* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Med Rec 1 Orientation - Communities of Practice
Survey
Document related concepts
Transcript
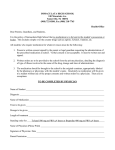
A formal process of obtaining a complete and accurate list of each patient’s current medications At Admission, Discharge and at all other Transitions in Care • Chart reviews have revealed over half of all hospital medication errors occur at the interfaces of care • Medication errors are one of the leading causes of injury to hospital patients • 2004 Canadian Adverse Events Study – Drug and fluid related events were the second most common type of procedure or event to which adverse events were related • 2004 Study in Canadian Hospital – 23% incidence of adverse events in patients discharged from an internal medicine service • 72% were medication related • 2005 Canadian Study – 151 General Medicine patients • Prescribed or receiving at least four medications • Not from an extended care facility – 53.6% - Patients 1 Unintentional Discrepancy • 38.6% - Potential to cause moderate or severe discomfort or clinical deterioration • 46.4% - Omission of regularly used medication • Canadian Council on Health Services Accreditation – Patient Safety Goals & Required Organization Practices for 2005 • “Reconcile the patients’ medications upon admission, and with the involvement of the patient” • “Reconcile medications with the patient at referral or transfer and communicate the patients’ medications to the next provider of service at referral or transfer to another setting, service, service provider, or level of care within or outside the organization” • “Desirable continuity of care delivered to a patient in the health care system across the spectrum of caregivers and their environment” • “When moving between levels of care, patients’ drug information is not always transferred to all care providers in a timely fashion… consequently, the patient may not receive the most appropriate regimen for their condition of this seamless care process” Medication Reconciliation is a key component of the Seamless Care process Easy as 1-2-3 1. Create the most complete and accurate list possible of all current medications 2. Use this list when writing medication orders 3. If using this process after admission orders have been written, reconcile and resolve any discrepancies An accurate medication history is performed prior to physician admission order writing An accurate medication history is performed after physician admission order writing This history is used to write admission orders This history is compared to admission orders and any discrepancies are reconciled PREVENTS ERRORS CATCHES ERRORS Nurse/Physician/Pharmacy performs medication history at time of admission and prior to admission orders being written Medication History & Orders Form used to document medication history Medication history documented in traditional locations in the patient’s chart Physician uses Medication History & Orders Form to indicate continuation, discontinuation or change to pre-admission medications. Any others admission orders are written on usual physician order sheet Physician uses usual physician order sheet to write admission orders Orders are processed to pharmacy using Medication History & Orders Form for any pre-admit medications and using the physician’s order sheet for new admission orders Orders are processed to pharmacy using usual physician order sheet Pharmacy dispensary receives the orders and processes as usual If a Medication History & Orders Form was completed in the admission order writing process, no further medication reconciliation is required All patient admitted without a completed Medication History & Orders Form will be assessed using the Assessment of Patient Risk (APR) Tool to determine all high risk patients requiring the completion of a Medication Reconciliation process Patients deemed high risk using the Assessment of Patient Risk (APR) Tool will be referred to the Clinical Pharmacy team The Medication History & Orders Form will be used as a worksheet to collect and document the medication history. (Additional patient may be audited if time permits) Clinical Pharmacy team will compare admission orders to medication history using the Medication History & Orders Form as a worksheet to document any discrepancies. If potential discrepancies are identified, a Discrepancy Clarification & Resolution Form will be completed and will be referred to the Clinical Pharmacist along with a copy of the Medication History Worksheet The Clinical Pharmacist will review potential discrepancies and determine urgency to clarify. If not urgent, the Discrepancy Clarification & Resolution Form will be placed on the patient’s chart for completion by the physician upon his/her next visit. If urgent, the pharmacist will contact the physician by phone to clarify and will write verbal orders onto the Discrepancy Clarification & Resolution Form and will place in the patient’s chart to be processed as an order. The