* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Clinical-Biochemistry-of
Survey
Document related concepts
Transcript
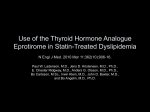
Clinical Biochemistry Aspects of Cardiovascular Disease Dr Vivion Crowley MRCPath FRCPI Consultant Chemical Pathologist Biochemistry Department St James’s Hospital Atherosclerosis is a major cause of morbidity and mortality Clinically manifests as • Coronary Heart Disease (CHD) angina MI • Peripheral vascular disease (PVD) Intermittent claudication limb amputation • Cerebrovascular disease TIA Stroke Atherosclerotic plaque is the key pathological lesion Underlying the morbidity and mortality associated with atherosclerosis What are the risk factors for the development of atherosclerotic disease? Modifiable Smoking *Dyslipidaemia *Hypertension *Obesity/T2DM Lack of exercise Non-modifiable Age Gender Family history Ethnicity Premature menopause Other risk factors for atherosclerosis •Stress/Personality •Homocysteine •Lipoprotein (a) •Fibrinogen •Socioeconomic •Geographic •? Depressive illness JBS CVD Risk Assessment Chart - Female JBS CVD Risk Assessment Chart - Male European CVD Guideline – SCORE CVD Risk Assessment Charts How is‘obese’ defined? Body mass index (BMI)= weight/height2 (kg/m2) BMI 30 Health Hazard overweight BMI 25 Healthy weight Insufficient weight BMI 20 Classification of Obesity & Overweight Time trends in the prevalence of obesity (BMI > 30kg/m2) 25 USA Germany 20 UK 15 % 10 Netherlands 5 0 1980 1985 1990 1995 1998 Year WHO MONICA 1997 data , 1997 Central (Visceral) adiposity is associated with a greater risk of developing metabolic syndrome Criteria for clinical identification of Metabolic syndrome Component Defining value Abdominal obesity WC >88cm in females >102cm in males > 1.65mmol/L Elevated fasting Triglyceride Reduced HDL cholesterol Elevated BP Elevated fasting glucose < 1/3mmol/L in females <1.0mmol/L in males SBP ≥ 130mmHg OR SBP ≥ 85mmHg 6.0mmol/L Waist circumference is a clinically useful measure of central adiposity Hypertension Defined as BP ≥ 140/90 Associated with stroke, CHD, Cardiac Failure, renal failure Aetiology - Essential (primary HT) – polygenic disorder - Secondary HT (consider in younger hyepretensive) Prevalence - 33% White males - 38% Black males Secondary Hypertension Renal disease Renovascular disease (Renal artery stenosis) -Atheroma in older subjects -Fibromuscular dyspalsia in younger subjects Coarctation of Aorta Endocrine causes -Primary hyperaldosteronism (Conn’s syndrome) -Cushing’s Syndrome -Phaeochromocytoma Renal tubular genetic defects -Liddle’s syndrome Drugs -Streoids -OCP Dyslipidaemia is a major risk factor for atherosclerosis Dyslipidaemia refers to any perturbation in lipoprotein metabolism -Hyperlipidaemia e.g. hypercholesterolaemia -Hypolipidaemia e.g. hypoalphalipoproteinaemia (low HDL) The major lipoprotein particles Very low density lipoprotein (VLDL) VLDL remnant (IDL) Low density lipoprotein (LDL) High density lipoprotein (HDL) Outline of normal lipoprotein metabolism LDL accumulates in the atherosclerotic plaque What is the relationship of plasma lipids and CHD? The plasma lipid profile consists of •Total Cholesterol (TC) •HDL Cholesterol (HDLC) •LDL Cholesterol (LDLC) •Triglycerides (TG) •TC:HDLC Raised TC and LDLC levels are positively associated with CHD HDLC levels are inversely associated with CHD -High level implies lower risk -Low level implies higher risk (M < 1.0mmol/L, F <1.3mmol/L) Raised Triglyceride levels are independently associated with CHD LDL cholesterol is calculated using the Friedewald formula Treatment targets for Plasma lipids TC <5.0mmol/L LDLC <3.0mmol/L (primary prevention) <2.5mmol/L (secondary prevention) HDL >1.0mmol/L in males >1.3mmol/L in females Elevated Plasma Cholesterol levels are associated with increased CHD mortality Plasma Total Cholesterol levels vary with age and gender CHD-related mortality is in decline over the last 30 years WHO Classification of Dyslipidaemia is now outdated Adopted