infections, such as Gonorrhea and Chlamydia (GC). Other guidelines suggest risk-based screening focusing on age (< 25 years old), behavior (multiple sexual partners or history of STIs) and prevalence of gonorrhea and syphilis in the population. Additionally, women who are found to be at risk and are being screened for sexually transmitted infections during early pregnancy are often not re-screened later in pregnancy, and women at high risk for STIs are generally not counseled about the well recognized, STI-preventive benefits of condom use, even during pregnancy (USPSTF 2010; ACOG 2003). Assess Offer STI testing to all patients at the 1st prenatal visit Screen for asymptomatic bacteriurea Assess for lifestyle factors and the need for re-screening Document if patient declines test Intervene Hand out educational materials at the 1st prenatal visit Treat for positive screens, treat to cure Ensure all sexual partners of infected patients are tested and/or treated presumptively Follow up Repeat GC screening by 34 wks for women at high risk and those previously treated Repeat screening raises the predictive value and is necessary to know that treatment was successful. It is important to re-screen patients who have a prior positive test during pregnancy and re-screen those with lifestyles that put them at-risk Group B Streptococcus (GBS) Assess Screen all patients between 35-36 weeks gestation Follow-up Document results on antenatal form Inform patient of results and if positive implication for treatment during labor Page 2 Human Immunodeficiency Virus (HIV) Early identification of maternal HIV seropositivity allows early antiretroviral treatment to prevent motherto-child transmission, allowing providers to avoid obstetric practices that may increase the risk for transmission, and allows an opportunity to counsel the mother against breastfeeding (USPSTF, 2010). Assess Screen all patients, as part of the prenatal blood work panel Document reason(s) for not testing or if patient opt-out/declines testing Follow-up Document results on antenatal form Inform patient of results. If positive, inform of treatment therapy for labor and treatment for newborn Hepatitis B (Hep B) The ACOG and AAP recommend universal screening for Hepatitis B with the use of Hepatitis B Surface Antigen (HBSAg) and early treatment (within 12 hours of birth) of neonates with HBSAg positive mothers. It is estimated that at least half neonatal Hepatitis B infections may be preventable by use of the maternal test (HBSAg), maternal re-screening when appropriate, and notifying pediatric providers of positive maternal screening in a timely manner. Assess Screen all patients for Hep B infection by testing for HBSAg regardless of previous Hep B vaccine or previous negative test Document Hepatitis (HBSAg) status on all prenatal patients. If maternal status is unknown at the time of delivery, hospital standing orders are such that neonate will receive immunoglobulin within 12 hours. Maternal Hepatitis status must be documented and accessible in prenatal record to avoid unnecessary treatment Document if patient declines newborn treatment Intervene Women with positive HBSAg should be provided with or referred to counseling and appropriate medical treatment Follow-up Ensure Hep B status is documented, on all prenatal charts, at time of admission to labor floor, or in a delivery setting. Women with unknown HBSAg status or with new or continuing risk factors for HBV infection (such as injection drug use or evaluation or treatment for a sexually transmitted infection) should receive screening Influenza Current guidelines place pregnant women in a high risk category concerning influenza and recommend vaccination, regardless of gestational age. Additionally, women with significant chronic diseases should get vaccinated at any point in their pregnancy. Assess Offer every pregnant woman an influenza vaccination regardless of gestational age Intervene Vaccinate pregnant Reassure patient that vaccination is not harmful, even in the first trimester Follow-up If patient referred out of office, ensure vaccination was received Document vaccination even if done out of office Page 3 Periodontal Disease Good oral health and control of oral disease protects a woman’s health and has the potential to reduce the transmission of pathogenic bacteria from mothers to their children. Dental health should be a routine part of the prenatal evaluation. Practices participating in IPCV experienced considerable problems with referring pregnant women for dental care within Vermont. Documentation regarding assessment and the lack of access to dental resources may help provide evidence to assist in the development of effective and available dental care during pregnancy. Access to care is especially challenging for the Medicaid population. This is an important topic for statewide policy development. Assess Screen all patients for periodontal disease by examining the oral cavity at the 1st prenatal visit Intervene Refer for dental care when evidence of periodontal disease is present or suspected or the patient has not had dental care in the last year Refer patients with suspicion of periodontal disease for dental care. Though prenatal care providers may not feel qualified to absolutely determine the presence of periodontal disease in every patient, it is important to refer those who appear to have decay and irritated gums Follow-up Ensure dental care was received Document lack of available resources, if applicable Suggestions for Monitoring Your QI Efforts To assess whether your intended change in practice is occurring and is being documented, regularly (i.e., quarterly) review