* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Fever - Yimg
Survey
Document related concepts
Transcript
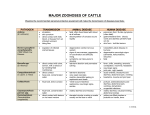
Fever • Fever may indicate the presence of a serious illness, but usually a fever is caused by common infections which are not serious Fever in Children Causes • Causes of fever include the following: – Bacterial infections – Viral infections – Medications • The causes of fever documented upon discharge were, in order of frequency, upper respiratory tract infection, nonspecific febrile illness, diarrhea, urinary tract infection, viral infection, pneumonia, herpangina, measles, pneumococcal bacteremia and dengue fever. Causes of fever in children with first febrile seizures: how common are human herpesvirus-6 and dengue virus infections? Pancharoen C - Southeast Asian J Trop Med Public Health - 01-SEP-2000; 31(3): 521-3 MEDLINE® Enteric Fever • Aka Typhoid fever is a potentially fatal multisystemic illness caused primarily by Salmonella typhi • Typhoid fever occurs worldwide, primarily in developing nations whose sanitary conditions are poor • Typhoid fever is endemic in Asia, Africa, Latin America, the Caribbean, and Oceania. Typhoid fever infects roughly 21.6 million people and kills an estimated 200,000 people every year. Shigellosis • Endemic throughout the world where it is held responsible for some 120 million cases of severe dysentery • Majority occur in developing countries • Involve children less than five years of age Etiologic Agent • Shigella species (eg, Shigella dysenteriae, Shigella flexneri, Shigella sonnei, Shigella boydii) are aerobic, nonmotile, glucosefermenting, gram-negative rods that are highly contagious, causing diarrhea after ingestion of as few as 180 organisms • The serotype 1 of S. dysenteriae (Sd1) is of particular concern due to its expression of the Shiga toxin. http://www.who.int/vaccine_research/diseases/diarrhoeal/en/index6.html Transmission • The organism is spread by fecal-oral contact; via infected food or water; during travel; or in long-term care facilities, day care centers, or nursing homes. Clinical Manifestations • • • • • • • Acute bloody diarrhea Crampy abdominal pain Tenesmus Passage of mucus Fever (1-3 d after exposure) Occasionally vomiting (35% prevalence) Physical – Lower abdominal tenderness – Normal or increased bowel sounds – Dehydration (occasional) Pathogenesis • Shigella invade the colonic epithelium by transcytosis through M cells and penetration into the epithelial cell layer by the basolateral membrane, then spread laterally from cell-to-cell. • The bacteria multiply in the cytoplasm and eventually kill the host cell while moving towards adjacent epithelial cells • The Shiga toxin inhibits protein synthesis in eukaryotic cells via inactivation of ribosomal RNA, leading to cell death. The toxin is cytotoxic, neurotoxic and enterotoxic. Treatment • Supportive care • TMP-SMX recommended if organism is suseptible. • Quinolones or Nalidixic acid if organism is resistant especially in developing countries. Acute Gastroenteritis • Inflammation of the gastrointestinal tract, involving both the stomach and the small intestine and resulting in acute diarrhea. • The inflammation is caused most often by an infection from certain viruses or less often by bacteria, their toxins, parasites, or an adverse reaction to something in the diet or medication Epidemiology • Every year worldwide rotavirus in children under 5 causes 111 million cases of gastroenteritis and nearly half a million deaths. • 82% of these deaths occur in the world's poorest nations. • In 1980 gastroenteritis from all causes caused 4.6 million deaths in children with most of these occurring in the third world. • Age, living conditions, hygiene and cultural habits are important factors. • Lack of adequate safe water and sewage treatment has contributed to the spread of infectious gastroenteritis • The incidence in the developed world is as high as 1-2.5 cases per child per year and is a major cause of hospitalization in