* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Pharmacy Medication Update: Dementia
Survey
Document related concepts
Transcript
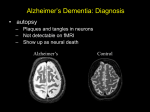
Pharmacy Medication Update: Dementia Megan J. Ehret, PharmD, MS, BCPP Associate Professor University of Connecticut Objectives • Describe the clinical presentation and diagnostic criteria for dementia and mild cognitive impairment. • Describe the treatment guidelines and landmark clinical trials for the treatment of dementia. • Select an evidenced-based drug therapy regimen for stabilizing symptoms of dementia. • Identify essential information to discuss during patient education about the drug therapy of dementia. Prevalence/Clinical Course • 2-4% of population over 65 years old • Increases with age • AD accounts for 60% of all dementias in the elderly • Gradual onset and is slowly progressive • Cognition is affected early on with impairment in motor, behavioral, and sensory functioning occurring later • Time to onset to death: 8-10 years • Loss of 3-4 points/year on MMSE Risk Factors • • • • • • • • • Degeneration of cholinergic neurons Cortical atrophy Presence of neurofibrillary tangles Accumulation of neuritic plaques Increasing age Down Syndrome Head trauma Depression Lower educational level DSM 5 Diagnostic CriteriaAlzheimer’s Disease • Must meet criteria for major or mild neurocognitive disorder • Cognitive decline from baseline in 1/5: Attention, Executive Function, Learning and Memory, Language, Perceptual-Motor, or Social Cognition) • Cognitive impairment is slow and gradual DSM 5 2013 Signs and Symptoms of AD • Loss of early memory- progresses to loss of long-term memory • Final stages: gait abnormalities, motor disturbances, decline in communication abilities, dependent on others Objective Signs of AD • Amyloid Beta Peptide• Imagining is appropriate in pts. with persistent mild cognitive impairment, pts. with core AD with atypical or unusual course, and progressive dementia with early age onset (<65) • MRI- Cortical atrophy • MMSE- 3-4 point loss • MoCA- Rapid screening instrument for mild cognitive dysfunction • Total score is 30; >26 is normal • Genetic Testing- APOE4, presenilins 1 and 2 • Controversial Alzheimer’s Association/Society of Nuclear Medicine and Molecular Imagining 2013 MINI-MENTAL STATE EXAM (MMSE) Other Rating Scales • Alzheimer’s Disease Assessment Scale (ADAS) • Evaluate the severity of dysfunction in cognition, and noncognitive behaviors over time • Severe Impairment Battery • Used to detect cognitive function in severe dementia • Neuropsychiatric Inventory • Assesses behavioral problems in dementia • Behavioral Pathology in Alzheimer’s Disease (BEHAVE-AD) • Assess behavioral symptoms and measure outcomes in treatment studies TREATMENT GUIDELINES NON-PHARMACOLOGICAL TREATMENT Therapies and Plans • • • • • Increase enjoyable activities Redirect and refocus Increase social activities for the patient Eliminate sources of conflict and frustration Assess the pt.'s caregiver for signs and symptoms of depression PHARMACOLOGICAL TREATMENT General Approach • First line treatment: Cholinesterase Inhibitors, memantine can also be used in moderate to severe dementia • Second line treatment: addition of memantine to cholinesterase inhibitors • Medications have been shown to only temporarily slow the progression of the disease • Switching between cholinesterase inhibitors is well tolerated and provides therapeutic benefit if previous agent lacked efficacy or tolerability Cholinesterase Inhibitors • Inhibit the cholinesterase (AChE) • Enzyme responsible for hydrolysis of acetylcholine • Elevates concentrations of acetylcholine for synaptic transmission in the CNS • Thought to improve memory and cognition Donepezil (Aricept)® • Treatment of mild to severe AD • Mild to moderate: 5mg daily; may increase to 10mg daily after 4-6 weeks, may increase to 23mg daily after >3 months • Moderate to severe: same as above • 23mg greater benefit in cognition, but not global functioning; higher rates of GI adverse events Donepezil • Warnings/Precautions • Peptic ulcer disease and GI bleeding: monitor for GI bleeding especially in those who are higher risk • Weight Loss • Adverse Events • Nausea, vomiting, and diarrhea: administer medication with food; reduce dose • Vagotonic effects: slows conduction through SA and AV nodes resulting in bradycardia • Insomnia: Give medication in morning Rivastigmine (Exelon)® • Treatment of mild, moderate, and severe AD, treatment of Parkinson’s Disease Dementia • 1.5mg twice daily, may increase by 3mg daily every 2 weeks based on tolerability; max dose: 6mg twice daily • Patch: 4.6mg/24hrs daily, may titrate to 9.5mg/24hrs, then to 13.3mg/24hrs (verify that old patch has been removed prior to applying a new patch) • If dosing is interrupted for more than 3 days, pt. needs to be restarted on initial dose • Same