* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Pelvic Examination
Survey
Document related concepts
Transcript
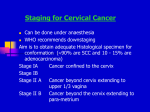
Pelvic Examination Akmal Abbasi, M.D. Cross Section, Side View Pelvic Examination 1. Preparation of the patient: – A. Instruments for pelvic examination: • • • • • • • • 1. 2. 3. 4. 5. 6. 7. 8. examining gloves bivalve speculum (plastic or metal) (various sizes) sponge forceps cotton balls or GYN “cue tips” wooden spatula Cyto brush 2 glass slides or whatever your clinic uses fixative, liquid or spray Pelvic examination • B. Positioning the patient • Raise the patients head so that eye contact is possible. • Put your hand at the end of the table over the sheet and have the patient move down until she feels your hand. • Drape the sheet around the legs and arrange so that you can see the patient and only the perineum is visible. Pelvic examination • Positioning the patient, continued • Tell the patient you are going to touch her and touch her on her leg or thigh • Ask her to move her legs out to “here”-and show her how wide. Pelvic examination • Tips to make the experience tolerable for the patient • Don’t say things like “spread your legs” or “it looks good” • Say “let your legs relax--out to here” and show her and “everything looks healthy” • Try to avoid talking about the “blades” or the speculum (ouch!). Pelvic examination • Tips, continued • Use firm pressure, not a light tickling touch • Talk to the patient and tell her what you are doing. • Look at the patient when you ask her a question, if you can. • But, maintain eye contact and and stay in touch with the patient’s response. • Be sensitive. Examination of External Genitalia A. B. C. D. E. F. G. Clitoris Prepuce Labia majora Labia minora Perineal body Hymen Urethral meatus Examination of External Genitalia H. Vestibule I. Bartholin’s glands (greater vestibular) J. Skene’s glands (paraurethral) K. Lesions, discharge L. Pubic hair pattern External Genitalia • Bartholin’s glands and Skene’s glands are normally non-palpable; swelling and tenderness indicate abnormality (e.g., abscess) • Test for relaxation of supporting structures: • Palpate perineal tone. • Patient is told to hold breath and strain (Valsalva maneuver); involuntary loss of urine; or descent of vaginal wall, or cervix to the introitus indicates abnormality. Inquire about loses of urine with cough or sneeze. Note any inflammation, ulceration of Skene's glands (e.g., from gonorrhea) is suspected, insert your index finger into the vagina and milk the urethra gently from the inside outward. Note any discharge from or about the urethral orifice. If present, a culture should be taken. If there is a history or appearance of labial swelling, check Bartholin's glands. Insert your index finger into the vagina near the posterior end of the introitus. Place your thumb outside the posterior part of the labia majora. On each side in turn palpate between your finger and thumb for swelling or tenderness. Note any discharge exuding from the duct opening of the gland. If present, culture it. Note any surgical scars (episiotomy or other scars) and other abnormalities. Inflammation commonly caused by gonorrhea and may be acute or chronic. Acutely, it is a tense, hot, very tender abscess. Look for pus coming out of the duct. Chronically, a non-tender cyst occupies the posterior labium. It may large or small. Assess the support of the vaginal outlet. With the labia separated by your middle and index finger; ask the pt. to strain down. Note any bulging of the vaginal walls. A cystocele is present when the anterior wall of the vagina, together with the bladder above it, bulges into the vagina and sometimes out the introitus. Look for the bulging vaginal wall as the client strains down. A rectocele is formed by the anterior and downward bulging of the posterior vaginal wall together with the rectum behind it. To identify it, spread the client's labia and ask her to strain down. INTERNAL EXAM INSTRUCTIONS • Inspect the vagina and cervix next using a speculum. • A speculum is placed inside the vagina and opened. • The speculum is an instrument that holds the vaginal walls apart and allows the examiner to see the cervix and vagina and check for inflammation, infection, scars or growths. • There may be some feeling of pressure on the bladder or rectum with the speculum in place. INTERNAL EXAM INSTRUCTIONS • Select a speculum of appropriate size, lubicate it and warm it with warm water. (Other lubricants, such as K-Y Jelly, may interfere with cytological or other studies but they may be used if no such tests are planned.) • By having your speculum ready during assessment of the vaginal outlet, you can ease speculum insertion and increase your efficiency by proceeding to the next maneuver while the pt. is still straining down. Place two fingers just inside or at the introitus and gently press down on the perineal body. With your other hand introduce the closed speculum past your fingers at a 45-degree angle downward. The blades should be held obliquely and the pressure exerted toward the posterior vaginal wall in order to avoid the more sensitive anterior wall and urethra. Be careful not to pull on the pubic hair or to pinch the labia with the speculum. After the speculum has entered the vagina, remove your fingers from the introitus. Rotate the blades of the speculum into a horizontal position maintaining the pressure posteriorly. Open the blades after full insertion and maneuver the speculum so that the cervix comes into full view. When the introitus is retroverted, the cervix points more anteriorly than diagrammed. Position the speculum more anteriorly, i.e., more horizontally, in order to bring the cervix into view. A normal cervix will appear pinkish in color. The cervix will appear as purplish in color if a woman is pregnant. OBTAINING SPECIMEN SAMPLES Pap smear • If you are going to obtain specimens for cervical cytology (Papanicolaou smears, also known as a pap smear). Take these steps in order: • 1. The Endocervical Swab: Moisten the end of a cotton applicator stick with saline and insert it into the os of the cervix. • Roll it between your thumb and index finger, clockwise and counter clockwise. Remove it. Pap smear • Smear a glass slide with the cotton swab, gently in a painting motion. (Rubbing