Clinical Pharmacy team will review patient charts daily and will follow until all discrepancies are resolved. Once physician clarifies discrepancies, Clinical Pharmacy team will classify the outstanding discrepancies on the Medication History Worksheet and will file. All statistics will be compiled and reported in a monthly report. • To reconcile patients within 24 hours of admission • At a minimum, target “high-risk” patients identified using the Assessment of Patient Risk (APR) Tool Reconcile patients who have scored 10 or have been admitted as a result of a drug-related problem • If time permits, set a goal to reconcile as many patients as possible, if not ALL Assessment of Patient Risk (circle all applicable factors) 0 – 64 years 0 65 – 80 years 1 > 80 years 2 0-1 0 2-4 2 5-7 3 8 or more 6 Antiseizure 3 Anticoagulant 3 More than two cardiovascular medications 5 Diabetic medications (oral +/- insulin) 2 Age Number of Medications Prior to Admission High Risk Medications Prior to Admission Is the reason for admission clearly drug-related (e.g. drug toxicity, non-compliance, polypharmacy)? Total Score Yes No 9 • Antiseizure • carbamazepine, phenytoin, valproic acid & divalproex sodium. • Anticoagulants • warfarin, low molecular weight heparin (e.g. enoxaparin, nadroparin), heparin. • NOT ASA. • Diabetic medications • Chlorpropamide, gliclazide, glyburide, metformin, rosiglitazone • Cardiovascular Medications • blood pressure meds, cholesterol meds, digoxin, amiodarone, daily ASA, clopidogrel, diuretics. • Do not count anticoagulants as a cardiovascular medication. Assessment of Patient Risk (circle all applicable factors) 0 – 64 years 0 65 – 80 years 1 > 80 years 2 0-1 0 2-4 2 5-7 3 8 or more 6 Antiseizure 3 Anticoagulant 3 More than two cardiovascular medications 5 Diabetic medications (oral +/- insulin) 2 Age Number of Medications Prior to Admission High Risk Medications Prior to Admission Is the reason for admission clearly drug-related (e.g. drug toxicity, non-compliance, polypharmacy)? Total Score Yes No 0 Assessment of Patient Risk (circle all applicable factors) 0 – 64 years 0 65 – 80 years 1 > 80 years 2 0-1 0 2-4 2 5-7 3 8 or more 6 Antiseizure 3 Anticoagulant 3 More than two cardiovascular medications 5 Diabetic medications (oral +/- insulin) 2 Age Number of Medications Prior to Admission High Risk Medications Prior to Admission Is the reason for admission clearly drug-related (e.g. drug toxicity, non-compliance, polypharmacy)? Total Score Yes No 10 Referral to Clinical Pharmacy Team Recommended/Required? Yes No Unsure Reason for referral: Example #1: Patient experiencing digoxin toxicity Form completed by: Alana Froese Date: Today’s Date Example #2: Scored 12 If total score is 10, if referral to a pharmacist is recommended or if the reason for admission is drug-related - place form in troubleshooting file Case Study: Carol Harrison • Admitted to Emergency Department at 0800hr with palpitations, tremor and flushing • Apparently patient thought her theophylline was acetaminophen extra strength and took two tablets at approximately 0400hr • Review her Pharmanet record and determine if she is considered “high risk” and a candidate for Medication Reconciliation MEDICATION RECONCILIATION Patient Name: Carol Harrison ASSESSMENT of PATIENT RISK (APR) TOOL Assessment of Patient Risk (circle all applicable factors) 0 – 64 years Age 65 – 80 years > 80 years 0-1 Number of Medications 2-4 Prior to Admission 5-7 8 or more Antiseizure Anticoagulant High Risk Medications More than two cardiovascular Prior to Admission medications Diabetic medications (oral +/insulin) Is the reason for admission clearly drug-related (e.g. drug toxicity, non-compliance, polypharmacy)? 0 1 2 0 2 3 6 3 3 5 Examples of medications for each medication category: Antiseizure e.g. carbamazepine, phenytoin, valproic acid & divalproex sodium. Anticoagulants e.g. warfarin, low molecular weight heparin (e.g. enoxaparin, nadroparin), heparin. NOT ASA. Cardiovascular Medications e.g. blood pressure meds, Yes cholesterol meds, digoxin, No amiodarone, daily ASA, clopidogrel, diuretics. Total Score Do not count anticoagulants as a cardiovascular medication. Referral to Pharmacist Recommended/Required? Yes No Unsure 2 Reason for referral: Admitted for drug-related problem – excess use of theophylline Form completed by: Date: Alana Froese Today’s Date If total score is 10, if referral to a pharmacist is recommended or if the reason for admission is drug-related place form in troubleshooting file Definition A medication history obtained by a healthcare professional which includes a thorough history of all regular medication use (prescription and non-prescription) • • • • • • • • Patient – best source if patient competent Caregiver Pharmanet Prescription vials/Compliance packaging Medication List Pharmacy Family Physician MAR from previous institution • Print Pharmanet record • Addressograph Forms • Determine if patient is capable of providing med history • Pharmanet is simply a record of the