* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Case Presentation
Mitochondrial optic neuropathies wikipedia , lookup
Visual impairment wikipedia , lookup
Retinitis pigmentosa wikipedia , lookup
Vision therapy wikipedia , lookup
Diabetic retinopathy wikipedia , lookup
Contact lens wikipedia , lookup
Visual impairment due to intracranial pressure wikipedia , lookup
Eyeglass prescription wikipedia , lookup
Dry eye syndrome wikipedia , lookup
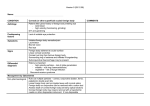
Case Presentation • Mary Palomaki November 11, 2009 9 y/o female with difficulty seeing far HPI History obtained from grandmother and patient • 9 y/o female with difficulty seeing the blackboard x 3 days. • She noticed the change in vision while playing with her dolls. • + slight pain with eye movements • + increased lacrimation • No alleviating factors, no provoking factors • Denies trauma, proptosis, edema, erythema of eye or eyelids, fever, headache, weight loss, nausea/vomiting, weakness, vertigo, neck stiffness • ROS: + cough, runny nose, sore throat x 4 days, no diarrhea or dysuria, good PO Past Medical History • • • • Birth History: FT, NSVD, no complications Tonsillectomy at age 7 History of headaches MRI (2008): cystic lesion in left hippocampus/tail of caudate nucleus, cleared by neurosurgery • FH: Mother: deceased, cancer Other History • Medications: Tylenol for sore throat • Allergies: NKDA • Immunizations: up to date (verified by CIR) • Social: lives with grandmother, three brothers, 7,9,14 y/o. Physical Exam • VS: T: 98.6 F, HR: 82, RR 16, BP: 80/60, wt: 39.9 kg, Ht 135 cm, BMI 21 (>95%tile) • Gen: Obese, NAD, AAO x 3 • HENT: NC/AT, TM: b/l shinny, grey, no fluid, + rhinorrea, oropharynx: no lesion, neck supple Physical Exam • Orbit: no edema, no discoloration, no crepitus on bony deformities, no proptosis • Eyelids: no edema, no lesion • Acuity: R: 20/20, L: 20/70, + diplopia on L • Pupils: round, symmetrical, direct and consensual pupillary reflexes intact • EOMI • No lacrimation • No nystagmus • Conjunctivae pink, no lesion, no hemorrhage Physical Exam • • • • CVS: S1/S2, no murmur, RRR Resp: CTA Abd: BS+, soft, NT/ND, no organomegaly Ext: FROM, 5/5 strength, no edema, cap refill < 2 sec. • Skin: no rash • Neuro: CN II-XII intact, normal tone, normal gait, heel-shin intact, failed pass pointing with right eye closed • GU: normal female, Tanner 1 Differential Diagnosis Ophthalmology Consult • Corneal abrasion on left eye, 4mm long • Erythromycin ointment x 3 days • Follow up with ophthalmology in 1 week Ocular Trauma Ocular Trauma Ocular trauma • 1/3 of blindness in children results from trauma • Boys age 11-15 are most at risk (M:F = 4:1) • Sports, toy darts, sticks, stones, fireworks, paintballs, air-powered BB guns are common causes of trauma Outline • • • • • • • • • • Review of Anatomy History Eye exam Corneal Abrasions Orbital fractures Lacerations Globe rupture Retinal Detachment Chemical Burns Prevention Review of anatomy History • • • • • • Mechanism of injury, events after injury Onset/duration of symptoms Preexisting eye disorders Systemic disorders Drug allergies Contraindications to anesthesia – When patient last ate • Prior tetanus immunization Physical Exam • Observation/inspection with pen light • External examination: – Orbital bones: palpate orbital rim – Position of globes (exophthalmos or enophthalmos) – Mobility of globes: note pain, diplopia, limitation of ocular rotation, and abnormal movements (nystagmus) – Inspection of lids (Do NOT palpate if globe ruptured!) • Skin, conjunctival surfaces of lids should be inspected for foreign body or laceration • Palpate lid for crepitus Physical Exam • Pupil exam: – Size – Shape – Reaction to light • Look for corneal opacities or defects • Look for blood in anterior chamber • Look for lens opacification or dislocation – Iridodonesis is a moving/shaking iris, a sign of dislocation Examination of Visual Acuity in Children • Preverbal children • Allow child to reach for a small toy with one eye covered, then the other eye