hard on the slide will destroy the cells.) • Place the slide into the ether-alcohol fixative at once. • 2. Cervical Scrape: Place the longer end of the scraper on the os of the cervix. • Press, turn and scrape. Smear on a second slide as before. Pap smear • 3. Vaginal Pool: Roll a cotton applicator stick on the floor of the vagina below the cervix. • Prepare a third slide as before. If the pt. has an infection or a discharge from the cervix or the vagina, this would be a good time to take a sample with a cotton swab for analysis. • If the cervix has been removed, do a vaginal pool and scrape from the cuff of the vagina. Cultures and Wet Mounts • Obtain cultures for GC/clamydia (Gynprobe) • Must use dacron Q tip and turn in os and leave in os at least 20 seconds. • Wet mounts • Trichamonas = Saline • Yeast, Bacterial Vaginosis+- KOH • Determine pH with Nitrazine or pH paper (normal is 4.5 and below) • “Whiff” test for amine odor characteristic of Bacterial Vaginosis BIMANUAL INSPECTION • Perform a bimanual examination. • From a standing position, introduce the index and middle finger of your gloved and lubricated hand into the vagina, again exerting pressure primarily posteriorly. • Your thumb should be abducted, your ring and little fingers flexed into your palm. • Note any nodularity or tenderness in the vaginal wall, including the region of the urethra and bladder anteriorly. BIMANUAL INSPECTION • Identify the cervix, noting its position, shape, size, consistency, regularity, mobility and tenderness. • Palpate the fornix around the cervix. Note that during pregnancy, the cervix will be softer in consistency (like palpating your lips) as compared to nonpregnancy (like the end of your nose). • Place your abdominal hand about midway between the umbilicus and symphysis pubis and press downward toward the pelvic hand. BIMANUAL INSPECTION • Your pelvic hand should be kept in a straight line with your forearm, and inward pressure exerted on the perineum by your flexed fingers. • Support and stabilize your arm by resting your elbow either on your hip or on your knee which is elevated by placing your foot on a stool. • Identify the uterus between your hands and not its size, shape, consistency, mobility, tenderness and masses. • This procedure may cause some discomfort for the client. • Uterine enlargement suggests pregnancy, benign or malignant tumors. Place your abdominal hand on the right lower quadrant, your pelvic hand in the right lateral fornix. Maneuver your abdominal hand downward, and using your pelvic hand for palpation, identify the right ovary and nay masses in the adnexa. Three to five years after menopause, the ovaries have usually atrophied and are no longer palpable. If you can feel an ovary in a post-menopausal woman, suspect an ovarian tumor. Note the size, shape, consistency, mobility and tenderness of any palpable organs or masses. The normal ovary is somewhat tender. Repeat the procedure on the left side. Vaginal-Rectal Exam: • Withdraw your fingers, removing your gloves and throwing them away. • Reglove using fresh, clean gloves. Place lubricant (K-Y Jelly) on internal exam glove. • Then slowly reintroduce your index finger into the vagina, your middle finger into the rectum. • Ask the pt. to strain down as you do this so that her anal sphincter will relax. Vaginal-Rectal Exam: • Tell her that this examination may make her feel as if she has to move her bowels - but, she won't. • Repeat the maneuvers of the bimanual examination, giving special attention to the region behind the cervix which may be accessible only to the rectal finger. • In addition, try to push the uterus backward with your abdominal hand so that your rectal finger can explore as much of the posterior uterine surface as possible. • Check the rectum itself and other nearby structures for any abnormalities. Pelvic Exam Checklist External Genitalia Inspect Palpate Chart Hair distribution X Pattern, amount Labia Majora -Symmetry -Shape -Color -Surface charact eristics X X X X X Stage of development, abnormal symmetry, color, surface lesions Labia Minor -Symmetry -Shape -Color -Surface charact eristics X X X X Same as labia majora X Pelvic Exam Checklist External Genitalia Inspect Palpate Chart Prepuce X Abnormalities Clitoris X Abnormalities in size Urethra & Meatus X X -discharge, redness Skenes (paraurethral) X X -discharge, enlargement Vaginal Orifice (introitus) X X Size--closed, gaping Bartholins (greater vestibular) X X Enlargement , tenderness Pelvic Exam Checklist External Genitalia Inspect Palpate Chart Cystocele X Preset/absent; degree Rectocele X Preset/absent; degree Uterine Dycensus X Preset/absent; degree Perineal Body X Anus X X Tone -hemmorhoids; tone, occult bloodtest Pelvic Exam Checklist Speculus Exam Inspect Vaginal Mucosa X Color, lesions, rugation Cervix -Size -Shape -Color -Symmetry -Surface charact eristics X X X X X X Size, shape, color, color, symmetry, surface charact eristics Eternal Os X Eversion, erosion, color consistency, odor GC/clamydia/culture/w et mount X Done/not done & w hy PAP smear Discharge Palpate Chart Done/not done & w hy X Color, consistency, odor Pelvic Exam Checklist Bimanual Exam Inspect Palpate Chart Vagina X Cysts, masses Cervix -Consistency -Mobility -Tenderness X X X X Soft/firm; mobile/immobile; tender/nontender Supra Pubic X Masses, tenderness Posterior Cul de sac X Masses, tenderness Pelvic Exam Checklist Bimanual Exam Uterus -Size Inspect Palpate X X -Shape -Position X X -Consistency -Mobility -Tenderness X X X Andenexa -Tubes, Ovaries, Ligaments X X Chart Small or w eeks gestation Smooth/irregular Anteverted/flexed, mid, retrovrted/flexed Soft/firm Mobile/immobile Tender/nont ender Enlargement , masses, tenderness Pelvic Exam Checklist Rectovaginal Exam Inspect Palpate Chart Rectovaginal Septus X Thickness Posterior Cul de sac X Masses, tenderness Posterior Uterine Wall X Same as vaginal Adenexae X Same as vaginal Rectal tone X Tone, occult blood test results Pelvic Examination of the Adolescent Patient Remember • The lithotomy position is uncomfortable both physically and psychologically. • Be professional, patient, and gentle. • "Endearing" names for the patient like "honey" or "darlin", though used by some gynecologists, are inappropriate, especially for the adolescent. • Explain ahead of time that the exam, though uncomfortable and embarrassing, should not hurt, and you will stop if it does. Order of Tests 1. External genitalia inspection 2. Insertion of vaginal speculum and identification of cervix (Stay away from the urethra and anterior vaginal wall; downward pressure on the perineal body during insertion is often helpful) 3. Swab cervix clean (if necessary) 4. Endocervical swab for GC culture and endocervical portion of Gram stain slide Order of Tests 5. Endocervical brush for Chlamydia FA and for endocervical component of PAP smear 6. Wooden spatula for ectocervical portion of PAP smear 7. Cotton tip swab of vaginal secretions in posterior fornix for NX Prep, KOH Prep and other portio of Gram stain slide 8. Inspect vaginal wall as you retract the speculum Bimanual Exam 1. Identify cervix with intravaginal gloved examining fingers that have been first covered with sterile lubricant. 