DISPENSING HISTORY – Does not indicate the medications discontinued or active or if the patient is taking the medications as prescribed – Does not include HIV/AIDS medications – Does not include samples given to patients in doctor offices – Does not include physician office changes (without writing a prescription) – Does not include medications given in hospitals • Medinet is a provider of Pharmanet info For Demo Purposes Pharmanet medication information for past 15 months 9029 820 762 HARRISON, CAROL A – 1927 Feb 01 – F Demographics Reported Clinical Conditions – 1 found: PHN – Personal Health Number (Care Card #) HYPERCHOLESTEREMIA 1999 Mar 01 Patient Name Reported Adverse Reactions – 2 found: 510645 2000 Jul 18 SULFAMETHOXAZOLE/TRIMETHOPRIM NOVOPHARM LTD 800-160MG TABLET P1/02301 RASH 2043246 1996 Jan 01 PENICILLIN G POTASSIUM WYETH-AYERST CA 10MU VIAL 91/15399 ANAPHYLAXIS Reported Medication History – 15 of 15 printed: 510645 14 @ 2/day Reversed: SULFAMETHOXAZOLE/TRIMETHOPRIM NOVOPHARM LTD 800-160MG TABLET TAKE ONE TABLET TWICE DAILY 2006 May 30 91/07692 (HARDY) Prescription cancelled by physician 2169126 250 @ 8.333/day Filled: P-EPHED HCL/CODEINE/TRIPROL RATIOPHARM 30-10-2/5 LIQUID TAKE 5 TO 10 ML EVERY 6 HOURS AS NEEDED 2006 Mar 29 91/03361 (LAVOY) 28053 15 @ 2.143/day Filled: SULFACETAMIDE SODIUM SCHERING CANADA 10% DROPS 2 DROPS IN EACH EYE EVERY 3 HOURS FOR 7 DAYS 2006 Mar 24 91/03361 (LAVOY) 2213672 120 @ 4/day FLUTICASONE PROPIONATE GLAXO SMITH KLINE 50MCG SPRAY USE TWO SPRAYS IN EACH NOSTRIL DAILY Date of Birth Sex For Demo Purposes Pharmanet medication information for past 15 months 9029 820 762 HARRISON, CAROL A – 1927 Feb 01 – F Reported Clinical Conditions – 1 found: HYPERCHOLESTEREMIA 1999 Mar 01 Patient Reported Adverse Reactions – 2 found: 510645 2000 Jul 18 SULFAMETHOXAZOLE/TRIMETHOPRIM NOVOPHARM LTD 800-160MG TABLET P1/02301 RASH 2043246 1996 Jan 01 PENICILLIN G POTASSIUM WYETH-AYERST CA 10MU VIAL 91/15399 ANAPHYLAXIS Reported Medication History – 15 of 15 printed: 510645 14 @ 2/day Reversed: SULFAMETHOXAZOLE/TRIMETHOPRIM NOVOPHARM LTD 800-160MG TABLET TAKE ONE TABLET TWICE DAILY 2006 May 30 91/07692 (HARDY) Prescription cancelled by physician 2169126 250 @ 8.333/day Filled: P-EPHED HCL/CODEINE/TRIPROL RATIOPHARM 30-10-2/5 LIQUID TAKE 5 TO 10 ML EVERY 6 HOURS AS NEEDED 2006 Mar 29 91/03361 (LAVOY) 28053 15 @ 2.143/day Filled: SULFACETAMIDE SODIUM SCHERING CANADA 10% DROPS 2 DROPS IN EACH EYE EVERY 3 HOURS FOR 7 DAYS 2006 Mar 24 91/03361 (LAVOY) 2213672 120 @ 4/day FLUTICASONE PROPIONATE GLAXO SMITH KLINE 50MCG SPRAY USE TWO SPRAYS IN EACH NOSTRIL DAILY Clinical conditions Typically this area is not used Reported by Date reported For Demo Purposes Pharmanet medication information for past 15 months 9029 820 762 HARRISON, CAROL A – 1927 Feb 01 – F Reported Clinical Conditions – 1 found: HYPERCHOLESTEREMIA 1999 Mar 01 Patient Reported Adverse Reactions – 2 found: 510645 2000 Jul 18 SULFAMETHOXAZOLE/TRIMETHOPRIM NOVOPHARM LTD 800-160MG TABLET P1/02301 RASH 2043246 1996 Jan 01 PENICILLIN G POTASSIUM WYETH-AYERST CA 10MU VIAL 91/15399 ANAPHYLAXIS Allergies and Reactions Can not guarantee this is an accurate listing of allergies Reported by: Date reported PRACTITIONER CODES Reported Medication History – 15 of 15 printed: 510645 14 @ 2/day Reversed: SULFAMETHOXAZOLE/TRIMETHOPRIM NOVOPHARM LTD 800-160MG TABLET TAKE ONE TABLET TWICE DAILY 2006 May 30 91/07692 (HARDY) Prescription cancelled by physician V9 Veterinarian 91 Physician/Surgeo n 2169126 250 @ 8.333/day Filled: P-EPHED HCL/CODEINE/TRIPROL RATIOPHARM 30-10-2/5 LIQUID TAKE 5 TO 10 ML EVERY 6 HOURS AS NEEDED 2006 Mar 29 91/03361 (LAVOY) 28053 15 @ 2.143/day Filled: SULFACETAMIDE SODIUM SCHERING CANADA 10% DROPS 2 DROPS IN EACH EYE EVERY 3 HOURS FOR 7 DAYS 2006 Mar 24 91/03361 (LAVOY) 2213672 120 @ 4/day FLUTICASONE PROPIONATE GLAXO SMITH KLINE 50MCG SPRAY USE TWO SPRAYS IN EACH NOSTRIL DAILY 95 Dentist P1 Pharmacist 93 Podiatrist 98 Midwife For Demo Purposes Pharmanet medication information for past 15 months 9029 820 762 HARRISON, CAROL A – 1927 Feb 01 – F Reported Clinical Conditions – 1 found: HYPERCHOLESTEREMIA 1999 Mar 01 Patient Reported Adverse Reactions – 2 found: 510645 2000 Jul 18 SULFAMETHOXAZOLE/TRIMETHOPRIM NOVOPHARM LTD 800-160MG TABLET P1/02301 RASH 2043246 1996 Jan 01 PENICILLIN G POTASSIUM WYETH-AYERST CA 10MU VIAL 91/15399 ANAPHYLAXIS Reported Medication History – 15 of 15 printed: 510645 14 @ 2/day Reversed: SULFAMETHOXAZOLE/TRIMETHOPRIM NOVOPHARM LTD 800-160MG TABLET TAKE ONE TABLET TWICE DAILY 2006 May 30 91/07692 (HARDY) Prescription cancelled by physician Dispensing History -Most recent reported first -Drug by generic name(s) -Drug Identification Number (DIN) -Quantity 2169126 250 @ 8.333/day Filled: P-EPHED HCL/CODEINE/TRIPROL RATIOPHARM 30-10-2/5 LIQUID TAKE 5 TO 10 ML EVERY 6 HOURS AS NEEDED 2006 Mar 29 91/03361 (LAVOY) -Sig (Instructions) 28053 15 @ 2.143/day Filled: SULFACETAMIDE SODIUM SCHERING CANADA 10% DROPS 2 DROPS IN EACH EYE EVERY 3 HOURS FOR 7 DAYS 