this age group. Acute Gastroenteritis in Children • Infections of the gastrointestinal tract caused by bacterial, viral, or parasitic pathogens. • Most are food borne illnesses. • The most common manifestations are diarrhea and vomiting, which may also be associated with systemic features such as abdominal pain and fever. Food Borne Illnesses Etiology Incubation Signs and symptoms Labs Bacillus cereus 1-6 hrs Sudden onset severe nausea and vomitng Diarrhea Clinical diagnosis Stool culture Toxin Identification Clostridium botulinun 12-72 hrs Vomiting, diarrhea, blurred vision, diplopia, dysphagia, and descending muscle weakness Stool and food culture EHEC 1-8 days Severe diarrhea that is often bloody, abdominal pain and vomiting. Usually, little or no fever is present. More common in children <4 yr old. Stool culture Food Borne Illnesses Etiology Signs and symptoms Labs Abdominal cramps, fever, and diarrhea Stools may contain blood and mucus. Stool culture Salmonella spp 1-3 days Diarrhea, fever, abdominal cramps, vomiting, fever, headache, constipation, malaise, chills, and myalgia Stool culture Shigella 24-48 hrs Abdominal cramps, fever, and Stool culture diarrhea. Stools may contain blood and mucus Staph aureus 1-6 hrs Sudden onset of severe nausea and vomiting, abdominal cramps. Diarrhea and fever may be present. Clinical diagnosis Vibrio cholera 24-72 hrs. Profuse watery diarrhea and vomiting, Severe dehydration Stool culture ETEC Incubation 1-3 days Food Borne Illnesses Etiology Incubation Signs and symptoms Labs Hepatitis A 15-50 days Diarrhea, dark urine, jaundice, and flu-like Increase in ALT, symptoms, i.e., fever, headache, nausea, billirubin, and abdominal pain Positive IgM and anti–hepatitis A antibodies. Rotavirus 1-3 days Vomiting, watery diarrhea, low-grade fever. Temporary lactose intolerance may occur. Immunoassay Other (Adenovirus, Parvovirus) 1—70 hrs Nausea, vomiting, diarrhea, malaise, abdominal pain, headache, fever Serology Immunoassay Food Borne Illnesses Etiology Incubation Enatmeoba histolytioca 2-3 days to 1-4 weeks Signs and symptoms Diarrhea (often bloody), frequent bowel movements, lower abdominal pain Labs Stool examination for cysts Clinical Manifestations • • • • • • • • • • • • Abdominal Pain Nausea and vomiting Diarrhea Loss of appetite Fever Headaches Abnormal flatulence Abdominal pain Abdominal cramps Fainting and Weakness Lethargic Dehydration Management • The objective of treatment is to replace lost fluids and electrolytes. • Oral rehydration is the preferred treatment of fluid and electrolyte losses caused by diarrhea in children with mild to moderate dehydration. Management • CDC recommends that breastfed infants continue to be nursed • Formula-fed infants should continue their usual formula immediately upon rehydration with ORS in amounts sufficient to satisfy energy and nutrient requirements and at the usual concentration. • Children receiving semisolid or solid foods should continue to receive their usual diet during episodes of diarrhea. • The practice of withholding food is not recommended and immediate normal feeding is encouraged. Pharmacologic Treatment • Antibiotics are usually not useful for gastroenteritis. • Antiemetic drugs may be helpful for vomiting in children. • The World Health Organization recommends that infants and children receive a dietary supplement of zinc for up to two weeks after onset of gastroenteritis Hepatitis A • Major health problem in both developed and developing countries • The hepatitis A virus has a worldwide distribution. The highest seropositivity is observed in adults in urban Africa, Asia, and South America, where evidence of past infection is nearly universal. • Improvements in hygiene, public health policies, and sanitation have had the greatest impact on this disease, and vaccination and passive immunization have successfully led to some reduction in illness in high-risk groups. Pathogenesis • The hepatitis A virus is a single-stranded, positive-sense, linear RNA enterovirus and a member of the