* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download STD_PRACTICAL
HIV and pregnancy wikipedia , lookup
Diseases of poverty wikipedia , lookup
Herpes simplex research wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Public health genomics wikipedia , lookup
Prenatal testing wikipedia , lookup
Infection control wikipedia , lookup
Canine parvovirus wikipedia , lookup
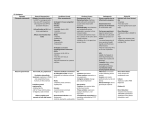
Reproductive block 2015 Prof kambal Dr.Ali M Somily Dr.Malak El-Hazmi Objectives Name various etiological agents causing sexually transmitted diseases Describe the clinical presentations of sexually transmitted diseases Discuss the microbiological and no microbiological methods for diagnosis of sexually transmitted diseases Outline the management of sexually transmitted diseases . Four Classes of STD’s 1- VirusesHerps HIV Hepatitis B Human papilloma virus 2- Bacterial Syphilis Gonorrhea Chlamydia Chancroid Mycoplasma hominis Ureaplasma urealyticum 3- Fungus Yeast – Candida albicans 4- Parasites Trichomonas Ectoparasites Phithrus pubis Pubic louse Sarcoptes scabiei Bacterial STDs Case 1 A 23-year-old alcoholic and drugs (cocaine) addict single male arrived from his trip to South East Asia six months ago. He gave history of multiple sexual partners. Two months ago he developed ulcer on his penis which disappeared compeletly. A full physical notes a rash on both her palms and her soles ? What are the possible causes for his presentation Treponema Pallidum Herpes Simplex Virus 2 Haemophilus Ducreyi How could you differentiate between them based on s/s of the patient? Ulcer Etiology Ulcer Lymphadeno pathy (Babo) Systemic Chancroid Haemophilus Ducreyi Wet , painful Inguinal tender Present Chancer Treponema Pallidum Dry, painless and raised margin Inguinal part of Depends on generalize stage disease Ulcerated Vesicles Herpes Simplex Virus 2 Multiple Occasionally shallow painful present In primary syphilis is a disease caused by a corkscrew-shaped bacterium (a spirochete) called Treponema pallidum. It causes disease when it penetrates broken skin of the genitals or the mucous membranes of the mouth or anus. It can also be passed from an infected person through an open cut or wound and from mother to child. Symptoms: 3-staged disease Primary syphilis Painless penile chancre in primary syphilis due to Treponema pallidum: primary syphilis infection vagina ulcers The lesion are sampled and identified through dark-field microscopy 2nd stage - or secondary syphilis . This stage occurs in about 6-8 weeks after formation of sore if the chancre is not marked and the patient untreated Typically, general signs appear: fever, the aches , headache , a tiredness , a rash as well as lesions on the palms of the hands and soles (feet), glossitis (lesions in the tongue), the lesions contain the bacteria, they are highly contagious secondary syphilis. A B Mucous patches (A and B) are superficial mucosal erosions seen in secondary syphilis. They can be found on any mucosal surface and are highly infectious Base on the finding, what is the most likely diagnosis? Briefly outline the management of this patient? Dx; Primary syphilis Rx; Benzathine penicillin IM---allergy Doxycycline Patient Counseling and Education He should be tested for other STD especially HIV 3rd stage or Tertiary / Acute stage This is the final stage in which the symptoms show no or minor cure despite seeking treatment. Syphilis symptom if left untreated it will then continue and often goes on to damage the nervous system and the heart, weakens bones & joints leading to death None of these third stage gummas or ulcers will heal to their original state Tertiary / Acute stage In the central nervous system it can affect the spinal column, resulting in a condition called tabes dorsalis. This condition causes postural instability with a staggering wide base gait that can damage the joints of the leg. The condition shown is called Charcot's knee. tertiary syphilis with gumma distruction of nose Identification of T. pallidum - Direct Microscopy Dark field showing Treponema pallidum: A dark field analysis of fluid from a lesion of primary or secondary syphilis is considered the gold standard for diagnosing syphilis Silver Stain Spirochetes may be seen in biopsy specimens of suspicious lesions such as palmar macular rash or gummatous lesions Case 1: A 36-year-old female presented with a chief complaint of rash all over the body, of 15 days duration, associated with severe itching. On detailed history, the patient stated that the rash started asymptomatic on the right forearm, and later became generalized. The patient applied some native medications and developed generalized itching and presented with a picture of contact irritant dermatitis in the form of papules, vesicles, and scaling, all over the body. The patient was treated for the same with a combination of topical steroids and antihistamines. The patient had little symptomatic relief with this. The patient's rash was persistent in the form of macules, papules, and scaling. A thorough examination revealed the presence of few lesions on the genitalia mainly