2006 Mar 24 91/03361 (LAVOY) -Date Filled or Reversed 2213672 120 @ 4/day FLUTICASONE PROPIONATE GLAXO SMITH KLINE 50MCG SPRAY USE TWO SPRAYS IN EACH NOSTRIL DAILY -Physician • Review entire dispensing history • Multidoctoring? – scan for number of physicians dispensing • Non-compliance? – are chronic meds being filled at regular intervals • Consider how much of the history to print – Look for intermittently used medications that may still be considered active orders and ensure they are included when printed » Salbutamol MDI 2 puffs q4h prn » Topical creams • If you can not identify a drug by its generic name(s), searching Canada’s Drug Product Database using the Drug Identification Number (DIN) will help you identify the brand name and manufacturer – http://www.hc-sc.gc.ca/hpb/drugs-dpd/ 2169126 250 @ 8.333/day Filled: P-EPHED HCL/CODEINE/TRIPROL RATIOPHARM 30-10-2/5 LIQUID TAKE 5 TO 10 ML EVERY 6 HOURS AS NEEDED 2006 Mar 29 91/03361 (LAVOY) Ratio – Cotridin • What’s in the Drug name – List of active chemical entities • Generic name(s) – Sometimes includes secondary name • Example: Salts of Erythromycin base • Estolate, Ethylsuccinate, Lactobionate – Additional product information • Strength & Formulation – Listed between the name and strength of the product • Manufacturer 21016 60 @ 1/day Filled: QUININE SULFATE NOVOPHARM LTD 300MG CAPSULE TAKE ONE CAPSULE AT BEDTIME AS NEEDED FOR LEG CRAMPS 2005 Dec 04 91/02295 (MACKAY) • Watch for specialty formulation information 2014165 90 @ 1/day Filled: THEOPHYLLINE ANHYDROUS PURDUE PHARMA 400MG TAB SR 24H TAKE ONE TABLET ONCE DAILY 2006 Mar 04 91/02295 (MACKAY) 02202441 56 @ 2/day Filled: OXYCODONE PURDUE PHARMA 10MG TABLET CR TAKE ONE TABLET EVERY 12 HOURS 2006 May 22 91/05568 (BROWN) 2007959 90 @ 1/day Filled: ACETYLSALICYLIC ACID PHARMASCIENCE 81MG TABLET DR TAKE ONE TABLET ONCE DAILY 2006 Mar 04 91/02295 (MACKAY) 2237280 60 @ 1/day Filled: Sustained Release Controlled Release VENLAFAXINE WYETH CANADA 75MG CAPSULE XR TAKE ONE CAPSULE ONCE DAILY 2006 Apr 15 91/05568 (BROWN) Delayed Release Extended Release • Time commitment – Goal 15min • Confirm positive identification of patient • Introduce yourself and explain your role – Tell patient you would like to ask him/her some questions about his/her medication use – Ask if this is a good time • If not, schedule another time • Ask questions until you are confident all information is complete and reliable – Pursue unclear answers until they are clarified • Use open-ended questions (what, how, why, when) balanced with yes/no questions WHAT medication do you take? Ramipril WHAT is the strength of the Ramipril? 10mg HOW often do you take it? Once daily WHEN do you take your Ramipril each day? Lunch time Do you ever forget to take your Ramipril? No • Use nonbiased questions – Do not lead the patient into answering something that may not be true WHAT NOT TO DO So you are taking Ramipril? Yes …and your Ramipril is a 10mg capsule? Yes …and the Pharmanet record says you take it once daily? Yes …and you take this with your other meds in the morning? Yes …and you are taking routinely without forgetting a dose? Yes • Ask simple questions – Avoid using medical jargon Are you taking any OTC meds? Are you taking any non-prescription medications? Do you take your lorazepam orally or sublingually? Do you swallow your lorazepam whole or do you place it under your tongue? • Prompt the patient to remember all medications – Prescriptions • Patches, creams, eye drops, inhalers, sample medications – Over-the-counter (OTC) medications – Herbal and other natural remedies – Vitamins and minerals • Use “head-to-toe” Review of Systems approach • HEENT – – – – – – Nose, ear or eye drops Analgesics used for headache or sinus pain Dental products Insomnia Motion sickness Smoking Cessation aids • Cardiovascular – Once Daily ASA • Respiratory tract – Antihistamines – Decongestants • GI/GU – – – – – – Antacids Antiflatulants Antidiarrheals Laxatives Hemorrhoidal preparations Vaginal antiinfectives • Musculoskeletal – ASA – Anti-inflammatory agents – Acetaminophen or combination • Dermatological – – – – Psoriatic/Seborrheic Antiinfective Analgesic topical preparation Corns/callus pads or other foot care • Hematological – Consider iron, B12, folic acid • Overall/System-wide – Vitamins – Herbal – Homeopathic or other alternative healthcare products • Indication – This is the patient’s version of the indication • Efficacy – Tell me how you know this medication is working for you? • Toxicity – Are there any problems that you are having which you think may be caused by this medication? – If patient says no, probe with a few of the most common side effects • Compliance – How often do you take this medication? – Try to verify if cost, dosing frequency, adverse effects, or personal beliefs may be an obstacle • How do you feel your medications impact your life? • Tell me how you feel about medication use, in general? – Inquire about technique and maintenance of devices used to facilitate drug delivery or