2. Assess size and position of uterus using intravaginal examining fingers and abdominal hand 3. Feel adnexal structures bilaterally 4. Rectal exam only if indicated. Bimanual Exam • • • Give the patient tissues or washcloth to clean away the lubricant. Examine slides while your patient is getting dressed. Then discuss the results, your diagnosis, and recommended treatment with her privately after she is dressed. Special Considerations with the Geriatric Patient Geriatric Patient • The pelvic examination proceeds similarly to that of most women. • Special considerations in examining the elderly patient include age-related comorbidities that may make postioning difficult or the examination uncomfortable. • Some of the following recommendations may also apply to younger women with disabilities. Geriatric Patient • Most elderly women can be examined in the dorsal lithotomy position. • For some, conditions that limit hip or knee movement, such as arthritis, make the left lateral decubitus position more comfortable. • With practice, thorough bimanual and speculum examinations can be done with the patient in this position. Geriatric Patient • For bed-bound women, placing an inverted bedpan under the sacrum to elevate the pelvis will facilitate the examination. • The effects of estrogen withdrawal make examination of the vulva particularly important. • After menopause the skin of the vulva loses elasticity and there is degeneration of underlying fat and connective tissues. Geriatric Patient • Inflammation caused by irritants, Candida infection, and vulvar dystrophies are common and treatable and are easily identified on pelvic examination. • Any lesion that is pigmented or does not respond to topical therapy should undergo biopsy. • Atrophic vaginitis is also common and is indicated by the presence of a urethral caruncle or by inflamed vulvar and vaginal tissue. Geriatric Patient • In women who are not receiving estrogen replacement therapy, vaginal stenosis and atrophy are very common. • Small speculums should be used to examine these women. • Lubricant may be necessary for the speculum examination but should be avoided if a Papanicolaou smear is to be obtained. Geriatric Patient • The speculum can be taken apart and the lower half used to hold down the floor and roof of the vagina to look for cystocele and rectocele, respectively, while the patient coughs or performs the Valsalva maneuver. • Urinary leakage with cough or straining may also be observed, indicating stress incontinence. Geriatric Patient • Bimanual examination is important to detect pelvic masses or tenderness. • Any palpable ovarian tissue in a postmenopausal woman warrants further investigation, as does any uterine mass. • Pelvic floor muscle strength and control can be assessed for incontinent patients by having them contract the muscles during digital examination. • This technique can also be used to teach Kegel exercises more effectively. Cystocele, a hernial protrusion of the urinary bladder through the anterior wall of the vagina. Rectocele, a hernial protrusion of part of the rectum through the posterior wall of the vagina. Evaluation of menstrual disorders I. A. 1. 2. 3. 4. 5. 6. 7. History: Components to Document Menstrual specific Age at menarche Frequency and duration of flow Quantity of pads/tampons per day and number periods Last menstrual period Last normal menstrual period Symptoms associated with menses Disruption of normal activities 8. Past treatment A. Past medical history 1. 2. 3. 4. 5. Hospitalization Surgery Serious infections Congenital problems (hydrocephalus) Chronic illness (rheumatologic, endocrinologic, oncologic, gastrointestinal) Tanner/SMR stage Bleeding disorders (epistaxis, hematuria, hematochezia) Previous gynecologic evaluation and treatment Growth Development Family history of gynecologic problems 6. 7. 8. 9. 10. A. 10. A. 1. 2. 3. 4. 5. 6. 7. 8. Development Family history of gynecologic problems Maternal menarche Dysmenorrhea/PMS Endometriosis Malignancy Virilization Ovarian cysts Bleeding disorders Surgical procedures 9. A. 1. 2. 3. 4. 5. 6. 7. A. 1. 2. 3. 4. Fertility problems Medications/substance use Use of contraceptives Steroids Alcohol Others (antianxiety, antidepressants, antipsychotics) Tobacco Marijuana Cocaine Related health issues Weight change Nutrition history Exercise, sports Emotional symptoms • Physical Examination: Specific Elements to Document A. Vital signs 1. Weight 2. Height 3. Blood pressure 4. Heart rate 5. Body mass index A. Tanner stages: B1-B5, P1-P5 B. External signs 1. Acne 2. Acanthosis nigricans 3. Bruising, ecchymosis, petechiae 4. Galactorrhea 5. Hirsutism, virilization 6. Thyroid size C. External genitalia and pelvic exam C. External genitalia and pelvic exam 1. Clitoromegaly a.Clitoral index = transverse diameter (3.4 mm ± 1.0 mm) × longitudinal diameter (5.1 mm ± 1.4 mm) = mean 18.52 mm2 † † Data from Verkauf BS, Von Thron J, O'Brien WF: Clitoral size in normal women. Obstet Gynecol 80:41-44, 1992. b.Enlarged ≥ 35 mm2 2. Evidence of estrogen effect on external genitalia, vaginal epithelium (vaginal smears) (Table 1) 3. Vaginal growths, foreign bodies 4. Cervix: erythema, friability, mucopus, shape of os I. A. 1. 2. 3. 4. 