on the labia majora which were flat topped papules and the patient also had a mucous patch over the hard palate [. Thus, secondary syphilis was strongly suspected and the patient was subjected for Venereal Disease Research Laboratory (VDRL) testing. The VDRL testing was non-reactive. As the suspicion of secondary syphilis was high As the suspicion of secondary syphilis was high, what further evaluation would you request to exclude or confirm syphilis? -Request for repeat VDRL test, with higher dilution as false negative results will occur due to. Prozone phenomenon in the excess of antibody( high concenteration in serum) - Also request specific Treponemal antigen tests e.g. FTA-Abs , ELIS - Briefly outline the management of this patient secondary treatment consists in two intramuscular of penicillin injections at weekly intervals. treatment effectiveness will be verified on the serology at : 3, 6 , 12 month for the drop of titers. Discussion Prozone phenomenon is an immunological event, relying on an antigen-antibody interaction such as in rapid plasma reagin (RPR) or VDRL. [3] An agglutination or precipitation reaction will be positive (i.e., visible through lattice formation) when the optimal ratio of the antigen antibody yields an insoluble precipitate that is visible, thus rendering the test positive. [4] The zone of equivalence defines this optimal ratio. In the zone of the antibody excess (prozone) or antigen excess (post zone), false negative results will occur. [4] The prozone phenomenon in the setting of syphilis may become prevalent because of the current acquired immunodeficiency syndrome (AIDS) epidemic. [2] As syphilis and HIV mutually increase the chance of contracting other diseases, B-cell behavior can lead to hyper-responsiveness to antigenic stimulation, leading to excess antibody production. [5] Treatment of syphilis The treatment of syphilis is variable depending on the stage of the disease: At the primary stage: the minute treatment: a single injection of penicillin 2.4 million iu intramuscularly (except againstindication) is made and the patient will be cured once the canker is gone, it will not secondary syphilis or tertiary. Stage secondary treatment consists in two 2.4 million iu intramuscular injections at weekly intervals. Syphilis will also be cured, treatment effectiveness will be verified on the serology. In the tertiary stage, the treatment is longer. The effectiveness of treatment is monitored on the evolution of HIV Case 2 A 35-year-old Pilipino married male presented to the emergency room complaining of dysuria for the last 24-hour and noted some "pus-like" drainage in his underwear and the tip of his penis. Urethral Discharge in Gonorrhea) Ophthalmia : 2-7 days after birth with Bloody, green or serosanguineous discharge What are the possible causes for his presentation? Organisms Urethritis Gonococcal Urethritis Neisseria gonorrhoeae Purulent discharge Non-gonococcal urethritis Chlamydia trachomatis Mucopurulent Others •Trichomonas vaginatis •Mycoplasma genitalium What investigations do you like to order for him? Explain how those investigations would help you? GCU Organisms Smear/Culture Neisseria gonorrhoeae Gram-ve diplococci & cellpus / Selective media NGCU Chlamydia trachomatis Others Trichomonas vaginalis Mycoplasma genitalium Immunological tests Molecular testing +ve Pus cell/McCoy Cell culture DFA +ve Wet mount; pus &TV/ Culture Pus cell / Special media culture EIA +ve EIA +ve This Gram-stained specimen from uretheral discharge reveals N. gonorrhoeae intracellular diplococci, leading to a positive diagnosis of gonorrhea Base on the finding, what is the most likely diagnosis? Briefly outline the management of this patient? Symptoms In both genders, gonorrhea spreads through the bloodstream to other organs, causing infection and inflammation of the joints (gonococcal arthritis), the heart (gonococcal endocarditis), or covering the brain (gonococcal meningitis). Some adults get eye infections by rubbing eyes after touching infected genitals Neisseria gonorrhoeae growing on heated blood agar (Chocolate Agar) Neisseria gonorrhoeae requires a rich growth medium, such as heated blood agar (Chocolate Agar) and an atmosphere containing 5-10% carbon dioxide. Even so, it may take up to 48 hours to get colonies of the size seen above. G.C. Sel Agar with L.C.A.T Enriched and selective; contains antibiotics colistin (kills gramnegative coliforms), vancomycin (kills gram-positives), nystatin (kills fungi Case 3 A 24-year-old female noted vaginal itching and irritation with a discharge. Previously, she developed a yeast infection that was treated with over-the-counter medications and resolved. Thinking that this was recurrence, she again self-treated. This time, however, the symptoms did not resolve. What are the possible causes for her presentation Bacterial vaginosis Candida vaginitis Trichomonas vaginalis Allergic vaginitis Chlamydia trachomatis Neisseria gonorrhoeae What investigations would you like to order for her? Explain how those investigations would help you? PH Whiff Gram stain / test Bacterial vaginosis Candida vaginitis