monitor drug therapy • Inhalers and Spacers, BP monitors, Blood glucose monitors Case Study: Carol Harrison • Interview Carol and document the medication history on the blank Medication History sheet • Use Carol’s Pharmanet record and prescription vials to guide your questions Allergies/Intolerances (specify reactions) Penicillin – Hives Peanuts – Anaphylaxis Ibuprofen – GI upset Eggs? - Rxn Unknown • • • NKA Weight Height ______ kg lbs ______ m / cm ft / in Estimated Actual Estimated Actual True Allergy – Drug, food, additives, etc – Immunologically mediated reaction • Type I – Type IV (see Coombs & Gell Classification) Possible Allergy – Vague/incomplete history of allergic reaction – Assume worst case scenario – Include “?” Intolerance – Side effects or adverse events – Predictable response • N&V, GI upset Allergies/Intolerances (specify reactions) Penicillin – Hives Peanuts – Anaphylaxis Ibuprofen – GI upset Eggs? - Rxn Unknown NKA Weight __ 76.8___ kg Height lbs Estimated Actual ______ m / cm ft / in Estimated Actual • Medication dosing is frequently dependent on weight • Document patient’s weight in kilograms (kg) or pound (lbs) – Actual • Hospital weigh scale – Estimate • Patient report • Nursing estimation Allergies/Intolerances (specify reactions) Penicillin – Hives Peanuts – Anaphylaxis Ibuprofen – GI upset Eggs? - Rxn Unknown NKA Weight __ 76.8___ kg Height lbs Estimated Actual 5’ 6’’_ _ m / cm ft / in Estimated Actual • Some medications require the patient’s height as well • Document patient’s height in either m/cm or ft/in • Only use actual if patient’s height is measured by a healthcare professional at the time of admission Generic Name Dose Route Floor Use Frequency PRE-ADMISSION MEDICATION Amoxicillin/Clavulanate CHANGE ORDER COMMENTS Last Dose Date/Time D/C CONTINUE • MEDICATION NAME – Document generic name - chemical name of drug • If two chemical ingredients, list both – Avoid use of brand names • Exception: multi-ingredient drugs – Sofracort – framycetin/gramicidin/dexamethasone – Include full name (Erythromycin base, Erythromycin estolate) – Avoid use of abbreviations • Exception: ASA - Acetylsalicylic acid CHANGE Generic Name Dose Route Floor Use Frequency PRE-ADMISSION MEDICATION Amoxicillin/Clavulanate suspension CHANGE ORDER COMMENTS Last Dose Date/Time • FORMULATION – Acceptable to use abbreviations • Dosage forms – Susp or Liq - suspension or liquid – Tab or Cap – tablet or capsule • Special formulations – EC – enteric coated – SR – sustained release D/C CONTINUE CHANGE Generic Name PRE-ADMISSION MEDICATION Amoxicillin/Clavulanate suspension Dose Route Floor Use Frequency 500mg/ 125mg(5ml) CHANGE ORDER COMMENTS • Last Dose Date/Time DOSE – Weight • mg = milligram, g = gram, mcg = microgram – Do not use µg – confused with mg – Volume • ml = millilitres, L = litres – Miscellaneous • units – Do not use U or u – confused as zero • International Units – Do not use IU – confused with IV or 10 (ten) D/C CONTINUE CHANGE Generic Name PRE-ADMISSION MEDICATION Amoxicillin/Clavulanate suspension Dose 500mg/ 125mg(5ml) Route Floor Use Frequency PO CHANGE ORDER COMMENTS Last Dose Date/Time • Route – – – – – po – oral ng – nasogastric sc – subcutaneous im – intramuscular iv – intravenous D/C CONTINUE CHANGE Generic Name PRE-ADMISSION MEDICATION Amoxicillin/Clavulanate suspension Dose 500mg/ 125mg(5ml) Route PO Floor Use Frequency TID CHANGE ORDER COMMENTS Last Dose Date/Time • FREQUENCY – daily • Do not use q.d. or QD – q2days • Do not use q.o.d. or QOD – BID, TID, QID – q4h, q6h, q8h – 5 times daily D/C CONTINUE CHANGE Generic Name PRE-ADMISSION MEDICATION Amoxicillin/Clavulanate suspension Dose 500mg/ 125mg(5ml) Route PO Floor Use Frequency TID CHANGE ORDER COMMENTS 2 days of 7 days completed Last Dose Date/Time D/C CONTINUE CHANGE • Duration – If patient has been on medication < 3 months, use comment section to document this information • wks, mths, days, doses… – If medication ordered for specific duration • Indicate time taken in relation to prescribed duration in comment section – 2 doses of 14 days Generic Name PRE-ADMISSION MEDICATION Amoxicillin/Clavulanate suspension Dose 500mg/ 125mg(5ml) Route PO Floor Use Frequency TID CHANGE ORDER COMMENTS Last Dose Date/Time D/C CONTINUE CHANGE Acute Sinusitis Non-compliance: taking bid 2 days of 7 days completed • Comments – Indication as reported by patient if known – Adverse events experienced? – Physician directed patient to reduce dose at last office visit – Non-compliance Generic Name Dose Route Floor Use Frequency PRE-ADMISSION MEDICATION Ranitidine 75mg tablets (Zantac) 150mg PO DAILY PRN CHANGE ORDER COMMENTS used occasionally to treat heartburn 6 episodes/mth Last Dose Date/Time Not taken in past week D/C CONTINUE CHANGE • Last dose (date/time) – Documentation not necessary if patient is already receiving treatment in hospital – Helpful in cases where patient uses a medication prn and has not used the medication in the past week – Use 24hr hospital time – Month and day is adequate