5. Laboratory and Radiologic Tests: Menu to Evaluate Menstrual Disorders Routine Complete blood cell count (CBC) with differential and indices and platelets Erythrocyte sedimentation rate§ § Only if history suggests. Sequential Multiple Analysis 12 (SMA 12) (liver, renal functions)§ Urinalysis and urine culture* Serum or urine pregnancy test¶ ¶ Only if teen is currently sexually active or has a past history of sexual activity. PELVIC INFLAMMATORY DISEASE (PID) Akmal Abbasi, M.D. PELVIC INFLAMMATORY DISEASE • Pelvic inflammatory disease (PID) is defined as a group of disorders that affect the upper genital tract of women. • It is thought to occur by the ascending spread of organisms from the cervix or vagina to the endometrium, fallopian tubes, and contiguous structures. • PID may include any combination of endometritis, salpingitis, tubo-ovarian abscess (TOA), or pelvic peritonitis. Incidence • More than 1 million women contract PID each year, resulting in more than 2.5 million outpatient visits, 200,000 hospitalizations, and 100,000 surgical procedures annually. • More than 25% of women with a history of PID suffer at least one sequela, including infertility, ectopic pregnancy, or chronic abdominal pain. Incidence • Increasing number of adolescents develop this disease. • Nearly 70% of female patients with PID are younger than 25 years of age, with ~33% experiencing their first infection before the age of 20 years. • Adolescents aged 15 to 19 years have the highest incidence of PID compared with all other age groups. ETIOLOGY Chlamydia trachomatis. Neisseria gonorrhoeae. Vaginal aerobes anaerobes Escherichia coli. Haemophilus influenzae. Mycoplasma hominis Ureplasma urealyticum Pathogenesis • • • PID develops when:pathogenic microorganisms ascend from an infected cervix along the endometrial mucosal surface to the uterus and fallopian tubes. N. gonorrhoeae and C. trachomatis may initiate changes in the cervix, endometrium, and tubal mucosa, causing damage and facilitating subsequent anaerobic or facultative bacterial invasion. Pathogenesis • Other mechanisms in the development of PID may include lymphatic drainage with spread of the infection parametrially or the adherence of N. gonorrhoeae, C. trachomatis, or other bacteria to spermatozoa that may spread through the genital tract. Pathogenesis • • The normal flora of the vagina consists predominantly of Lactobacillus sp., which are believed to be responsible for regulating the growth of the vaginal flora. Lactobacilli sp. produce hydrogen peroxide and are also responsible for the presence of a low vaginal pH level that may inhibit the growth of other microorganisms Pathogenesis • Bacterial vaginosis is a clinical syndrome caused by an overgrowth of endogenous and anaerobic flora. • A shift in the vaginal flora occurs from a predominance of Lactobacillus flora to one characterized by high concentrations of G. vaginalis, anaerobic bacteria, and genital mycoplasmas. • Bacterial vaginosis-associated organisms include G. vaginalis, Bacteroides sp., anaerobic cocci, Mobiluncus sp., M. hominis, and U. urealyticum. Pathogenesis • The endocervical canal and mucus plug within the endocervix represent the major barriers that protect the endometrium and the rest of the upper genital tract from the vaginal flora. • Changes in the composition of the normal vaginal flora and a failure of the barrier function at the cervical-vaginal interface may allow the ascendance of lower genital tract flora into the endometrial cavity and contiguous structures. Pathogenesis • Infection may also diminish the clearance mechanism normally provided by the ciliary epithelial cells of the uterine and fallopian tubes. RISK FACTORS--Age • Teenagers , especially those who are sexually active. • Sexually experienced teenagers are three times more likely to be diagnosed with PID than are 25- to 29 year olds. Menstrual Cycle Influences: • Symptoms of PID frequently present within the first 7 days of the menstrual cycle, especially in association with N. gonorrhoeae infection. • This may suggest that organisms are transmitted from the cervix to the upper genital tract at the time of menses. Sexual Behavior: • • Behaviorally, adolescents have more sexual partners per time period, tend to be inconsistent in the use of barrier methods of protection, and have a higher prevalence of STDs in the partner pool. A higher frequency of sexual intercourse and an increased rate of acquiring unprotected, new partners are also risk factors for PID. Choice of Contraceptive: • Barrier methods, including condoms, spermicides, and diaphragms, reduce the risk for PID . • IUD increase the risk for PID, although this risk seems to be highest in the first 4 months after IUD placement and not significantly elevated above baseline at 5 months follow-up and beyond. • In these cases, PID is probably caused by the introduction of vaginal or cervical organisms into the uterus at the time of intrauterine device insertion. Other Risk Factors: • Women who have had previous episodes of Gonococcal PID are more likely to have recurrent PID involving any cause. • Douching may increase the risk for PID by altering the vaginal environment to one that is less protective against pathogenic organisms. • Another theory is that douching flushes vaginal and cervical microorganisms into the uterine cavity, thus increasing the risk for upper genital tract infection. SYMPTOMS Lower abdominal pain (1wk post menses). Adnormal vaginal discharge. Poscoital bleeding. Spotting between menses. N/V/diarrhea. Fever/chills. Dyspareunia. CLINICAL FINDINGS Fever, Lower abd. pain with rebound. CMT Adenexal tenderness. Adenexal fullness/mass. Lab evaluation Urine and/or serum CBC ESR Chlamydia and GC. HCG. DIAGNOSTIC EVALUATION Ultrasound. To R/O tubo-ovarian abscess. Laporoscopy gold standard for diagnosis. Endometrial biopsy to r/o endometritis. RECOMMENDATIONS FOR CRITERIA USED TO DIAGNOSE PID • Minimum criteria: Lower abdominal tenderness Adnexal tenderness Cervical motion tenderness • Additional criteria Oral temperature >101°F Abnormal cervical or vaginal discharge Elevated erythrocyte sedimentation rate Elevated C-reactive protein Lab documentation of cervical infection with N. gonorrhoeae or C. trachomatic RECOMMENDATIONS FOR CRITERIA USED TO DIAGNOSE PID • Elaborate criteria: Histopathologic evidence of endometritis on endometrial biopsy Transvaginal sonography or other imaging techniques showing thickened, fluid-filled tubes with or without free pelvic fluid or tubo-ovarian