Trichomonas vaginatis Wet prep Culture Immunologic/ molecular test Chlamydia: is currently one of the most common and widespread bacterial STDs Spread During unprotected sex. Symptoms: Occur within 7-21 days of infection. Men: Clear thick discharge from Penis, burning during urination Women: Painful Urination, itching, burning or bleeding from vagina may have vaginal discharge, dysuria, urination, labial pain/swelling, abd. Pain • Chlamydia: is currently one of the most common and widespread bacterial STDs • Spread During unprotected sex. • Responsible for causing cervicitis, urethritis, proctitis, lymphogranuloma venereum, and pelvic inflammatory disease • Potential to transmit to newborn during delivery Conjunctivitis, pneumonia • Symptoms: Occur within 7-21 days of infection. • Men: Clear thin discharge from Penis, burning during urination • Women: Painful Urination, itching, burning or bleeding from vagina. Chlamydia - Laboratory Diagnosis Tissue culture has been the standard Non-amplified tests Enzyme Immunoassay (EIA), e.g.Chlamydiazyme Nucleic Acid Hybridization (NA Probe), e.g. Gen-Probe Pace-2 detects chlamydial ribosomal RNA able to detect gonorrhea and chlamydia from one swab DNA amplification assays polymerase chain reaction (PCR) ligase chain reaction (LCR) LCR ability to detect chlamydia in first void urine What investigations you like to order for her? Explain how those investigations would help you? PH Bacterial >4.5 Whiff Gram stain / test Wet prep +++ Clue cells Culture molecular test Not helpful DNA Probe vaginosis Candida (gardnerella vaginalis) <4.5 - vaginitis Trichomonas vaginalis Immunologic/ Yeast and Candida DNA Probe Motile EIA pseudohyphae >4.5 +- Trichomonas Trophozoi DNA Probe tes Chlamydia - Laboratory Diagnosis 2- Culture This McCoy cell 1- Chlamydia Direct monolayer micrograph reveals a number Fluorescent Antibody (DFA) of intracellular C. trachomatis inclusion bodies Elementery bodies inclusion bodies Chlamydia - Laboratory Diagnosis A sexually transmitted disease caused by a bacterium Haemophilus ducreyi) characterized by a genital ulcer (sometimes called a soft chancre) that begins as a tender pimple surrounded by a reddened area. It is more commonly seen in men than women, particularly uncircumcised males . Chancroid is spread by having unprotected sex. Some symptoms include: sores or raised bumps on the genitals which eventually if untreated, becomes filled with pus and eventually ruptures leaving a painful sore/ulcer. The bacteria may also infect the lymph glands in the groin. These glands may become enlarged, hard and painful. In Women, ulcers appear on the genitals, painful urination and painful intercourse Chancroids are contagious as long as the person as open sores. 2 to 3 Following is the Gram-stained smear of from genital ulcer of a 25 –year old male The organism MOST likely causing the ulcers is ; 1. Treponema pallidum 2. Herpes Simplex Virus 2 3. Haemophilus ducreyi 4. Gonorrhea CDC / Center for Disease Control and Prevention/ Division of STD Prevention Regional adenopathy Chancroid Diagnosis: No blood test is available to diagnose chancroid, so the diagnosis is usually made on clinical grounds after a physical exam. She presented to her family physician for management. On examination there is a bad odor along with a frothy discharge and strawberry cervix. Swab of the secretions was taken in order to perform tests. “Strawberry cervix” Source: Claire E. Stevens/Seattle STD/HIV Prevention Training Center at the University of51Washi Wet prep/ Gram stain A wet mount of the swab demonstrates "swimming" Motile Trophozoites . Base on the finding, what is the most likely diagnosis? Briefly outline the management this case? Dx; Trichomoniasis Rx; Metronidazole Husband should be treated No sex until they are cured Patient Counseling and Education STDs- Ectoparasitic Infestations Lice in Pubic Area STDs- Ectoparasitic Infestations Scabies causing eczema-like Scabies (under the skin crabs) hand condition How do you diagnose HIV infection ? Serological profile of HIV infection DIAGNOSIS 1. Serological test: - Screening assay (routine ELISA/rapid) Detection Ag or Ab Confirmatory assay (Western blot, RIBA, LIA) 2. Direct Methods: PCR NA detection (early inf ,neoate inf, monitor Rx ) Genital herpes Neonatal herpes infection 1- ELISA: serum sample is analyzed for detection the IgM Ab. 2- Direct immunofluorescence (IF): scraping of the base lesion sample is analyzed for detection the Ag. 3- Polymerase chain reaction (PCR): CSF sample in case of neonatal herpes. 4- Tissue culture: vesicle fluid sample is cultured in cell line (Vero or Hep-2 cells) and then identified by the following: - Observe the viral CPE - Direct immunofluorescence (IF) Genital warts Diagnosis • External genital warts can be easily diagnosed by medical examination. • Internal genital warts can be visualized by colposcopy. Lab diagnosis: 1- Polymerase chain reaction (PCR) is used to detect HPV DNA. 2- Pap-smear test is used to identify abnormal epithelial cells of the cervix (cervical dysplasia). 3- In-situ DNA hybridization is used for HPV genotyping. THE END