* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Ovaries
Survey
Document related concepts
Transcript
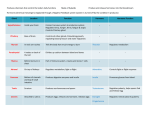
Endocrine System Chapter 16 Overview • Overall goal of endocrine system: maintain a stable internal environment (homeostasis) • Endocrine glands are “ductless glands” • Endocrine glands secrete hormones which travel through the blood to a target cell – Receptor must be present on target cell Endocrine vs Nervous System • Both systems function to maintain homeostasis • Main differences: Feature Endocrine System Nervous System Effector cells Target cells throughout the body Postsynaptic cells in muscle and glandular tissue only Chemical messenger Hormone-chemical Neurotransmitter Distance traveled by messenger Long – in blood Short – across synaptic cleft Regulatory effects Slow to appear; long-lasting Appear rapidly; short Endocrine vs Nervous System Major Endocrine Glands Classification of Hormones • Classified by Function – Tropic hormones: target other endocrine glands and stimulate their growth & secretion – Sex hormones: target reproductive tissues – Anabolic hormones: stimulate anabolism in their target cell Chemical Classifications of Hormones How Hormones Work • Hormones bind to receptors on target cells – Lock & key • Hormone-receptor interactions produce regulatory changes within the target cell – Ex: initiating protein synthesis; activation/inactivation of enzymes; opening/closing of ion channels How Hormones Work • Synergism: combinations of hormones have a greater effect on the target cell compared to a single hormone acting alone • Permissiveness: a small amount of one hormone allows a second hormone to exhibit its full effect on the target cell • Antagonism: two hormones produce opposite effects Regulation of Hormone Secretion • Hormone secretion is controlled by a negative feedback loop – Ex: parathyroid hormone (PTH) and blood calcium levels (fig 16-10) – Ex: insulin and blood glucose levels Endocrine Feedback Loop Hyper vs Hyposecretion • Tumors or abnormalities of the endocrine glands cause secretion of too much or too little hormone • Hypersecretion: production of too much hormone • Hyposecretion: production of too little hormone – Results in lack of target cell response – Also caused by target cell insensitivity Pituitary Gland • Also called hypophysis • Located on ventral surface of brain, inferior to the hypothalamus • “Master gland” because functions are crucial to life • Composed of two parts: Anterior Pituitary and Posterior Pituitary Anterior Pituitary • Hormones secreted from Anterior Pituitary: – Growth Hormone – Prolactin – Trophic hormones • Thyroid-stimulating hormone (TSH) • Adrenocorticotropic hormone (ACTH) • Gonadotropic hormones – Follicle-stimulating hormone (FSH) – Luteinizing hormone (LH) Growth Hormone • Growth Hormone (GH) – promotes growth by stimulating protein anabolism • Increased protein anabolism allows increased growth rate • Target cells: – Promotes growth of bone and muscle • GH has a hyperglycemic effect; antagonist of insulin – Hyperglycemic effect because GH stimulates fat metabolism – Interaction vital to maintaining homeostasis of blood glucose levels Growth Hormone Abnormalities • Hypersecretion – Prior to ossification of the epiphyseal plates hypersections of GH results in rapid skeletal growth Gigantism – After closure of epiphyseal plates hypersecretion causes cartilage to continue to form new bone Acromegaly • Distorted appearance; enlarged hands, feet, face, jaw; thickened skin Growth Hormone Abnormalities • Hyposecretion – Results in stunted body growth pituitary dwarfism – Treated with genetically engineered growth hormone Prolactin (PRL) • • • • Also called lactogenic hormone Initiates milk secretion (lactation) Target cells: Mammary glands During pregnancy PRL promotes development of breasts • At birth PRL stimulates milk production Prolactin Abnormalities • Hypersecretion: – Lactation in non-nursing women – Disruption of menstrual cycle – Impotence in men • Hyposecretion: – Insignificant unless mother wishes to breastfeed Trophic Hormones • Review: a trophic hormone stimulate effects of other endocrine glands • Trophic hormones released from anterior pituitary gland: – Thyroid-stimulating hormone (TSH) – Adrenocorticotropic hormone (ACTH) – Gonadotrophic hormones • Follicle-stimulating hormone (FSH) • Luteinizing hormone (LH) Thyroid-stimulating hormone (TSH) • Promotes and maintains growth and development of thyroid gland • Required for thyroid gland to secrete its hormones Adrenocorticotropic hormone (ACTH) • Promotes and maintains normal growth and development of the cortex (outer portion) of the