* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Nutrition
Survey
Document related concepts
Transcript
NUTRITION
NRS 129 - Introduction to
Nursing Skills
Nutritional Needs
Determining Your Patient Needs:
Assessment
History
Observation - Daily Contact
Anthropometry
Laboratory data
Nutritional Needs: Nurses’
Role
Need to inform the doctor of assmt.
findings
Investigate reasons for a decreased
intake
Offer the patient alternative methods of
intake and types of food
Factors that influence our
Patterns of Eating:
Health Status
Culture & Religion
Socioeconomic
Status
Personal Preference
Psychological
Factors
Alcohol & Drugs
Misinformation &
Food Fads
Dietary History
Done to assess actual or potential
problems
History focuses on habitual intake of
food and liquids
preferences
allergies
problems
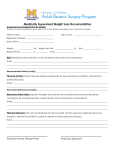
Information Obtained for a
Diet History
Name, Age
Present weight
Changes in Weight
# meals/day, snacks
Who prepares the
meal?
Problems R/T food
Chewing difficulties
Information Continued ….
Denture Use
Usual bowel pattern
Medications
Medical/Surgical
History
Physical Activity
Personal Crises
Measurements
Height and weight always done unless
patient is critically ill
Weigh patient at the same time, in
same clothing with same scale
Rapid wt. gain reflects fluid shifts
Assessment Measurements
Anthropometric:
wrist, mid-arm, skin fold measurements
Body Mass Index
Weight (kg) / Height (m2)
>25 = overweight
>30 = obese
>35 higher medical risk for CAD, DM, HTN
Characteristics of Health
Category
Good
Poor
General
Appearance
Alert,
Responsive
Listless,
apathetic,
cachexia
Laboratory Data
CBC: Low Hemoglobin and Red blood
cell count = anemia
Serum Albumin: If value is decreased
= protein & calorie malnutrition
Negative Nitrogen Balance = catabolic
state
Hgb, Hematocrit, and BUN reflect
hydration
Patients at Risk for Nutritional
Problems:
Condition that interferes with ingestion,
digestion, and absorption
Surgical revisions of the GI tract
IV intake only for > 7-10 days
Poor dietary habits
Patients undergoing treatment for CA
Management of
Common Problems
Vomiting
How do you position
your patient?
Serve small amounts
frequently
Anti-emetics:
time administration
appropriately
Planning & Implementation
Make sure your patient is comfortable
No odors in the room
Attractive tray
Not in pain or needing nursing care
Mouth Care
Positioned correctly
Special Diets
Are they Necessary?
Why?
Basic Types of Hospital Diets
General (Regular)
Soft vs. Mechanical Soft
Full Liquid
Clear Liquid
Basic Types of Hospital Diets
Low-Residue
High Fiber
Pureed Diet
Sodium Restricted
Dietary Modifications for
Disease Conditions
Gastrointestinal disease:
Diarrhea (Low residue)
Acute gastritis: Liquid, bland
Chronic gastritis: avoid foods causing the
problem
Diverticulitis:
Acute: low residue
Chronic: high fiber
Dietary Modifications. . .
Peptic Ulcer:
Eat what you can
tolerate
May need to avoid
spices, alcohol,
caffeine
Cardiovascular Disease:
Cardiac Prudent Diet
Goals:
decrease stomach distention
decrease weight
decrease lipids
Cardiovascular Disease . . .
Atherosclerosis & Hypertension:
weight,
Low fat, cholesterol, and
low sodium
Myocardial Infarction
Avoid ice, caffeine, low fat, low sodium,
cholesterol
Diabetes with Dietary Changes
Diet, exercise
Individualized Plan
Control of
cholesterol, lipids,
Increased use of
complex
carbohydrates
CHO counting
BALANCE
Dietary Modifications: Renal
Depends on disease state:
Acute versus Chronic:
May Need restriction of protein, sodium,
fluids, and potassium
Nursing Interventions:
Assisting with Eating
Assure patient’s diet/tray is correct
Good Lighting (vision) available
Remove covers
Arrange food & Prepare food
Offer assistance, self
Evaluation of intake
Assessing the Need
to Feed a Patient
Patients who should minimize oxygen
needs
Patient who cannot feed self because of
disease process or weakness
Nursing Interventions
for Feeding
Being Fed = Loss of Independence
Need to be considerate of Patient to
protect their dignity
Allow patient to set pace NOT you
Describe meal so patient can determine
the sequence
Nursing Interventions for
Feeding
Before Starting: Evaluate comfort needs
pain relief (timed appropriately) 30’
Offer bedpan
Position patient as upright as possible
Good Opportunity for Nursing
Assessment
M/S, agility, color, tremors, etc.
Nursing Interventions for
Feeding
Protect the patient’s clothing
“Napkin” No Reference to “Bib”
Assume a comfortable position at the
patient’s level
May need a signal for indicating
additional food
Offer self: “ Talk to patient”
Nursing Interventions . . .
Additional Guidelines:
Stroke patient: Don’t place food on
paralyzed side
Relatives may assist with feeding: Be
careful, family may view as they would
only eat if they are there
Don’t scold patients who cannot eat
Assure the environment is clean afterwards
Nursing Interventions . . .
Encourage Food intake
get rid of odors
Make positive comments about food
Breakfast usually best time of day
nausea:
slow deep breaths
avoid movement
limit food and fluid intake
Intake and Output
Why is it important?
What is included in the measurement?
All things liquid at room temperature
Thin, cooked cereals
Tube feedings, irrigations, IV fluids
Measurement of I and O
Incorporate the pt. in the process
Need to record amounts immediately
after consumption or elimination
Need to total amounts at specified
times
End of 8 hour shift
End of 24 hours
Fluids to be counted as
Output:
Sum of all liquids
eliminated from the
body
Urine
Emesis
Drainage tubes
Remaining Irrigation
fluid
Liquid stool
Diapers
Saturated dressings
Measurement Considerations
1 pint { 475 ml }
of water = 1 pound
1 ounce = 30 cc
or 30 ml
Measurement of Output
Urine is chief source of output
Teach patient & family need to measure
Hat may be placed in toilet
Catheter drainage bag
Leg Bag
Bedpan/urinal
{need to measure using graduated cylinder}