complex Laparoscopic abnormalities consistent with pelvic inflammatory disease DDX Ectopic pregnancy. Appendicitis. Chronic pelvic pain. Chronic adhesive disease. Endometriosis. Ovarian torsion. Ovarian cyst. IBS SEQUELAE • The sequelae of PID are a major cause of reproductive morbidity and can occur in as many as 25% of women with PID. • Infertility • Ectopic pregnancy • Recurrent PID • Chronic abdominal pain • Dyspareunia • Pelvic adhesions • Pyosalpinx • Tubo-Ovarian Abscess RECOMMENDATIONS FOR HOSPITALIZATION OF PATIENTS WITH SUSPECTED PID • Uncertain diagnosis (surgical emergencies cannot be excluded) • Pregnancy • Failure to respond clinically to oral antimicrobial therapy • Noncompliance (unable to follow outpatient regimen) • Severe illness, nausea, and vomiting; or high fever • Unable to tolerate an outpatient oral regimen • Tubo-ovarian abscess is present • Immunodeficiency or HIV positivity RECOMMENDATIONS FOR OUTPATIENT TREATMENT OF PID • Regimen A Ofloxacin, 400 mg PO BID for 14 days Plus Metronidazole, 500 mg PO BID for 14 days RECOMMENDATIONS FOR OUTPATIENT TREATMENT OF PID • Regimen B Ceftriaxone, 250 mg IM QD Or Cefoxitin, 2 g IM, plus Probenecid, 1 g orally in a single dose Or Other parenteral third-generation cephalosporin Plus Doxycycline, 100 mg PO BID for 14 days RECOMMENDATIONS FOR INPATIENT TREATMENT OF PID • Regimen A Cefotetan, 2 g IV every 12 hours Or Cefoxitin, 2 g IV every 6 hours plus Doxycycline, 100 mg IV or orally every 12 hours RECOMMENDATIONS FOR INPATIENT TREATMENT OF PID • Regimen B Clindamycin, 900 mg IV every 8 hours Plus Gentamicin, 1.5 mg/kg IV every 8 hours (load 2 mg/kg IV or IM first dose) ALTERNATIVE PARENTERAL REGIMENS FOR INPATIENT TREATMENT OFPID • Regimen A Ofloxacin, 400 mg IV every 12 hours Plus Metronidazole, 500 mg IV every 8 hours • Regimen B Ampicillin/Sulbactam, 3 g IV every 6 hours Plus Doxycycline, 100 mg IV or orally every 12 hours ALTERNATIVE PARENTERAL REGIMENS FOR INPATIENT TREATMENT OFPID • Regimen C Ciprofloxacin, 200 mg IV every 12 hours Plus Doxycycline, 100 mg IV or orally every 12 hours Plus Metronidazole, 500 mg IV every 8 hours PATIENT COUNSELING • Counseling should provide an adequate opportunity to discuss contraception, especially the use of barrier methods, to prevent the transmission of STDs. • Other potentially health-compromising behaviors, such as douching, should be addressed. PATIENT COUNSELING • Patients should be instructed to avoid intercourse while ill with symptoms and while being treated. • They should be encouraged to discuss treatment with their partners and to verify that their partners have been treated before reinitiating sexual intercourse. Puberty Akmal Abbasi, M.D. Puberty • Between 10 and 20 yr of age, children undergo rapid changes in body size, shape, physiology, and psychologic and social functioning. • Hormones set the developmental agenda in conjunction with social structures designed to foster the transition from childhood to adulthood. • Adolescence proceeds across three distinct periods—early, middle, and late—each marked by a characteristic set of salient biologic, psychologic, and social issues. • Gender and subculture profoundly affect the developmental course, as do physical and social stressors such as cerebral palsy or parental alcoholism. Puberty • Levels of luteinizing hormone (LH) and folliclestimulating hormone (FSH) rise progressively throughout middle childhood without dramatic effect. • The rapid changes of puberty begin with increased sensitivity of the pituitary to gonadotropin-releasing hormone (GnRH), pulsatile release of GnRH, LH, and FSH during sleep, and corresponding increases in gonadal androgens and estrogens. • The triggers for these changes are incompletely understood, but may involve neuronal development that is ongoing throughout middle childhood and adolescence. Puberty • Children in the United States may enter puberty earlier than the published norms (although reports of dramatically earlier puberty are controversial), perhaps related to increased weight and adiposity. The resulting sequence of somatic and physiologic changes gives rise to the sexual maturity rating (SMR) or Tanner stages. Puberty-Girls • In girls, the first visible sign of puberty is the appearance of breast buds, between 8 and 13 yr. • Menses typically begin 2–21/2 yr later (normal range 9–16 yr), around the peak in height velocity. • Less obvious changes include enlargement of the ovaries, uterus, labia, and clitoris; thickening of endometrium and the vaginal mucosa; and increased vaginal glycogen, predisposing to yeast infections. Puberty-Boys • In boys, testicular enlargement begins as early as 91/2 yr. • Peak growth occurs when testis volumes reach approximately 9–10 cm3 . • Under the influence of LH and testosterone, the seminiferous tubules, epididymis, seminal vesicles, and prostate enlarge. • The left testis normally is lower than the right; the opposite may be true in situs inversus. • Some degree of breast hypertrophy occurs in 40–65% of pubertal boys as a result of a relative excess of estrogenic stimulation. Puberty-Boys • Gynecomastia sufficient to cause embarrassment and social disability occurs in fewer than 10%. Breast swelling less than 4 cm in diameter has a 90% chance of spontaneous resolution within 3 yr. • For greater degrees of enlargement, hormonal or surgical treatment may be indicated. • Obesity may exacerbate gynecomastia and should be addressed through diet and exercise. Puberty • For both sexes, growth acceleration begins in early adolescence, but peak growth velocities are not reached until SMR3 or 4. • Boys typically peak 2–3 yr later than girls and continue their linear growth for approximately 2–3 yr after girls have stopped. • The growth spurt begins distally, with enlargement of hands and feet followed by the arms and legs and finally by the trunk and chest. • This asymmetric growth gives young adolescents a gawky look. • Rapid enlargement of the larynx, pharynx, and lungs leads to changes in vocal quality, often heralded by a period of vocal instability (voice cracking) or dysphonation. Puberty • Adrenal androgens stimulate the sebaceous glands, promoting the development of acne. • Elongation of the optic globe often results in nearsightedness. • Dental changes include jaw growth, loss of the final deciduous