by WHO in 1970 Based on laboratory parameters - Lipoprotein analysis - Lipoprotein electrophoresis - Serum/plasma appearance Most practical classification takes account of aetiology and Plasma Lipid pattern Primary (Inherited) Secondary (Acquired) Secondary Dyslipidaemias have multiple causes Diabetes mellitus Obesity Alochol abuse Hypothyroidism* Nephrotic syndrome* Chronic Renal failure* Cholestasis* PCOS Drugs -Retinoic acid -Diuretics -Steroids -OCP -HAART -Cyclosporin * Predominant Hypercholesterolamia LFTs, U/E, TFTs, BMI, WC, Glycaemic status, medications and dietary habits need to be adequately assessed in the context of dyslipidaemia Primary Dyslipidaemia should be considered in specific circumstances Abnormal lipid profile without obvious secondary cause Premature CVD Family hx of Premature CVD Family hx of dyslipidaemia 1. 2. 3. 4. Identification of primary dyslipidaemia may have implications CHD risk Clinical management Family screening Genetic counselling Primary dyslipidaemias can be sub-classified Predominantly elevated plasma cholesterol •Polygenic hypercholesterolaemia •Monogenic hypercholesterolaemias e.g. FH, FDB Predominantly elevated plasma triglyceride •Lipoprotein lipase (LPL) deficiency •ApoC-II deficiency •Familial hypertriglyceridaemia Mixed (Combined elevated plasma Cholesterol and Trigs) •Familial combined hyperlipidaemia (FCH) •Dybetalipoproteinamia (Type III HPLA) Very rare dylipidaemias •Low LDL syndromes e.g. abeta-, hypobeta-lipoproteinaemia •Low HDL syndromes -ApoA-I mutations -Tangier disease -LCAT deficiency Miscellaneous – Lp(a), Hyperalphalipoproteinamia Monogenic Hypercholesterolaemias All known defective genes causing monogenic hyeprcholesteroloaemia are involved in the receptor mediated uptake of LDL by LDL Receptor (LDLR) Familial Hypercholesterolaemia (FH) is the most prevalent autosomal dominant inherited disorder Caused by mutation in the LDLR (Goldstein and Brown) High genetic heterogeneity (implications for genetic screening of populations) > 700 mutations Heterozygous 1 in 500 Homozygous/Compound Het 1 in 1,000,000 Biochemical Characteristics of FH Pathogenesis •Reduction in functioning LDLR decreases plasma LDL catabolism •Also some degree of LDL overproduction - ? increased IDL conversion or direct liver LDL overproduction Lipid profile •Increased plasma Total Cholesterol 8-14mmol/L •Increased plasma LDL Cholesterol 6-11mmol/L •Normal or decreased plasma HDL Cholesterol •Normal plasma triglycerides Lp(a) – may also be increased ( ? Role in increased CHD risk) Clinical Characteristics of FH Tendon Xanthomata are a pathognomic feature of FH -Usual sites are extensor tendons on hands, Achilles tendon, pretibial tuberosity -Present in 70% Heterozgotes by 4th decade of life -Present in Homozygotes by age 5 years -Homozygotes also have cutaneous planar xanthomas e.g. inter-digital spaces, buttocks, knees, hands Corneal Arcus and Xanthelasmata may also be features of FH FH is associated with markedly increased risk of CHD and premature death Heterozygotes •Mean age of onset of CHD is 43yrs (males) 53yrs (females) •Relative Risk (RR) was 8 pre-introduction of statins for Rx FH •RR in statin era is 3-4 Homozygotes •Symptomatic CHD may be evident before age 10 years •Usually present by 20 yrs •Mean age of death from CHD is 26 yrs Haemodynamically significant Aortic stenosis is a major cause of morbidity in Homozygous FH •Due to atheromatous involvement of the aortic root •Usually present by puberty •In Heterozygotes, aortic valve involvement is not characteristic How do you diagnose FH? Three established sets of diagnostic criteria 1. The Simon Broome FH Register 2. Dutch Lipid Clinic Network 3. US MEDPED Program Simon Broome Register FH Criteria Differential diagnosis of FH • Polygenic Hypercholesetrolaemia • Familial Combined Hyperlipidaemia • Other monogenic Hypercholesterolaemia Screening for FH Universal Population screening – impractical, not cost effective Screening within the clinical setting (Opportunistic