* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Ventilator Associated Pneumonia and SDD
Autoimmune encephalitis wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Multiple sclerosis signs and symptoms wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Management of multiple sclerosis wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
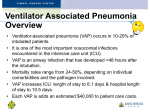
Ventilator Associated Pneumonia Dr. Hany V. Zaki Lecturer of Anaesthesia and ICU Department Ain Shams University Introduction Most patients who receive mechanical Ventilatory support for a protracted period develop microbial colonisation of the airway A subset of these patients develops invasive infection requiring antibiotics VAP is the commonest ICU acquired infection Definition Pulmonary infection acquired in hospital, at least 48 hours after intubation and ventilation. Traditional clinical features (pyrexia, leucocytosis, pulmonary infiltrates on CXR, positive endobronchial sputum culture) may be inadequate. Incidence and Risk Factors Incidence: In 2002, an estimated 250,000 healthcare-associated pneumonias developed in U.S. hospitals and 36,000 of these were associated with deaths. For the year 2010, NHSN facilities reported more than 3,525 VAPs and the incidence for various types of hospital units ranged from 0.0-5.8 per 1,000 ventilator days (Dudeck MA, Horan TC, et. al. National Healthcare Safety Network (NHSN) Report, Data Summary for 2010) Mortality Mortality ranges from 20 to 41%, depending on infecting organism, antecedent antimicrobial therapy, and underlying disease(s) COST OF VAP Strikingly, VAP adds an estimated cost of $40,000 to a typical hospital admission Risk Factors: Duration of ventilation. 3% per day in first week, 2% per day in second, 1% per day after Severity of illness: high APACHE II scores (>16) correlate with risk of VAP Head injury or other cause of coma Burns and trauma Acute of chronic respiratory condition, ARDS Male sex and increasing age Early vs Late Early onset pneumonia occurs during the first four days of hospitalization and is often caused by Moraxella catarrhalis, H. influenzae, and S. pneumoniae. Late onset pneumonia are frequently gram negative bacilli or S. aureus, including methicillin-resistant S. aureus. Viruses (e.g., Influenza A and B or Respiratory Syncytial Virus), yeasts, fungi, legionellae, and Pneumocystis carinii. VAP Etiology Most are bacterial pathogens, with Gram negative bacilli common Pseudomonas aeruginosa Proteus Acinetobacter Staphylococcus aureus Early VAP associated with non-multi-antibioticresistant organisms Late VAP associated with antibiotic-resistant organism VAP Prevention General measures - Universal Precautions and Hygiene - Feeding Kinetic therapy - Stress ulcer and DVT prophylaxis - Team Approach Prevention of Aspiration - Head up - Cuff pressure of ETT - Avoid circuit manipulation - Drainage of secretions Preventive measures for VAP Decontamination - Oral decontamination - GI decontamination - Silver ETT Early Extubation - Early weaning protocol - Daily sedation brakes Prevention of VAP General measures Prevention of Aspiration - Universal Precautions and Hygiene - Head up - Feeding - Cuff pressure of ETT - Kinetic therapy - Avoid circuit manipulation -Stress ulcer prophylaxis - Drainage of secretions - Team Approach Preventive measures for VAP Decontamination - Oral decontamination - GI decontamination - Silver ETT Early Extubation - Early weaning protocol - Daily sedation brakes Hand washing Wash hands or use an alcohol-based waterless antiseptic agent before and after suctioning, touching ventilator equipment, and/or coming into contact with respiratory secretions. CDC Guideline for Prevention of Healthcare Associated Pneumonias 2004 AACN Practice Alert for VAP, 2007 Entral Feeding and VAP Enteral feeding may predispose to aspiration of gastric contents and the subsequent development of VAP. It has been suggested that placement of a post-pyloric feeding tube might reduce the risk of aspiration and VAP. A meta-analysis of seven studies found that post-pyloric feeding showed a trend toward lower incidence of VAP and mortality than gastric feeding. however, the differences were not statistically significant The timing of initiation of enteral feeding has also been reported to be associated with the development of VAP. In a large retrospective multicenter analysis, early feeding (i.e., within 48 hours of onset of mechanical ventilation) was