teeth, and eruption of the permanent cuspids, premolars, and finally molars. Orthodontic appliances may be needed. Maturity Stages in Girls SMR Stage Pubic Hair Breasts 1 Preadolescent Preadolescent 2 Sparse, lightly pigmented, straight, medial border of labia Breast and papilla elevated as small mound; areolar diameter increased 3 Darker, beginning to curl, increased amount Breast and areola enlarged, no contour separation 4 Coarse, curly, abundant but amount less than in adult Areola and papilla form secondary mound 5 Adult feminine triangle, spread to medial surface of thighs Mature, nipple projects, areola part of general breast contour Sex maturity ratings of breast changes in adolescent girls. Sex maturity ratings of pubic hair changes in adolescent boys and girls. Maturity Stages in Boys SMR Stage Pubic Hair Penis Testes 1 none Preadolescent Preadolescent 2 Scanty, long, slightly Slight enlargement pigmented Enlarged scrotum, pink, texture altered 3 Darker, starts to curl, small amount Longer Longer 4 Resembles adult type but less in quantity; coarse, curly Larger; glans and breadth increase in size Larger, scrotum dark 5 Adult distribution, spread to medial surface of thighs Adult size Evaluation of precocious puberty, excluding factitious and iatrogenic causes. Evaluation of patient with delayed puberty. Sexual Assault Akmal Abbasi, M.D. • Traditionally, rape was defined as the carnal knowledge of a woman, forcibly and against her will. • Most legal reforms have expanded this definition to include many different types of sexual assault such as sodomy, oral copulation, rape with a foreign object, and sexual battery. • Emergency personnel must be well prepared to handle the evaluation and treatment of sexual assault victims. • Training should emphasize the need to maintain patient comfort and support, while approaching patients in a caring and sensitive manner. • A patronizing, dismissive, or accusatory attitude may so alienate the victim that further evaluation or even needed treatment is refused. • The patient’s anxieties may be lessened by specifically acknowledging the assault and by encouraging her expression of her feelings, concerns, and needs. • Step-by-step explanations of any necessary procedures should be provided as the evaluation progresses. • The procedure should also include informing the patient of her rights and options and allowing her to participate in decisions affecting her care. • Prepackaged sexual assault or rape kits are available in the ED or can be obtained from the law enforcement agency where the incident occurred. • These kits contain instructions that guide the examiner, in a stepwise fashion, through the forensic evaluation process. • The kit contains instructions and materials needed to collect, label, and preserve all the required specimens. • Kits may also contain forms designed for the documentation of history and examination findings, as well as specialized consent forms required for evidence collection. Legal Issues • Although the law may not require victims to personally report the crime, most states require physicians to report the alleged sexual assault to the local law enforcement agency in the jurisdiction where the crime occurred. • Reporting requirements generally include the victim’s name and address, the nature and extent of injuries, and the location of the assault. • The victim should be informed of this physician responsibility and told that her decision regarding the report of the assault does not affect her access to medical care and other supportive services. Legal Issues • Patient’s legal rights regarding any examination, treatment, or evidence collection must be preserved because she may refuse or withdraw consent from any or all parts of the evaluation process at any time. • To protect both patients and examiners, signed informed consents must be obtained before the examination. • This may require obtaining consent from a parent or legal guardian if the patient is a minor. • A general consent in accordance with hospital policy is all that is required for routine medical evaluation and treatment. • Special and separate informed written consent must be obtained for the collection and release of forensic evidence, including any photographs taken. Recommended History • • • • • • • General medical history Acute injury or illness Chronic disease • Psychiatric disorders Preexisting injuries Current medications Allergies Immunizations • Tetanus • Hepatitis B Recommended History • • • • • • • • Gynecologic history Gravidity and parity Last normal menstrual period Last voluntary intercourse Birth control • Possibility of missed birth control pills Possible symptoms of pregnancy Recent gynecologic surgery Sexually transmitted diseases Recommended History History of the assault • • • • • • • • • • • • • • • Date, time, and place Number and race of assailants Types of force and threats used Use of alcohol or drugs By victim By assailant(s) Loss of consciousness Type of assault Fondling Oral penetration Vaginal penetration Anal penetration Foreign bodies used Ejaculation on or in the body Recommended History • • • • • • • • • Type of assault Fondling Oral penetration Vaginal penetration Anal penetration Foreign bodies used Ejaculation on or in the body Use of condoms Use of a lubricant Recommended History • • • • • • • • • Postassault activity Medications Alcohol or drug use Change of clothing Urination or defecation Bathing, washing, douching Eating, drinking Brushing teeth, mouthwash Tampon use Physical Examination • The physical examination is done to identify and treat injuries and to collect forensic evidence for prosecution. • If the patient refuses consent for evidence collection, it is still important to do a complete medical examination and to document physical findings. • This documentation may be used later as evidence. • If the assault occurred within 72 hours, a complete evidentiary examination should be done. If more than 72 hours have passed, a full physical examination and a modified evidentiary examination are indicated because there may still be value in obtaining cervical samples for the presence of sperm. • It is imperative to maintain patient comfort and avoid further psychological pain throughout the examination. Physical Examination • The physical examination is done to identify