adrenal gland • Required for adrenal cortex to secrete its hormone Gonadotrophic hormones • Target cells: gonads (testes & ovaries) • Follicle-stimulating hormone (FSH) – Females: • Stimulates growth & development of an ovum that is released each month during ovulation • Stimulate estrogen release from the ovaries – Males • Stimulates development of seminiferous tubules and maintains sperm production in the testes Gonadotrophic hormones • Luteinizing hormone (LH) – Females: • Triggers ovulation • Promotes development of corpus luteum which secretes progesterone and estrogen; these hormones help maintain pregnancy – Males: • Stimulates cells of the testes to synthesize and secrete testosterone Control of Anterior Pituitary Secretion • The hypothalamus releases chemical called releasing hormones which influence hormone secretion from the anterior pituitary gland • This regulatory mechanism is a negative feedback loop Posterior Pituitary • Hormones secreted from Posterior Pituitary: – Antidiuretic Hormone (ADH) – Oxytocin (OH) Antidiuretic Hormone (ADH) • Target cells: kidney • Prevents formation of large volumes of dilute urine • Antidiuresis • Helps conserve water balance • Example: – Blood is hypertonic change detected by osmoreceptors ADH is released water reabsorbed in kidneys and returned to blood ADH Abnormalities • Hyposecretion – – – – Diabetes insipidus Increased urine output of dilute urine “high and dry” Na+ levels are increased; ICF dehydrated • Hypersecretion – Syndrome of inappropriate antidiuretic hormone (SIADH) – Decreased urine output – Fluid overload; low Na+ levels Oxytocin (OT) • Target cells: mammary glands & uterine smooth muscle • Operates on a positive feedback loop • Stimulates uterine smooth muscle contractions – During childbirth stretching of receptors causes continued release of oxytocin until after delivery of the placenta • Ejection of milk into ducts of the breast of lactating women – When breastfeeding the suckling action of the baby causes secretion of additional oxytocin increasing milk production – Breastfeeding also helps the uterus continue to contract back to normal size during the postpartum period Pineal Body • Regulates the body’s biological clock – Patterns of eating – Sleeping – Female reproductive cycle – Behavior • Secretes melatonin – Induces sleep – Secretion is inhibited by sunlight – Target cell in humans is unknown Melatonin & Seasonal Affective Disorder • Also know as “winter depression” • During shorter days, melatonin secretion increases causes a depressed feeling in affected patients • Treatment – Exposure to high-intensity lights to inhibit melatonin secretion Thyroid Gland • The thyroid gland is composed of two lateral lobes connected by an isthmus • Located on the anterior and lateral surfaces of the trachea, below the larynx Thyroid Hormones • Tetraiodothyronine or thyroxine (T4) – Most abundant thyroid hormone – Contains 4 iodine atoms – May have effect on target cells, but mostly serve as precursor to T3 • Triodothyronine (T3) – “principal thyroid hormone” – Contains 3 iodine atoms Thyroid Hormones • Both hormone bind to plasma proteins once secreted into the bloodstream • Function: – Regulate metabolic rate of all cells – Regulate cell growth – Regulate tissue differentiation • Target cells: “general” because thyroid hormones can potentially interact with all cells of the body Hypersection • Graves Disease – Autoimmune condition (thyroid stimulating antibodies causes abnormal secretion) – Weight loss – Increases basal metabolic rate – Increased heart and respiratory rate – exophthalmos Exophthalmos Hyposecretion of Thyroid Hormone • Cretinism – develops during the growth years due to hypothyroidism – Low metabolic rate – Retarded growth and sexual development – Mental retardation (possibly) • Hypothyroidism later in life – – – – – – Decreased metabolic rate Loss of mental & physical vigor Weight gain Loss of hair Yellow discoloration of the skin myxedema Goiter • Caused by lack of iodine in the diet • Iodine is needed to synthesize thyroid hormone • Lack of iodine causes drop in thyroid hormone production/secretion • Negative feedback loop informs hypothalamus and anterior pituitary to release releasing hormones and TSH • Lack of iodine causes enlargement of thyroid gland Calcitonin • The 3rd hormone secreted from the thyroid gland • Target cells – bone • Function – regulates calcium levels in the blood by decreasing blood calcium levels – Increases action of osteoblasts (build bone) and inhibits action of osteoclasts (breakdown bone) – Antagonist to parathyroid hormone Parathyroid Glands • Parathyroid glands are embedded in the posterior aspect of the