Generic Name Dose Route Floor Use Frequency PRE-ADMISSION MEDICATION Ibuprofen 400mg PO TID PRN CHANGE ORDER COMMENTS Headaches 1-2 episodes/month Last Dose Date/Time 1200hr Sep 12 D/C CONTINUE CHANGE SPECIAL SITUATIONS • Documenting PRN’s – Record frequency if there is a pattern – Include indication and frequency of episodes – Record in “Last Dose” column if medication not taken in past week Generic Name Dose Route Floor Use Frequency PRE-ADMISSION MEDICATION Etidronate 400mg/Calcium 1250mg Kit 1 tab PO Daily CHANGE ORDER COMMENTS Osteoporosis 56 tablets left in 90 day kit Last Dose Date/Time 0800hr Sep 12 D/C CONTINUE CHANGE SPECIAL SITUATIONS • Medications given in cycles – Didrocal kit – note where patient is in 90 day cycle Generic Name PRE-ADMISSION MEDICATION Cyanocobalamin Dose 1,000 mcg (1ml) Route IM Floor Use Frequency Monthly CHANGE ORDER COMMENTS Anemia Next dose due: Oct 21 Last Dose Date/Time 0800hr Sep 21 D/C CONTINUE CHANGE • SPECIAL SITUATION – Medications given at intervals • Note due date of next dose as well as last dose Source of Information Verification Codes Interviewed Patient Poor Historian Pharmanet Prescription containers Caregiver _ Jane Smith_ Ph: 987-4321 Medication List Wal-Mart _ MAR Pharmacy _ Ph: 987-6543 1 Indication 5 Wrong Drug 2 No Indication 6 Non-Compliance 3 Dose Too Low 7 Adverse Event 4 Dose Too High 8 Drug Interaction Other________________ History Documented by Date/Time • Indicate Source of Information – Ideal to interview patient • Limitations if patient: – Confused – Does not speak English – Too ill to interview – A good idea to document Pharmacy and Caregiver contact info in the event more information is needed later Source of Information Verification Codes Interviewed Patient Poor Historian Pharmanet Prescription containers Caregiver _ Jane Smith_ Ph: 987-4321 Medication List Wal-Mart _ MAR Pharmacy _ Ph: 987-6543 Other________________ History Documented by Alana Froese Date/Time Today’s Date • Sign your name • Record date and time 1 Indication 5 Wrong Drug 2 No Indication 6 Non-Compliance 3 Dose Too Low 7 Adverse Event 4 Dose Too High 8 Drug Interaction Case Study: Evelyn Smith • Use the new Medication History worksheet to interview Evelyn Smith • Evelyn was admitted to Emergency with mild confusion and dehydration • She has not brought in her prescription vials however, you have printed her Pharmanet record in preparation for the interview • Access the patient’s chart to compare admission orders to the medication history documented • Look in history or progress note sections of patient chart for reason for any changes • You are going to be shown how you can use this information to identify and document discrepancies • Type 0 - No Discrepancy • Type 1 - Intentional • Physician has made an intentional choice to add, change, discontinue a medication • Choice is clearly documented • Type 2 - Undocumented Intentional • Physician has made an intentional choice to add, change, discontinue a medication • Choice is not clearly documented • Type 3 - Unintentional • Physician unintentionally changed, added, or omitted a medication the patient was taking prior to admission • Purpose – A quick method used to indicate physician’s reason for continuing, changing or discontinuing a pre-admission medication Verification Codes 1 Indication 5 Wrong Drug 2 No Indication 6 Non-Compliance 3 Dose Too Low 7 Adverse Event 4 Dose Too High 8 Drug Interaction • INDICATION Patient has a diagnosed problem which requires a drug therapy New symptoms or indication revealed/presented Preventative drug required Taking a drug for valid indication, but this drug causes side effects which require prophylactic therapy Synergistic drug required Requires synergistic drug therapy to potentiate effect of current drug therapy • NO INDICATION No clear indication for drug use Improvement of disease state Receiving drug chronically which was intended for acute condition Recreational use, addiction/dependence Condition can be more appropriately treated by non-drug therapy Receiving a drug to treat an avoidable ADR Inappropriate duplication of therapeutic class or active ingredient • DOSE TOO LOW/DURATION TOO SHORT Drug dose too low (sub-therapeutic) Dosage regime not frequent enough Duration of treatment too short • DOSE TOO HIGH/DURATION TOO LONG Drug dose too high (dose dependent toxicity) Dosage regime too frequent Duration of treatment too long • WRONG DRUG Inappropriate drug Inappropriate drug or dosage selection More cost effective drug available Drug therapy is known to be ineffective for this indication Drug therapy is effective for this indication, but not effective in this patient for unknown reasons Inappropriate drug form Cannot take the drug product (swallow, taste, administration) Contraindication for drug (incl. pregnancy/ breastfeeding) • NON-COMPLIANCE Patient is not compliant Drug underused, overused or abused Patient has difficulties reading/understanding Drug not taken/administered at all Patient unable to use drug/form as directed