and treat injuries and to collect forensic evidence for prosecution. • If the patient refuses consent for evidence collection, it is still important to do a complete medical examination and to document physical findings. • This documentation may be used later as evidence. • If the assault occurred within 72 hours, a complete evidentiary examination should be done. If more than 72 hours have passed, a full physical examination and a modified evidentiary examination are indicated because there may still be value in obtaining cervical samples for the presence of sperm. • It is imperative to maintain patient comfort and avoid further psychological pain throughout the examination. Physical Examination • It is recommended that patients remain clothed until the actual examination begins. If possible, the victim should be photographed in the clothing worn during the assault. • The patient should remove her own clothing while standing on clean paper provided in the sexual assault kit, all of which must be submitted to the crime laboratory in paper bags. • If she needs assistance to remove her clothing, gloves should be worn by medical personnel. Approximately 80% of the population secrete ABO blood group antigens in their other body fluids including perspiration, saliva, semen, and vaginal fluid. • Gloves prevent cross-contamination from any perspiration on the hands of medical personnel to the clothes of the victim. • Next, a thorough head-to-toe scan of the victim should be performed to look for any signs of injury or foreign material. • Nongenital injuries occur between 20% and 50% of the time in sexual assaults, more than 80% of these are minor abrasions or contusions. • The most common areas of injury are the head, neck, and upper extremities. • Samples of any foreign material should be gathered on clean paper and properly placed in collection envelopes. • Dried stains (possibly secretions or semen from the assailant) should be collected using water-moistened swabs and the swabs air dried for 60 minutes before placement in collection envelopes. • Visual examination can be aided by using long-wave ultraviolet light (Wood’s lamp) in a darkened room. • Most semen stains will fluoresce under ultravioletlight, but fluorescent stains are not specific to seminal fluid and can be caused by many substances including urine. • Rope marks, recent contusions, and other subtle injuries may also be more visible with the aid of a Wood’s lamp. • The pelvic examination should be performed with the patient in the lithotomy position. • A Wood’s lamp may be used again to examine the inner thighs and perineum. • The condition of the hymen and any signs of trauma to the introitus should be documented. • Evaluations of women without prior sexual experience have revealed significantly more sites of genital injury than those with prior experience. • The posterior commissure is a common site of injury with forced penetration in both groups. • Lower vaginal lacerations are most common in virgin women. • If a tampon is in place, it should be removed, air dried for 60 minutes, and saved in a paper bag or collection envelope because it may contain seminal fluid, blood, or other foreign substances. • To avoid the loss of evidence from the perineal area by voiding, wiping, or washing, an attempt should be made to have the patient delay voiding until the examination is completed. • If the patient is too uncomfortable to undergo an adequate examination before voiding, the patient can void but the urine should be collected so that it may be analyzed for sperm. • Also save any tissue used for wiping so that it may be submitted and analyzed with the other evidence. • Any visible bite marks should be photographed and then swabbed using only distilled water for moistening. • If indicated by the history or examination, fingernail scrapings should be collected at this time. • Saliva samples can be obtained while examining the oral cavity for injuries. Swabs of the mouth may be indicated for seminal fluid up to 6 hours after assault. • A nonlubricated speculum moistened only with water should be used for the vaginal examination because lubricants interfere with specimen drying and analysis. • The vaginal walls should be examined for lacerations and any evidence of foreign body penetration. • More subtle signs of recent sexual activity include erythema of the posterior fourchette and superficial abrasions of the vagina. • After the visual examination, vaginal secretions must be aspirated or collected on swabs from the posterior fornix. • If no secretions are seen, normal saline can be instilled and then aspirated to help collect any seminal fluid. • This fluid can then be examined for sperm, acid phosphatase, and ABO blood group antigens. • Depending on local protocol, a wet mount slide may be studied for motile sperm; however, it is preferable to have this performed by forensic specialists rather than the clinician to improve diagnostic accuracy. • Failure to demonstrate sperm does not exclude the possibility of sexual assault. • The absence of sperm may be due to several factors, including poor evidence collection or examination skills, condom use, and a vasectomy or sexual dysfunction in the assailant. • It is unnecessary to obtain samples from the cervix unless the assault occurred more than 24 hours from the time the patient is examined in the ED. • A standard bimanual pelvic examination should follow to evaluate uterine size, adnexal tenderness, or masses. • The rectal area must also be carefully examined. Any signs of trauma to the buttocks, perianal skin, and anal folds should be documented. • Semen stains, lubricant, or other foreign material are scanned for and samples collected as indicated. If the patient reports anal penetration during the attack, rectal swabs should also be obtained. • The swabs must be collected by a method that does not allow contamination with any material present on the perianal area. • This is best accomplished by swabbing through a nonlubricated anal speculum moistened with water. • The swabs may be analyzed for the presence of sperm and acid phosphatase. • An alternative method is to instill 5 to 10 ml of normal saline into the rectum, allow it to equilibrate for 5 minutes, and then aspirate. • A proctoscopic examination is recommended when significant