thyroid glands • Usually 4 or 5 parathyroid glands Parathyroid Hormone • Secreted from Parathyroid glands • Target cells: bone and kidney • Action: maintains calcium homeostasis – Increases osteoclast activity; decrease osteoblast activity – Calcium absorbed in kidneys and returned to the bloodstream – Activates vitamin D in the kidneys which increases intestinal absorption of calcium • Parathyroid hormone is an antagonist to calcitonin Adrenal Glands • Located on top of both of the kidneys • Composed of two parts: – Outer portion adrenal cortex – Inner portion adrenal medulla • Both parts of the adrenal glands are structurally and functionally different; often treated as two different glands Adrenal Cortex • Composed of three distinct layers or zones – Outer zone secrete mineralocorticoids – Middle zone secrete glucocorticoids – Inner zone secrete glucocorticoids and gonadocorticoids Pancreas • Located in the LUQ • Contains both endocrine and exocrine tissue • Endocrine portion is made up of tiny islands of cells called pancreatic islets (also islets of Langerhans) • Alpha cells secrete glucagon • Beta cells secrete insulin Pancreatic Hormones • Glucagon – Increases blood glucose levels • Converts glycogen to glucose in liver cells • Stimulates gluconeogenesis – Target cells liver • Insulin – Decreases blood glucose levels • Promotes movement of glucose, amino acids, fatty acids into cells • Promotes metabolism of these molecules once by cells – Target cells general (all cells) • Glucagon and Insulin produce antagonistic effects (fig 16-27, page 512) Diabetes • Results from either – 1) inadequate or absence of insulin production – 2) Insulin resistance – decreased insulin receptors results in decreased effectiveness of glucose uptake Diabetes – Signs & Symptoms • Hyperglycemia – elevated amounts of glucose in the blood – Results glucose not entering the cells properly • Glycosuria – glucose present in the urine – Elevated glucose levels in the blood exceeds kidney’s abilities to reabsorb glucose; glucose “spills over” into the urine • Polyuria – increased urine production – Water follows glucose lost in urine Diabetes – Signs & Symptoms • Polydipsia – excessive thirst – Polyuria causes dehydration • Polyphagia – excessive and continuous hunger – Although blood sugar is high cells are “starving” because cells cannot uptake glucose **3 P’s = polyuria, polydipsia, polyphagia** Type 1 Diabetes • Absolute deficiency of insulin production • Cause of beta cell destruction is unknown • Requires insulin injections or an insulin pump Type 2 Diabetes • Previously called non-insulin-dependent diabetes (NIDDM) or adult onset diabetes • Beta cell produce reduced amounts of insulin • Loss of insulin receptors on target cells leads to insulin resistance • Treated with insulin injections, oral diabetic medication and lifestyle modifications Complications of Diabetes Untreated or poorly controlled diabetes can lead to many complications that affect almost every system in the body: • Atherosclerosis – build up of fatty materials in the blood vessls – Lead to heart attack, stroke, reduced circulation • Diabetic retinopathy – can lead to blindless Complications of Diabetes • Neuropathy – nerve damage – Amputations • Kidney disease – May require dialysis Gonads – Testes & Ovaries Testes: • Composed mainly of coils of seminiferous tubules & interstitial cells • Interstitial cells secrete testosterone • Target cells – general • Function: – Growth & maintenance of male sexual characteristics – Sperm production • Testosterone secretion is regulated by the gonadotropin leutinizing hormone (LH) Gonads – Testes & Ovaries Ovaries: • Estrogen – Secreted by cells of the ovarian follicles – Target cells: general – Functions: • Promote development & maintenance of female sexual characteristics • Breast development • Regulation of menstrual cycle Gonads – Testes & Ovaries Ovaries: • Progesterone (“pregnancy-promoting hormone”) – Secreted by corpus luteum – Target cells: general – Functions (with estrogen): • Maintains the lining of the uterus to maintain a pregnancy • Remember Estrogen & Progresterone secretion is regulated by FSH and LH (gonadotropic hormones) Placenta • Tissue that forms along the lining of the uterus • Serves as the connection between the circulatory systems of the mother and developing fetus • Secretes human chorionic gonadotropin (hCG) • Target cells: ovaries Placenta • Function: – Stimulates hormone (estrogen & progesterone) secretion from the ovaries – High levels of estrogen & progesterone help maintain uterine lining for pregnancy • hCG is high during the 1st trimester • A high hCG level is used to confirm a pregnancy