Patient unwilling to carry financial costs Prescribed drug not available Wrong drug taken/administered Prescribing error Dispensing error (wrong drug or dose dispensed) Administration error (by patient/caregivers) • ADVERSE EVENT Side effect suffered at a therapeutic dose (non-allergic) Side effect suffered at a therapeutic dose (allergic) Toxic effects suffered • DRUG INTERACTION Potential or actual Drug/Drug interaction Potential or actual Drug/Food interaction Potential or actual Drug/Laboratory interaction Generic Name Dose Route Floor Use Frequency PRE-ADMISSION MEDICATION Ramipril 10mg PO BID CHANGE ORDER 0 COMMENTS Last Dose Date/Time D/C CONTINUE CHANGE 1 • If there is no change, add the verification code “1” to the continue box • Document a Type 0 discrepancy in the “Floor Use” section Generic Name Dose Route Floor Use Frequency PRE-ADMISSION MEDICATION Ramipril 10mg PO BID 5mg PO Daily CHANGE ORDER Ramipril COMMENTS Last Dose Date/Time D/C 1 CONTINUE CHANGE 4 • When there are differences, write the admission order below the medication in question • If a reason for the change has been documented by the ordering physician, use one of the verification codes to indicate the intention of the change • Document a Type 1 discrepancy in the “Floor Use” section Generic Name Dose Route Floor Use Frequency PRE-ADMISSION MEDICATION Hydrochlorothiazide 25mg PO QAM 12.5mg PO QAM CHANGE ORDER Hydrochlorothiazide COMMENTS Last Dose Date/Time D/C ? CONTINUE CHANGE ? • If a reason for the change has NOT been documented by the ordering physician, this discrepancy may either be a Type 2 or Type 3 discrepancy • Clarification with the ordering physician will be required before the type of the discrepancy can be documented • In this case, leave “undocumented” until resolved by the clinical pharmacist Generic Name Dose Route Floor Use Frequency PRE-ADMISSION MEDICATION Ramipril 10mg PO BID CHANGE ORDER Nil COMMENTS 1 Last Dose Date/Time D/C CONTINUE CHANGE 7 • When there are no matching admission orders, write “nil” below the medication in question • If a reason for the discontinuation has been documented by the ordering physician, use one of the verification codes to indicate the intention to stop • Document a Type 1 discrepancy in the “Floor Use” section Generic Name Dose Route Floor Use Frequency PRE-ADMISSION MEDICATION Ramipril 10mg PO BID CHANGE ORDER Nil COMMENTS ? Last Dose Date/Time D/C CONTINUE CHANGE ? • If a reason for the discontinuation has NOT been documented by the ordering physician, this discrepancy may either be a Type 2 or Type 3 discrepancy • Clarification with the ordering physician will be required before the type of the discrepancy can be documented • In this case, leave “undocumented” until resolved by the clinical pharmacist Case Study: Evelyn Smith • You have been to Evelyn’s chart and have reviewed the admission orders – See physician order sheet provided to you • The only place in the chart you could find explanations for changes to pre-admission medications is on the actual physician order sheet. • Begin the reconciliation process by comparing the medication history to the admission medications ordered and filling out the second part of the Medication History form • All potential type 2 or 3 discrepancies are to be documented on the Discrepancy Clarification & Resolution Form • Addressograph the form • Transcribe all information collected on potential type 2 or 3 discrepancies onto this second form • Document sources of information • Include signature and date under source of information section • Direct both forms to the Clinical Pharmacist for review and clarification/resolution • After reviewing and assessing level of urgency to resolve, the pharmacist may choose to either: • Place the form on the patient’s chart to be completed by the physician OR • Calling the physician for clarification and writing verbal orders onto the form then placing the form onto the patient’s chart for processing OR • Using the form as a worksheet only and, after clarifying, writing the verbal orders into the patient’s chart Generic Name Dose Route Frequency PRE-ADMISSION MEDICATION Hydrochlorothiazide 25mg PO QAM 12.5mg PO QAM ORDER AT ADMISSION Hydrochlorothiazide COMMENTS Hypertension Continue admission order Revert to pre-admission order • If the physician states he/she intended to change the order but did not document this on the patient’s chart, the physician/pharmacist will indicate “Continue Admission Order” Floor Use Generic Name Dose Route Frequency PRE-ADMISSION MEDICATION Ramipril 10mg PO BID ORDER AT ADMISSION Nil COMMENTS Hypertension Continue admission order Revert to pre-admission order • If the physician states he/she DID NOT intend to change the order, the physician/pharmacist will indicate “Revert to Pre-Admission Order” Floor Use Source of Information Discrepancy Types Undocumented Intentional Resolution: Continue admission order Interviewed Patient Caregiver _ Poor Historian Jane Smith_ Ph: 987-4321 Pharmacy _ Wal-Mart _ History