patient charts within the first and third trimesters for the following indicators: Was patient screened for GC and Chlamydia? Was patient re-tested if positive and/or re-screened if at risk due to social factors by 34 weeks? Is the GBS status of all patients clearly documented on all prenatal records for patients by the 37/38 week? Is the date of influenza vaccination recorded? Did the patient receive an evaluation for periodontal disease? If evidence of periodontal disease found, was referral made for dental care? If resources unavailable was there documentation of this? Is there documentation of HIV results and the opt-out decision noted, if applicable? If patient declined testing for GC and Chlamydia or influenza vaccination, was it documented? Was Hepatitis B Surface Antigen screening performed? Is Hepatitis B Surface Antigen result easily accessible within the prenatal chart? Resources and References — Center for Disease Control and Prevention. STD Treatment Guide. http://www.cdc.gov/std/treatment Assessed May 10, 2011. — Center for Disease Control and Prevention. Hepatitis C FAQs for Health Professionals. http://www.cdc.gov/hepatitis/HCV/HCVfaq.htm Accessed May 3, 2011. — March of Dimes Web site: http://www.marchofdimes.com (English) or http://www.nacersano.org – Page 4 (Spanish). To order a catalog or multiple copies of materials, call 1-800-367-6630. • Prenatal Care (booklet) (also available in Spanish) • Preconception Health Promotion: A Focus for Women's Wellness (nursing education) • High-Risk Antenatal Home Care (nursing education) Guilbeau, J. R., & Hurst, H. Brush Up. Periodontal Disease and Pregnancy. (2010). Nursing for Women’s Health, 13(1), 496-499. – – – – Page 5 Jared, H. & Boggess, K. (2008). Periodontal disease and adverse pregnancy outcomes: A review of the evidence and implications for clinical practice. Journal of Dental Hygiene, 3(summer Suppl.). 3-21. Primary and Preventive Care: Periodic Assessments. American College of Obstetricians and Gynecologists Committee on Gynecologic Practice. Committee Opinion No. 293. November 2003. United States Preventive Services Task Force (USPSTF). Department of Health and Human Service. Guide to Clinical Preventive Services 2010-2011. Washington, DC. http://www.USPreventiveServicesTaskForce.org Accessed May 10, 2011. Vermont Department of Health for current statistics – state or county specific rates of testing and infection Are you pregnant? Have you had your flu shot? Ask your provider for more information. Created by Improving Prenatal Care in Vermont, VCHIP, Burlington, VT. 2011 Page 6 Initial Screening Questions: Hepatitis C Adusumalli J, Bonney EA, Odenat L, Jameison D. Hepatitis C Virus: Prevalence in an inner city urgent care clinic population Infect Dis Obstet Gynecol 2004; 12: 9-12 The purpose of this survey is to determine if an additional blood test might be recommended for you. Please circle “Yes” or “No” in response to the following questions. 1. Have you ever had a blood transfusion or organ transplant? Yes or No 2. Have you ever been on hemodialysis? Yes or No 3. Have you ever been exposed to blood or bodily fluids that were infected with hepatitis C? Yes or No 4. Do you have hepatitis C? Yes or No 5. Have you ever been told that you have hepatitis or that your liver has been functioning abnormally? Yes or No 6. Do you have any tattoos or body piercing? Yes or No 7. Have you had sex with more than 3 people in the past year? Yes or No 8. Have you ever had an infection that you got by having sex (i.e. Chlamydia, gonorrhea, trichomonas, syphilis, HIV, etc)? Yes or No 9. Have you ever used cocaine or illegal intravenous (injectable) drugs? Yes or No Care or Education of Special Groups Centers for Disease Control and Prevention. Sexually Transmitted Disease Treatment Guidelines 2002. MMWR 2002;51(RR06);1-80. Printed by Improving Prenatal Care in Vermont, Vermont Child Health Improvement Program, Burlington, VT. 2005. Last reviewed 2011. Page 7 Nursing Strategies to Improve Maternal Oral Health Consider: • Including oral health information during prenatal care and birth preparation classes • Recommending scheduling a dental appointment before patient becomes pregnant or early in the pregnancy for assessment, prevention and treatment • Explaining that hormones present during pregnancy make gum tissues more susceptible to gum diseases • Looking for and asking about signs of gum disease • Recommending daily plaque removal • Encourage reduction in the risk for premature birth and all oral diseases, including cancer, by quitting smoking • Recommending rinsing with a sodium bicarbonate solution (1/4 teaspoon baking soda in 1 cup warm water) to help neutralize acid to combat the dental effects of frequent vomiting; wait 30 minutes to brush to avoid removal of damaged tooth structure, and strengthen teeth with fluoride toothpaste and mouth wash. • Including oral health in overall health and wellness education • Reminding parents their newborn’s first dental visit should be by 1 year of age • Networking with oral health professionals • Working to ensure nursing educational programs and in-service trainings have a comprehensive oral health component Warning Signs of Periodontal Disease • Red, Swollen or tender gums or other mouth pain • Bleeding while brushing, flossing or eating hard food • Gums that are receding or pulling away from the teeth, causing the teeth to look longer then before • Loose or separating teeth • Pus between the gums or teeth • Sores in mouth • Persistent bad breath • A change in the way teeth fit together when the woman bites down • A change in the fit of partial dentures (Guilbeau, 2010) Page 8