found to be associated with an increased risk of VAP, although ICU and hospital mortality were decreased in the early feeding group Probiotics and VAP Probiotics are commercially available preparations of live non-pathogenic microorganisms administered to improve microbial balance resulting in health benefits for the host. Administration of probiotics has been advocated as a means of preventing a variety of infections including VAP in the ICU. The potential beneficial effect of probiotics in prevention of VAP may be in their competition with VAP-producing microorganisms in the oropharynx and stomach. In addition, it has been suggested that the benefits of probiotics might be explained by their immunomodulatory properties. Administration of probiotics was also found to be beneficial in reducing length of stay in the ICU and colonization of the respiratory tract by Pseudomonas aeruginosa. Stress ulcer and VAP The use of acid-suppressive medications and the subsequent increase in gastric pH allows bacterial growth in the stomach, increasing the risk of colonization in case of aspiration of gastric contents. A cohort study of more than 60,000 patients showed an increased risk of hospital-acquired pneumonia when acid-suppressive medications were used However, no definitive recommendation can be provided about the use of acid-suppressive medications in relation to VAP in the ICU setting, and stress-ulcer prophylaxis is still suggested as part of the bundle treatments for VAP prevention published by the Institute for Healthcare Improvement Herzig SJ, Howell MD, Ngo LH, Marcantonio ER: Acid-suppressive medication use and the risk for hospital-acquired pneumonia. JAMA 2009, 301:2120-2128 Kinetic therapy Immobility of the intubated critically ill patient may impair mucociliary clearance Mechanical rotation of patients with 40° turns (kinetic therapy) may improve pulmonary function more than the improvement in function achieved via standard care (i.e., turning patients every 2 hours). Kinetic therapy is believed to improve movement of secretions and to avoid the accumulation of mucus in dependent lung zone Nakagawa NK, Franchini ML, Driusso P, de Oliveira LR, Saldiva PH, Lorenzi-Filho G: Mucociliary clearance is impaired in acutely ill patients. Chest 2005, 128:27722777 Team Approach The prevention of VAP is a multidisciplinary team approach that should involve all health care givers from doctors, nurses, assistants, porters, housekeeping as all should act together with the same protocol to decrease the incidence of VAP Prevention of VAP General measures Prevention of Aspiration - Universal Precautions and Hygiene - Head up - Feeding - Cuff pressure of ETT - Kinetic therapy - Avoid circuit manipulation - Stress ulcer prophylaxis - Drainage of secretions - Team Approach Preventive measures for VAP Decontamination - Oral decontamination - GI decontamination - Silver ETT Early Extubation - Early weaning protocol - Daily sedation brakes Oral Care Role of oral care, colonization of the oropharynx, and VAP unclear – dental plaque may be involved as a reservoir Limited research on impact of rigorous oral care to alter VAP rates Surveys indicate most nurses use foam swabs rather than toothbrushes in intubated patients Oral chlorhexidine washes decrease the incidence of VAP CDC Guideline for Prevention of Healthcare Associated Pneumonias 2004 Grap M. Amer J of Critical Care 2003;12:113-119. Silver ETT Coating the endotracheal tube with silver is theoretically attractive because silver has broad-spectrum antimicrobial activity in vitro, reduces bacterial adhesion to devices in A silver-coated tube has been developed with silver ions microdispersed in a proprietary polymer on both the inner and outer lumen, permitting ion migration to the tube surface to provide a sustained antimicrobial effect. The polymer may add to the antimicrobial activity of silver by blocking bacterial adhesion to the endotracheal tube However, despite numerous studies of various such interventions, there is insufficient evidence upon which to base strong recommendations, and important safety concerns remain regarding the use of some devices. Most importantly cost effectiveness data are lacking for modified ETTs designed to prevent VAP Respir Care 2010;55(8):1046 –1055. © 2010 Selective Digestive Decontamination VAP often have an endogenous source of infection. Colonisation of the digestive tract and the oropharynx correlates with development of VAP SDD = Selectively eliminating potentially pathogenic organisms (not normal anaerobic flora) in the digestive tract and oropharynx with the aim of decreasing the incidence of VAP and it’s associated mortality SDD usually involves: Topical application of non absorbable agents (such as polymyxin B, tobramycin and amphotericin B) that have activity against G negative organisms and fungi. Initial use of broad spectrum IV antibiotics for 3-4 days, such as cefotazime. Potential benefits: Decreased VAP, improved mortality, less time in ITU Potential problems: Increased resistant organisms, cost, side effects. Prevention of VAP General measures Prevention of Aspiration - Universal Precautions and Hygiene - Head up - Feeding - Cuff pressure of ETT - Kinetic Therapy - Avoid circuit manipulation - Stress ulcer and DVT prophylaxis - Drainage of secretions - Team Approach Preventive measures for VAP Decontamination - Oral decontamination - GI decontamination - Silver ETT Early Extubation - Early weaning protocol - Daily sedation brakes HOB Elevation HOB at 30-45º CDC Guideline for Prevention of Healthcare Associated Pneumonias 2004 ATS / IDSA Guidelines for VAP 2005 36 Primary Route of Bacterial Entry into Lower Respiratory Tract Micro or macro aspiration of oropharyngeal pathogens Leakage of secretions containing bacteria around the ET cuff Cuff pressure and VAP Cuff pressures of less than 20 cm H2O represent a modifiable risk factor for VAP. Usually cuff pressure is measured intermittently with the use of a manometer. The target cuff pressure level was 25-30 cm H2O Continuous Removal of Subglottic Secretions Use an ET tube with continuous suction through a dorsal lumen above the cuff to prevent drainage accumulation. CDC Guideline for Prevention of Healthcare Associated Pneumonias 2004 ATS / IDSA Guidelines for VAP 2005 Circuit manipulation and VAP Warm expired air condenses in ventilator tubing. Microbial growth occurs rapidly in the pooled condensate. Disconnection of the circuit and manipulation to drain the tubing can cause the contaminated condensate to dump directly into the lungs. Condensation traps permit drainage without opening the circuit, preventing both microbial dump and contamination from the external environment. Opening the circuit for other procedures should be avoided. Accumulation of condensate can also be reduced by heat-moisture exchanger (HME). However, care must be taken not to allow patient secretions to dry, which can cause endotrachael and tracheostomy tube blockage Early extubation The risk of developing VAP increases with prolonged intubation, and re-intubation is a known risk factor Since the ETT is believed to be involved in the pathogenesis of VAP, many clinicians avoid intubation when possible. The early use of NIV with the aim of avoiding intubation may be worth considering, particularly in fragile patients. Although a reduction in VAP incidence has not been demonstrated, the early use of CPAP reduced the need for ICU admission and ventilatory support Squadrone V, Massaia M, Bruno B: Early CPAP prevents evolution of acute lung injury in patients with hematologic malignancy. Intensive Care Med 2010, 36:16661674 Reduced administration of sedatives is associated with shorter ICU stays and fewer days of intubation. Although no data are currently available to prove that VAP occurrence is decreased by reduced sedative administration, daily suspension of sedative drugs has been suggested as a preventive measure. Blackwood B, Alderdice F, Burns KE, Cardwell CR, Lavery G, O'Halloran P: Protocolized versus non-protocolized weaning for reducing the duration of mechanical ventilation in critically ill adult patients. Cochrane Database Syst Rev 2010, 12:CD006904 Coppadoro A *, Bittner E and Berra L. Novel preventive strategies for ventilator-associated pneumonia. Critical Care 2012, 16:210 However, only a few have been demonstrated to be effective, and many others still need evaluation in large randomized clinical trials before definitive recommendations can be made. Among others, modifications to the ETT (e.g., subglottic secretion drainage systems, antimicrobial coating, alternative cuff shapes and materials), continuous maintenance of proper cuff inflating pressures, ETT secretion removal, patient positioning in the lateral horizontal position, kinetic therapy, and administration of probiotics are measures worthy of consideration and further study in the ongoing battle to reduce the rates of VAP.