Documented by Pharmanet Prescription containers Medication List MAR Other________________ Unintentional Resolution: Revert to preadmission order Ph: 987-6543 Nancy Green Date/Time Today’s Date Faxed to Pharmacy Authorizing Physician v/o Dr. B. Brown/Alana Froese Date/Time Today’s Date Pages ____ of ____ • Physician/Pharmacist to sign and date at bottom of form • Ideally, to be placed in patient’s chart and processed as an order Case Study: Evelyn Smith • Complete a Discrepancy Clarification & Resolution form – Ensure all potential type 2 & 3 discrepancies are filled in on the form – Refer this form as well as your original Medication History to your pharmacist for review – In this case, the pharmacist determined the physician should be called to clarify discrepancies – Call physician and document clarifications on Discrepancy Clarification & Resolution form Generic Name Dose Route Floor Use Frequency PRE-ADMISSION MEDICATION Hydrochlorothiazide 25mg PO QAM 12.5mg PO QAM CHANGE ORDER Hydrochlorothiazide COMMENTS Last Dose Date/Time D/C 2 CONTINUE CHANGE 4 • BACK TO THE MEDICATION HISTORY WORKSHEET… • A member of the Clinical Pharmacy team will indicate the reason for an undocumented intended change once clarified • Place a verification code in the change box • In this case, a Type 2 discrepancy is documented in the Floor Use box Generic Name Dose Route Floor Use Frequency PRE-ADMISSION MEDICATION Ramipril 10mg PO BID CHANGE ORDER Nil COMMENTS 3 Last Dose Date/Time D/C CONTINUE CHANGE 1 • If an Unintentional Discrepancy is identified • Indicate a Type 3 discrepancy in the Floor Use box • In this situation, the physician reverted to the preadmission order indicating a true error occurred Faxed to Pharmacy Authorizing Physician Dr. B. Brown/Alana Froese Date/Time Today’s Date Pages __1__ of __1__ • The person who completes the resolution information must indicate the physician who was involved and sign/date the bottom of the form • As this is considered a worksheet only, the Faxed to Pharmacy section is not used and this form is not processed as an order • The Pharmacy Technician will be responsible for maintaining all forms, compiling statistics and generating monthly discrepancy reports Case Study: Evelyn Smith – The final step! – Document resolutions on Medication History form – Return to Technician to compile statistics Generic Name Dose Route Frequency Floor Use PRE-ADMISSION MEDICATION Ramipril 10mg PO BID UC ORDER AT ADMISSION Nil RN COMMENTS Hypertension Continue admission order Revert to pre-admission order • Unit Clerk/Nurse will transcribe orders to MAR and initial in Floor Use section • RN will check orders and accuracy of transcription and will initial below the first initials in the Floor Use section Source of Information Discrepancy Types Undocumented Intentional Resolution: Continue admission order Interviewed Patient Caregiver _ Poor Historian Jane Smith_ Ph: 987-4321 Pharmacy _ Wal-Mart _ History Documented by Pharmanet Prescription containers Medication List MAR Other________________ Unintentional Resolution: Revert to preadmission order Ph: 987-6543 Nancy Green Date/Time Today’s Date Faxed to Pharmacy Authorizing Physician v/o Dr. B. Brown/Alana Froese Date/Time Today’s Date 1 1 Pages __ ___ of __ ___ • Unit Clerk/Nurse will indicate number of pages & check Faxed to Pharmacy Box when sending to pharmacy Case Study: Carol Harrison • You have just completed a BPMH 1. Compare the Physician Orders to the Medication History 1. 2. 3. 4. 5. Note: you are unable to glean additional information regarding the rational to therapeutic changes from other sections in the chart Document Discrepancies on Medication History form Complete Discrepancy Clarification & Resolution (DCR) form Call physician to clarify discrepancies and document on DCR form Document resolution of discrepancies on Medication History form An accurate medication history is performed prior to physician admission order writing This history is used to write admission orders PREVENTS ERRORS Nurse/Physician/Pharmacy use Medication History & Orders Form to document medication history Physician uses Medication History & Orders Form to indicate continuation, discontinuation or change to pre-admission medications. Any others admission orders are written on usual physician order sheet Orders are processed to pharmacy using Medication History & Orders Form for any preadmit medications and using the physician’s order sheet for any new admission orders “The names of the patients whose lives we save can never be known. Our contribution will be what did not happen to them. And, though they are unknown, we will know that mothers and fathers are at graduations and weddings they would have missed, and that grandchildren will know grandparents they might never have known, and holidays will be taken, and work completed, and books read, and symphonies heard, and gardens tended that, without our work, would never have been.” Donald M. Berwick, MD, MPP President and CEO Institute for Healthcare Improvement