rectal trauma is suspected. Psychological Effects of Sexual Assault • The rape trauma syndrome is a two-phase syndrome of behavioral, somatic, and psychological reactions that occur as a result of being exposed to an act of violence, in this case sexual assault. • Many symptoms of the rape trauma syndrome also fit the diagnostic criteria for posttraumatic stress disorder. • • • • • • • Psychological Effects of Sexual TheAssault acute phase, which is one of disorganization, begins immediately and may last for several months. In this phase patients may initially react in either an expressive or a controlled manner. Expressive patients may demonstrate feelings of fear, anger, and anxiety through such behavior as crying, tenseness, or restlessness. In the controlled style, the patient masks her feelings and appears calm and composed. During the acute phase it is essential that the victim be accepted, believed, understood, and made to feel safe, while regaining a sense of control over her life. Victims in this phase may demonstrate a wide range of emotions from humiliation and self-blame to anger and revenge. Psychosomatic reactions commonly occur in this phase as well. Psychological Effects of Sexual Assault • The long-term reorganizational phase begins in approximately 2 to 3 weeks and may last indefinitely. • It is the phase in which victims develop coping mechanisms and eventual recovery. • Many victims attempt lifestyle changes by altering daily routines, residences, or telephone numbers, and some turn to alcohol or drugs. • Nightmares and phobias commonly occur, and sexual dysfunction, which may become chronic, is common. • It is reported that 50% to 80% of women who have been raped lose their husbands or boyfriends after the assault. • Because family members are also victimized by the assault, they may experience some of the same psychological effects as the patient. • Appropriate referrals for support services should be given to them as well. Menopause Akmal Abbasi Definition • Menopause is the transition period in a woman's life when the ovaries stop producing eggs, the body decreases the production of the female hormones estrogen and progesterone, and menstrual activity diminishes and eventually ceases. Causes, incidence, and risk factors • Menopause is a natural event which normally occurs between the ages of 45 and 55, beginning, on average, at age 51. • During menopause, ovulation (egg production) stops and menstruation becomes less frequent, eventually stopping altogether. • The symptoms of menopause are caused by changes in estrogen and progesterone levels. • As the ovaries become less functional, they produce less of these hormones and the body responds accordingly. Causes, incidence, and risk factors • In some women, menstrual flow comes to a sudden halt. • More commonly, however, it tapers off, both in amount and duration of flow. • During this time, often called perimenopause, menstrual periods generally become either more closely or more widely spaced. • This irregularity may last for 1 to 3 years before menstruation finally ends completely. Symptoms • The potential symptoms of menopause, which can last from 1 to 3 years, include: • Hot flashes and skin flushing • Night sweats • Insomnia • Mood changes including frequent swings of irritability, depression, and anxiety • Irregular menstrual periods • Spotting of blood in between periods Symptoms • • • • • Vaginal dryness and painful sexual intercourse Decreased sex drive Vaginal infections Urinary tract infections In addition, the long-term risks of menopause include: • Bone loss and eventual osteoporosis • Changes in cholesterol levels and heart disease Signs and tests • Blood and urine tests can be used to measure hormone levels that may indicate when a woman is close to menopause or has already gone through menopause, for e.g. • Estradiol • FSH, LH • A Pap smear may indicate changes in the vaginal lining caused by changes in estrogen levels. • A bone density test may be performed to screen for low bone density levels seen with osteoporosis. Treatment • Menopause is a natural process. It does not necessarily require treatment unless menopausal symptoms, such as hot flashes or vaginal dryness, are particularly bothersome. • HORMONE REPLACEMENT THERAPY • For years, hormone replacement therapy (HRT) was the main treatment for menopause symptoms. • Many physicians believed that HRT was not only the best treatment available for reducing menopausal symptoms, but also reduced the risk of heart disease and bone fractures from osteoporosis. Treatment • However, the results of a major study -- called the Women's Health Initiative (WHI) -- has led physicians to revise their recommendations regarding HRT. • In fact, one part of this important study was stopped early because the health risks outweighed the health benefits for women taking both estrogen and progesterone. • Women taking both of these hormones did see benefit as far as their bones were concerned. Treatment • However, they greatly increased their risk for breast cancer, heart attacks, strokes, and blood clots. • If the symptoms are severe, may still want to consider HRT for short-term use (two to four years) to reduce vaginal dryness, hot flashes, and other symptoms. • To reduce the risks of estrogen replacement therapy and still gain the benefits of the treatment, may use estrogen/progesterone regimens that do not contain the form of progesterone used in this arm of the study. Treatment • Using a lower dose of estrogen or a different estrogen preparation (for instance, a vaginal cream rather than a pill). • There are also some medications available to help with mood swings, hot flashes and other symptoms. These include low doses of antidepressants such as paroxetine (Paxil), venlafaxine (Effexor) and fluoxetine (Prozac), or clonidine, which normally used to control high blood pressure. Prevention • Menopause is a natural and expected part of a woman's development and does not need to be prevented. However, there are ways to reduce or eliminate some of the symptoms that accompany menopause. • NO SMOKING. • Exercise regularly, including activity against the resistance of gravity, to strengthen your bones. • Low-fat diet, calcium and vitamin D. • Control blood pressure, cholesterol, and other risk factors for heart disease.