covered Examination of Visual Acuity in Children • Children 4-8 years old: • Eye chart with Pictures, tumbling E’s, numbers, or letters • 2 inch wide paper taped to brow to cover one eye • Test with corrective lenses in place if possible • Vision difference more important than absolute vision • Referral to ophthalmologist if both eyes in 5 year old are 20/50 or worse, or 20/60 or worse in 6 year old Examination Visual Acuity in Children • Children > 8 years old • Use standard Snellen Chart at 20 ft. • Most common ocular condition in this age group is myopia – blurred vision at distance – can develop over several months Fluorescein Staining • First use topical anesthetic drops (proparacaine) – Warn patients and parents of transient pain before anesthesia takes effect • Moisten a fluorescein strip, and touch to lower fornix • Or use fluorescein drops • Fluorescein stains tear film, washes away on intact epithelium and stains exposed corneal stroma • Yellow dye is visible in white light, but better under ultraviolet light (Wood Lamp) – Wood’s lamp is better tolerated if photophobia present Physical Exam--Slit Lamp Exam • Binocular microscope that allows the examiner to have a three-dimensional view of the eye • Beam of light (rather than diffuse light) can be adjusted by height and width • Provides 10-25 x magnification • Anterior segment of the eye: – lids, lashes, conjunctiva, cornea, – anterior chamber, iris, and lens • Ocular foreign body removal Physical Exam: Dilation • Perform after visual acuity tested and pupil exam • Perform only if patient is neurologically intact • Use Topical 2.5% phenylephrine plus 1-2 drops of 0.5% tropicamide • Wait 20 minutes • Complete the ophthalmoscopic exam • Dilation lasts 2-5 hours • (Atropine is contraindicated because dilation can last for days.) Corneal Abrasions: Corneal Anatomy • Avascular • Densely innervated – Sensory pain fibers from CN V • 5 layers: – Epithelium: outermost, 5-6 cell-thick • Cells quickly regenerate after injury – Boman’s layer: tough layer, protects – Stroma: thick layer composed of collagen fibrils aligned in parallel – Descemet’s membrane – Endothelium: if damaged will not regenerate Corneal Abrasions • Most common eye trauma • Symptoms: photophobia, tearing, intermittent sharp pain due to ciliary body spasm, foreign body sensation • PE: irritability, blurry vision, conjunctival injection, blepharospasm, irregular red reflex, dulled corneal light reflex, fluorescein staining of epithelial defect • Be sure to evert the lid to examine tarsus • Lid Eversion Corneal Abrasions • Traumatic corneal abrasions: mechanical trauma to the eye, or foreign body under the lid • Foreign body related corneal abrasion: objects embedded in cornea • Contact lens related corneal abrasions: from over-worn, poorly fitting, dirty lens • Spontaneous defects: previous trauma Corneal Abrasions: Treatment • Remove foreign bodies with moist cotton swab or sterile needle (by ophthalmologist only) • Long-acting topical cycloplegic drop – Homatropine 5% – For pain relief caused by ciliary body spasm • Antibiotic ointment – Better than drops because it lubricates – Erythromycin – Aminoglycosides should be avoided since they can be toxic to the epithelium. – Drops with steroids are contraindicated; they slow epithelial healing and decrease immune response. • Semi-pressure patch – controlled studies have found that patching does not improve the rate of healing or comfort Corneal Abrasions: Follow Up • Small (<3 mm) abrasions with no change in vision do not need follow up – Except patients with contact lens related abrasions, where daily follow up recommended • Large abrasions (>3 mm), or any abrasion with diminished vision, need daily follow-up. Corneal Abrasion--Refer to Ophthalmologist when: • corneal infiltrate, white spot, or opacity – Refer same day • epithelial defect is larger at 24 hours, • purulent discharge present • Patient has experienced a drop in vision Orbital Fractures •Lateral Orbit fractures: zygomatic bone fracture •Cosmetic