* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download What do you tell her?
Survey
Document related concepts
Transcript
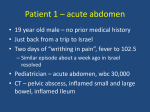
Who is in charge? Ethical dilemmas when patients and families disagree on the treatment plan Teresa Wachs, RN, CCM, BC Advances in IBD Hollywood Florida December 14, 2013 Disclosure I have no actual, potential or perceived vested interests in relation to this program. What is an ethical dilemma? An ethical dilemma is any situation in which guiding moral principles cannot determine which course of action is right or wrong. “The biggest issue in medical ethics today is the growing occurrence of conflict between health care providers, their patients and families over treatment options” -University Of Toronto Joint Centre for Bioethics Principles of Ethical Decision Making Ethical Principles • Autonomy: To acknowledge that all people have intrinsic worth, the right to hold views, to make choices and to take action based on their values and beliefs. • Beneficence: The duty to try to bring the improvements in physical or psychological health that medicine can achieve. • Non-maleficence: Going about these activities in ways that prevent further harm or reduce its risk. • Justice: The concern of fairness or impartiality. Fox,V.(1990). Caught between religion and medicine. AORN Journal, 52(1),131-146 Treatment Decisions • Preferences of patent- The choices people make when they are faced with decisions about health and medical treatments • Respect for autonomy- acknowledging the moral right of every individual to choose and follow his or her own plan of life and actions. Autonomy requires both freedom from controlling influences and the capacity for self determination. • Self Advocacy-Does patient have capacity to advocate on their behalf? Who decides? • Adult patient- able to understand treatment, risks, options and benefits. • Parents- legally authorized to consent for or refuse medical treatment. We assume that parents are best able to ascertain their child’s best interest. • Mature minor- “minors over 14 are presumed to have capacity to make medical decisions”- Cardwell v. Betchtol, 1987 New York • Emancipated minor- married, in the armed services, bearing a child, graduated from high school, living apart from one’s parents or managing their own finances. • Guardian/ Power of attorney- court appointment due to diminished mental or physical or incapacitation. Patient and Family Disagreement • Do they understand the treatment proposed? • Do they understand the risks and benefits? • Do they understand the consequences of refusing a treatment? • Are there religious or cultural reasons for refusal? • Are there financial concerns? Strategies to gain consensus • Verify understanding- ask each to repeat the plan • Ask what they think their life would be like with the proposed treatment? • Consider if finances are a barrier. • Do they expect their body to look different? • Do they think this will interfere with school or work? • Would they be willing to talk to someone who has experienced this treatment? • What do they perceive the impact on their relationships and family will be? • Are there ways to make the treatment compatible with religious or cultural beliefs.? Resources • • • • • • • • Second opinion Patient who has had a similar treatment Clergy Crohn’s and Colitis Foundation of America Power of Two Program Financial Counselor Social worker Psychologist Case Study Ellen is a 32 old female who has had Ulcerative Colitis for 20 years. Recently married. No children. She is an attorney who typically works 50-60 hours per week. She had 4 hospitalizations in the last 18 months. Treatments have included: 1. Mesalamine 2. Azathioprine 3. Infliximab for 6 years 4. 4 course of prednisone in the last 2 years Her gastroenterologist recommends a colectomy. Her husband wants her to have the surgery right away, but Ellen refuses. Possible Barriers? For Ellen: • Concern over fertility • Body image • Intimacy • Loss of income during recovery • Fear of unknown Possible Barriers? For her husband: • Concern about cancer • Difficulty seeing her sick • Fear of her dying without surgery • Caregiver fatigue • Wanting a family Cases to consider • Lori is a 15 year old female with Crohn’s that was diagnosed when she was 12, She is stable on infliximab infusions. She is now refusing to come to infusions, clinic appointments or go to school. She is defiant and disregards family rules. What do you do? What are your obligations? • Alex is a 47 year old man with UC. He was diagnosed at 22 and has stopped and started medications many times. He is undergoing a colonoscopy and states that if a malignancy is found his wife not be told. After the procedure his wife asks how things looked. What do you tell her? Cases to consider • Ben is a 16 year old male with Crohn’s Disease diagnosed 2 years ago. He was stable on azathioprine until 4 months ago when symptoms increased and colonoscopy revealed moderate to severe disease. His gastroenterologist recommends starting an Anti-TNF drug. Parents are against this therapy because of what they have read about lymphoma. They want to try the specific carbohydrate diet. Ben does not want to do the diet and wants to start on the Anti-TNF so he will be healthy for the soccer season. What do you do? What are your resources? Clinical Ethics… …is seldom a matter of deciding between ethical and unethical, between good and right verses bad and wrong; rather is involves finding the better, most reasonable solutions among the relevant options. Thank you