Picornaviridae family. • Acquisition results almost exclusively from ingestion although isolated cases of parenteral transmission have been reported. Pathogensis • Hepatocyte uptake involves a receptor, on the plasma membrane of the cell. • Viral replication is believed to occur exclusively in hepatocytes. • After entry into the cell, viral RNA is uncoated, and host ribosomes bind to form polysomes. Viral proteins are synthesized, and the viral genome is copied by a viral RNA polymerase. Assembled virus particles are shed into the biliary tree and excreted in the feces Pathogenesis • The period of greatest shedding of the hepatitis A virus is during the anicteric prodrome (14-21 d) of infection and corresponds to the time when transmission is highest. Clinical Manifestations • Prodrome – Mild flulike symptoms of anorexia, nausea and vomiting, fatigue, malaise, fever, myalgia, and mild headache. • Icteric phase – Dark urine appears first – Pale stool soon follows – Jaundice occurs in most (70-85%) adults with acute hepatitis The degree of icterus also increases with age. – Abdominal pain occurs in approximately 40% of patients. – Itch (pruritus) – Arthralgias and skin rash occurs on the lower limbs and may have a vasculitic appearance. • Relapsing hepatitis A – Relapsing hepatitis A is an uncommon sequela of acute infection, is more common in elderly persons, and is characterized by a protracted course of symptoms of the disease and a relapse of symptoms and signs following apparent resolution. Treatment • For acute cases of hepatitis A virus infection, therapy is generally supportive, with no specific treatment of acute uncomplicated illness. Amoebiasis • Infection caused by Entamoeba histolytica. • Amebiasis is the third leading parasitic cause of death worldwide. • Incidence of amebiasis is higher in developing countries. Areas of high prevalence include the Indian subcontinent, southern and western Africa, the Far East, South America, and Central America. Transmission • Food or drink contaminated with Entamoeba cysts and direct fecal-oral contact are most common means of infection Etiology • Two morphologically identical but genetically distinct species commonly affect humans. – Entamoeba dispar – Entamoeba histolytica • Infection is established by ingestion of parasite cysts Pathogenesis • The ingestion of E histolytica cysts is followed by excystation in the small bowel and invasion of the colon by the trophozoites. • Invasive disease begins with the adherence of E histolytica to colonic mucins, epithelial cells, and leukocytes. Adherence of the trophozoite is mediated by a galactose-inhibitable adherence lectin. Pathogenesis • After adherence, trophozoites invade the colonic epithelium to produce the ulcerative lesions typical of intestinal amebiasis. • Numerous hemolysins, cytotoxic to the intestinal mucosal cells, have been described in E histolytica. • An extracellular cysteine kinase causes proteolytic destruction of the tissue, producing flask-shaped ulcers. • Spread of amebiasis to the liver occurs via the portal blood. • Trophozoites ascend the portal veins to produce liver abscesses filled with acellular proteinaceous debris. Clinical Manifestations • • • • • • Asymptomatic cysts passage Colicky abdominal pain Diarrhea Tenesmus Blood stained stools with mucoid material Fever Treatment • Invasive amebiasis is treated with nitroimidazole followed by treatment with luminal amebicide. • Broad spectrum antibiotic may be indicated in fulminant colitis. • Perforation and megacolon are indications for surgery Patient Acute Gastroenteritis Clinical Manifestations Fever (T=39⁰C) Vomiting Abdominal pain Malaise Anorexia Weight loss Headache Productive cough Colds Abdominal Pain Nausea Vomiting Diarrhea Loss of appetite Fever Headaches Abnormal flatulence Fainting Weakness Lethargic Dehydration PE findings Ill- looking Well hydrated Well nourished Flushed skin Globular abdomen, soft Normoactive bowel sounds Epigastric tenderness No masses (+/-) abdominal tenderness Normal or