screening) •Hyperchol, premature CHD, Fam Hx of CHD or dyslipidaemia Cascade screening of FH relatives •Use diagnostic criteria (limited sensitivity) •Genetic approach -52-76% of patient who meet criteria are LDLR Mutation positive Management of FH Heterozygotes: Effective lowering of LDL Chol can significantly reduce morbidity and mortality Use of high dose Statins is the first line treatment Statin may not adequately reduce LDL levels Consider combination with Ezetimibe (18% further reduction), Resin or Fibrate If lack of response consider LDL-apheresis + statin (rarely required now) In females consider contraception if commencing statins or other lipid-lowering drugs Regular non-invasive testing for silent ischemia (every 1-2 years depending on risk) e.g. stress ECGs, thallium scans Family screening is mandatory in FH Dysbetalipoproteinaemia •Type III HPLA •Remnant particle disease Pathophysiology: -Absence of ApoE R mediated removal of chylomicron and VLDL remnants -Mixed HPLA where plasma Cholesterol and Trigs are elevated to the similar levels -Mean untreated levels of P Chol and Trigs is 8-10mmol/L Clinical features: Palmar xanthomatosis, tubero-euptive xanthomata Associated with increased risk of premature CHD and PVD (approx 50%) Excellent repsonse to Fibrates (± statin) Genetics of Dysbetalipoproteinaemia There are several different genetically determined isoforms of ApoE ApoE2/E2 is present in > 90% Type III HPLA E2/E2 genotype frequency of 1 in 100 However Type III HPLA prevalence is 1 in 5000-10000 Further environmental “stresses” required to manifest this pheontype e.g. T2DM, alcohol, hypothyroidism, obesity Example of a gene-environment interaction Other Mutations in ApoE e.g. R147W -can cause an autosomal dominant form of Type III HPLA CHD – clinical aspects Spectrum of clinical presentation Angina Acute Coronary Syndrome (ACS) Unstable angina MI Symptoms of ACS -Severe crushing central chest pain -Dyspnoea -Cold sweat -Pallor -Nausea Diagnosis of Acute Coronary Syndrome (ACS) Clinical history ECG -STEMI or NSTEMI -Q waves appear later Clinical Biochemistry “Older” Cardiac Biomarkers for Diagnosis of MI Creatine Kinase (CK) • muscle enzyme • Nonspecific in that it may originate from skeletal or cardiac muscle • start to increase at 3-8h • Peak level 18-24h • Returns to normal 3-4 days Aspartate transaminase (AST) • Found in Liver and muscle (an dother tissues) • Nonsepcific • Incraese 6-10h • Paek level 24h • Return to normal 3-5 days Lactate dehydrogenase (LDH) • Nonspecific (LDH 1 isoform is more cardiospecific) • Peak at 72hrs • Return to normal 8-14 days Changes CK, AST and LDH after MI New Cardiac Biomarkers for ACS Diagnosis CK-MB •Myocardium has higher concentration of CK-MB, more specific for heart •In ACS similar kinetics to total CK •CK-MB >6%of total CK indicates myocradial origin (Fractionated) •CK-MB mass >5 Troponins •Regulatory complex in muscle consisting of 3 protein T, C, I •Increases in Troponin T or I are very specific for cardiac muscle damage •In ACS increase at 3-6 hr •Peak 18-24 hr •Can remain elevated for 7-10 days •A Troponin T or I taken at 12 hrs post onset of chest pain is very sensitive Changes in Troponin I or T and CK-MB post MI Future Markers for use in diagnosis of ACS Ischaemia modified albumin - May fulfil a role as an early sensitive marker of ACS Biochemical changes in Cardiac Failure Biochemical abnormality Hyponatraemia Hypokalaemia Renal Failure Pathophysiology Diuretics, increased AVP Diuretics, 2o hyperaldosteronism Reduced perfusion Biomarkers in Diagnosis of Cardiac Failure Natriuretic peptides •Atrial Natriuretic peptide •B-type Natriuretic peptide -Both are normally produced in atrium -Induce natriuresis (Na loss in urine) BNP - produced in ventricle in cardiac failure Measurement of BNP or its cleavage product NT-proBNP -Can facilitate the diagnosis of LVF in acute dyspnoeic patient -Also can assist in identifying patinets with early LVF for echocardiogram How can NT-proBNP be used in clinical practice?