warnings/precautions Galantamine (Razadyne)® • Mild to moderate AD • IR or solution: 4mg twice daily for 4 weeks, then 8mg twice daily for >4 weeks, if tolerated than 12mg twice daily • ER: 8mg once daily for 4 weeks, then 16mg daily for >4 weeks, if tolerated than 24mg daily • Same warnings/precautions Memantine (Namenda)® • Treatment of moderate to severe AD • Low to moderate, uncompetitive, N-methyl-D-aspartate (NMDA) receptor antagonist • Glutamate is an amino acid which may contribute to the pathogenesis of AD by over-stimulating the NMDA receptor • Short acting: 5mg/day for 1 week, 5 mg twice daily for 1 week, 5 mg in the AM and 10mg in the PM for one week, then 10mg twice daily • Long acting: 7mg/day for 1 week, 14mg/day for 1 week, 21mg/day for 1 week, then 28mg/day Memantine • Use with caution in patients with seizure disorders, hepatic impairment, or mild-moderate renal impairment • Most common adverse effects: dizziness, headache, hallucinations, insomnia, confusion, and constipation Duration of Therapy • Controversial • If no efficacy seen within 3 months of therapy at maximum dose, switching should be attempted • Both immediate switching and a 7-14 day wash our has been done: good tolerability and efficacy DIETARY SUPPLEMENTS Vitamin E • Late 1990’s: recommended due to it’s antioxidant effect • Decrease the accumulation of free radicals • Evidence on prevention is mixed • Adverse effects: impaired hemostatis, fatigue, nausea, diarrhea, abdominal pains, falls • Meta-analysis: high-dose can increase mortality • Not recommended Nutraceuticals/Supplements • Ginkgo Biloba: increase blood flow, decrease blood viscosity, antagonize platelet-activating factor receptors, increase anoxia tolerance, inhibit monoamine oxidase, antioxidant • Side effects: nausea, vomiting, diarrhea, headaches, dizziness, palpitations, restlessness, weakness Nutraceuticals/Supplements • Omega-3: large, prospective, placebo-controlled trial in AD subjects • Primary study endpoints: negative Medical Food • Axona • Modification of medium-chain triglyceride formulation • Contains mixtures of C5-C12 fatty acids • Converted to betahydroxybutyrate: oxidative phosphorylation substrate by neuron mitochondria; supports brain bioenergetics • Supported by trials of 40 mg /day for 45 days Behavioral and Psychological Symptoms in Dementia Diagnostic Criteria • No specific diagnostic criteria • Could be met for impulse control disorders, obsessive-control disorder, and bipolar disorder Signs and Symptoms • Physically aggressive agitation: pushing, biting, kicking, spitting • Physically nonaggressive behavior: pacing, wondering, inappropriate voiding, undressing • Verbally aggressive behavior: screaming, yelling, cursing • Verbally nonaggressive behavior: requesting attention, repetitively calling out • Most common: apathy, delusions, aggression/agitation, anxiety, psychomotor disturbance, irritability, sleep/wake disturbance, depression, disinhibition, hallucinations Risk Factors/ Prevalence • Can occur in up to 60% of demented patients in community dwelling and 80% in long term care facilities • 1/3 of mildly-impaired dementia pts., 2/3 of moderate impairment pts. • After 5 yrs. w/dementia: 90% with have one BPSD • Risk of developing varies • Fronto-temporal dementias, LBD, vascular dementia, Huntington’s disease more likely to experience BPSD symptoms Clinical Course • Depression, apathy, social withdrawal: can be noticed several years before diagnosis of dementia • As dementia progresses: frequency and intensity of agitation and aggression worsen • At end stages of dementia, episodes of agitation and aggression may diminish Treatment Guidelines • Rule out psychological and psychosocial causes for change in behavior • Elimination of causative factors and psychosocial intervention are treatments of choice • Medication therapy can be recommended • Hyperactivity syndrome and psychosis: risperidone, olanzapine, quetiapine, aripiprazole, citalopram, trazodone, and carbamazepine • Valproic acid and lithium should be avoided: lack of evidence World Federation of Societies of Biological Psychiatry 2011 Non-Pharmacological Treatment • Treatment of choice • Recognizing, redirecting, and diffusing the neuropsychiatric behavior • Intervene early • Stay calm- avoid arguing or trying to reason with the patient • Wondering: • • • • Environmental modifications Providing activities Electronic alarms Safety Plans Non-Pharmacological Treatment • Sleep disturbances • • • • • Strive for consistent bedtimes Limit daytime napping Restrict use of alcohol and caffeinated beverages Reduce light levels, changes in temperature, and nighttime noises Avoid changes in daily routines • Other therapies: • • • • Music therapy Light therapy Massage therapy Multisensory Stimulation PHARMACOLOGICAL TREATMENT Antipsychotics • Evidence is high to support the use of antipsychotics for BPSD • Second Generation Antipsychotics • Over 37 trials; risperidone, olanzapine, quetiapine, aripiprazole • Limited to no data: clozapine, ziprasidone, paliperidone, iloperidone, asenapine, lurasidone • Range: 2 days to 1 year; endpoints were not standardized Dementia Psychosis Agitation Aripiprazole ++ + + Olanzapine + +/- ++ Quetiapine + +/- +/- Risperidone ++ ++ ++ SHIFT IN RISK PERCEPTION OF ANTIPSYCHOTICS Current Medical Realities Past Areas of Concern Weight Gain Tardive Dyskinesia Sedation Insulin Resistance CHD Prolactin Hyperlipidemia Diabetes Weight Gain Prolactin TD Hyperlipidemia Insulin Resistance Sedation Coronary Heart Disease SIDE EFFECTS OF ATYPICAL ANTIPSYCHOTICS CLOZ RIS OLZ QUE ZIP ARIP Low Blood Pressure +++ + +/0 ++ 0/+ 0/+ Dry mouth, constipation +++ 0 +/++ 0 0 0 0 +/++ 0/+ 0 +/0 0 +++ +/- ++ +++ 0 0 ++++ + ++++ ++ -/+ -/+ Lipids +++ + +++ ++ 0 0 Blood sugar +++ + +++ ++ 0 0 Tremors, stiffness, endocrine problems Sedation Weight gain CLOZ = clozapine; RIS = risperidone; OLZ = olanzapine; QUET = quetiapine; ZIP = ziprasidone; ARIP = aripiprazole; Adapted from: Nasrallah HA, Mulvihill T. Ann Clin Psychiatry. 2001(Dec);13(4):215-227 WEIGHT GAIN ATYPICAL ANTIPSYCHOTICS Data for Package Labels LIPID ABNORMALITIES Aripiprazole, Ziprasidone, Paliperidone Risperidone Quetiapine Olanzpine, Clozapine Data from product labels ADA/APA CONSENSUS CONFERENCE ON ANTIPSYCHOTIC DRUGS AND OBESITY AND DIABETES SUMMARY Drug Weight Gain Risk for Diabetes Worsening Lipid Profile Clozapine (Clozaril) +++ ++ ++ Olanzapine (Zyprexa) +++ ++ ++ Risperidone (Risperdal) Paliperidone (Invega) ++ +/- +/- Quetiapine (Seroquel) ++ +/- + Aripiprazole* (Abilify) +/- - - Ziprasidone* (Geodon) +/- - - + = increase effect; - = no effect; D = discrepant results. *Newer drugs with limited long-term data. ADA/APA CONSENSUS CONFERENCE ON ANTIPSYCHOTIC DRUGS AND OBESITY AND DIABETES SUMMARY Baseline 4 wk 8 wk 12 wk Quarterly Annually Q5yr Weight X X X X X BP X X X Fasting Glucose X X X X Waist X Circumf erence Fasting Lipid X X X X Antipsychotics • Typical Antipsychotics • 5 clinical trials comparing the efficacy of haloperidol to a SGA • Average haloperidol dose per day: 2-4 mg • No difference in efficacy with haloperidol versus a SGA Adverse Events- Black Box Warning WARNINGS: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS and SUICIDALITY AND ANTIDEPRESSANT DRUGS Black Box Warning: Cerebrovascular Accidents • Cerebrovascular Adverse Events, Including Stroke, in Elderly Patients with Dementia-Related Psychosis • In placebo-controlled trials with risperidone, aripiprazole and olanzapine in elderly subjects with dementia, there was a higher incidence of cerebrovascular adverse events (cerebrovascular accidents and transient ischemic attacks) including fatalities compared to placebo-treated subjects Risk Factors for Stroke • Beyond Control • Advancing age, risk doubles after age 55 years • Male gender • African-American • Family history of diabetes • Family history of stroke or • TIA • May be altered • • Medical • • • • • Hypertension Atrial fibrillation Elevated cholesterol Coronary Heart Disease Sleep Apnea • • Lifestyle • Smoking • Obesity • Excessive Alcohol Source: National Stroke Association Antidepressants • Mixed studies • • • • • Trazodone > haloperidol Fluoxetine = haloperidol Sertraline > placebo; agitation Citalopram- mixed studies Fluvoxamine + perphenazine > perphenazine alone • All studies showed similar adverse event profiles; studies were relatively short in duration, lacked randomization, and small number of pts. Mood Stabilizers • One meta-analysis and 5 RTCs: did not support efficacy of valproic acid in treating aggression, agitation, or psychosis • Carbamazepine: one meta-analysis and 3 trials: efficacy in treatment of agitation and aggression compared to placebo; placebo was better tolerated • Oxcarbazepine: failed trial • Lamotrigine, gabapentin, topiramate: case reports or case series Cholinesterase Inhibitors • AChE inhibitors can improve BPSD • If AChE inhibitors are tapered: Worsening of BPSD symptoms can occur Memantine • Naturalistic, small, open-labeled studies • Modest improvement in BPSD and overall good tolerability General Recommendations • Do not discontinue or change the dose of treatment without discussion with health care provider • Reduce/eliminate risk for strokes and diabetes • What matters most: • • • • • • Symptom relief Reduced care giver burden Increase quality of life Avoidance of unacceptable risks Improved functional status Risk reduction and cost of care CONCLUSION Key Concepts • Etiology is unknown • Current pharmacotherapy neither cures or arrests the pathology • Pharmacotherapy focuses on 3 areas: • Cognition • Behavioral and psychiatric symptoms • Functional ability • Pharmacotherapy may reduce the total cost of treating AD by delaying cognitive decline and time to nursing home placement