increased bowel sounds Dehydration Laboratory Patient Shigellosis Clinical Manifestations Fever (T=39⁰C) Vomiting Abdominal pain Malaise Anorexia Weight loss Headache Productive cough Colds Fever Acute bloody diarrhea Crampy abdominal pain Tenesmus Passage of mucus Occasionally vomiting PE findings Ill- looking Well hydrated Well nourished Flushed skin Globular abdomen, soft Normoactive bowel sounds Epigastric tenderness Lower abdominal tenderness Normal or increased bowel sounds Dehydration (occasional) Laboratory Routine stool culture Patient Hepatitis A Clinical Manifestations Fever (T=39⁰C) Vomiting Abdominal pain Malaise Anorexia Weight loss Headache Productive cough Colds Mild flulike symptoms anorexia, nausea and vomiting, fatigue, malaise, Fever (usually <39.5°C), myalgia, and mild headache. Dark urine Pale stool Jaundice Abdominal Pruritus Arthralgias and skin rash PE findings Ill- looking Well hydrated Well nourished Flushed skin Globular abdomen, soft Normoactive bowel sounds Epigastric tenderness No masses Hepatomegaly is common. Jaundice or scleral icterus may occur. Fever Laboratory Patient Dengue Fever Clinical Manifestations Fever (T=39⁰C) Vomiting Abdominal pain Malaise Anorexia Weight loss Headache Productive cough Colds Fever Pharyngeal inflammation Rhinitis, and mild cough Frontal or retro-orbital pain, Myalgia and arthralgia Nausea and vomiting Lymphadenopathy, cutaneous hyperesthesia or hyperalgesia, Taste aberrations, anorexia Generalized, morbilliform, maculopapular rash PE findings Ill- looking Well hydrated Well nourished Flushed skin Globular abdomen, soft Normoactive bowel sounds Epigastric tenderness No masses Cold, clammy extremities, warm trunk, flushed face, diaphoresis, restlessness, irritability, and mid-epigastric pain Hepatomegaly Bleeding manifestations Laboratory Pancytopenia Neutropenia white blood cell counts of <2,000/mm3 Thrombocytopenia 100,000/mm3 hemoconcentration, with an increase of >20% in hematocrit, thrombocytopenia, prolonged bleeding time, and moderately decreased prothrombin level that is seldom <40% of control. Fibrinogen levels may be subnormal and fibrin split Clinical Manifestations PE findings Laboratory Patient Amoebiasis Fever (T=39⁰C) Vomiting Abdominal pain Malaise Anorexia Weight loss Headache Productive cough Colds Asymptomatic cysts pasaage Colicky abdominal pain Diarrhea Tenesmus Blood stained stools with mucoid material Fever *Constitutional symptoms are Ill- looking Well hydrated Well nourished Flushed skin Globular abdomen, soft Normoactive bowel sounds Epigastric tenderness No masses characteristically absent Patient Age group Enteric Fever 6 year old male Etiologic agent Salmonella spp. Transmission Fecal oral route Signs and Symptoms Laboratory findings Fever Cough Colds Abdominal pain Malaise Anorexia foul, greenyellow, liquid diarrhea (pea soup diarrhea Fever diffuse abdominal pain and tenderness Anorexia Malaise Weight loss AGE, HEPA A, DHF Patient Age group 6 year old male Etiologic agent Transmission Signs and Symptoms Laboratory findings Fever Cough Colds Abdominal pain Malaise Anorexia foul, greenyellow, liquid diarrhea (pea soup diarrhea Acute gastroenteritis Patient Age group 6 year old male Etiologic agent Transmission Signs and Symptoms Laboratory findings Fever Cough Colds Abdominal pain Malaise Anorexia foul, greenyellow, liquid diarrhea (pea soup diarrhea Hepatitis A Patient Age group Dengue Fever 6 year old male Etiologic agent Salmonella spp. Transmission Fecal oral route Signs and Symptoms Laboratory findings Fever Cough Colds Abdominal pain Malaise Anorexia foul, greenyellow, liquid diarrhea (pea soup diarrhea Fever diffuse abdominal pain and tenderness Anorexia Malaise Weight loss Patient Age group Malaria 6 year old male Etiologic agent Salmonella spp. Transmission Fecal oral route Signs and Symptoms Laboratory findings Fever Cough Colds Abdominal pain Malaise Anorexia foul, greenyellow, liquid diarrhea (pea soup diarrhea Fever diffuse abdominal pain and tenderness Anorexia Malaise Weight loss