deformity, pain, difficulty opening mouth •Lateral canthus tendon inserts in the zygomatic, with fracture, the lateral canthus is inferiorly displaced •Orbital Apex fracture: •Can cause optic nerve compression, central retinal artery occlusion, retrobulbar hemorrhage •Blow-Out fracture: •Orbital floor and medial wall •Usually caused by blunt trauma with a large object Blow-Out fracture • Four signs: • Enophthalmos • Loss of sensation over malar eminence and cheek • Inability to look up on affected side • Diplopia on up-gaze • Positive traction test – Inability to rotate eye upward with forceps Blow-Out fracture: Management • Oral antibiotic prophylaxis x 5-7 days • Surgical correction 2-3 weeks later by otolaryngologist Complicated Lid Lacerations • Lid Margin lacerations: must be aligned properly to avoid lash inversion, damaging the cornea • Medial canthus lacerations: – May go through canaliculi – Cause persistant tearing – Canaliculi must be reattached Traumatic Hyphema • Blood in anterior chamber secondary to trauma • (Spontaneous Hemorrhage can occur secondary to juvenile xanthogranuloma) • Vision impaired until blood settles and forms a red meniscus • 20% of patients re-bleed – – – – “Blackball hyphema” Usually occurs at 3-5 days after initial injury Occurs from lysis of clot Recurrence of bleeding is more severe; possibly causing glaucoma, hemophthalmitis Black ball Hyphema Primary Hyphema: Management • • • • • Bed rest, elevation of the head Eye Shield Cycloplegia Topical Steroids Systemic antifibrinolytics – Aminocaproic acid: in your healthy patients • Measurement and control of intraocular pressure • Screen all black patients with hemoglobin electrophoresis – Secondary glaucoma is more likely with SS or trait Open Globe Injuries • Blunt trauma: globe rupture, most common site is near the insertion of the rectus muscles in the sclera • Penetrating trauma: laceration to the globe, most common in the cornea Open globe Injuries • Avoid any examination procedure that might apply pressure to the eyeball • For young children, an examination facilitated by procedural sedation or anesthesia should be performed by an ophthalmologist • Avoid medication (anesthetic drops or fluorescein) into the eye. • Foreign bodies should be removed by ophthalmologist Open Globe Injuries: PE • • • • • • • • Markedly decreased visual acuity Volume loss Afferent pupillary defect Increased anterior chamber depth Leakage of vitreous Outward prolapse of the uvea (iris, ciliary body, or choroid) Tenting of the cornea or sclera Low intraocular pressure – (checked by an ophthalmologist only) • Seidel sign – fluorescein streaming away from the laceration site Imaging • Axial and coronal CT of the eye without contrast – 1 to 2 mm cuts through the orbits Open Globe injuries: Management • • • • Place eye shield over the affected eye Do not touch, move eye Bed rest Antiemetic therapy (eg, IV ondansetron 0.15 mg/kg, maximum dose: 16 mg) • Pain medication: morphine, fentanyl – Don’t use NSAIDs --> platelet inhibiting properties • Sedation: lorazepam • NPO Open Globe Injury: Prognosis • Depends on: – Primary closure by ophthalmologist within 24 hours – Blunt trauma has worst outcome – Initial visual acuity – Wound location: posterior lacerations have poorest outcome – Afferent pupillary defect Open Globe Injuries: Complications • Endophthalmitis: internal eye infection • Endophthalmitis is associated with poor prognosis • Prophylactic antibiotic treatment: – Vancomycin (15 mg/kg, maximum dose: 1 gram) – ceftazidime (50 mg/kg: maximum dose 1 gram) • Organisms: – – – – – Bacillus species coagulase-negative Staphylococcus Streptococcal species S. aureus gram negative organisms Retinal detachment • Rhegmatogenous detachment: a break in the retina allows fluid to enter the subretinal space – (child abuse/shaking) • Traction retinal detachments: adhesions between the vitreous and the retina pull on the retina Retinal detachment • PE: loss of vision (curtain moving across visual field), secondary strabismus, nystagmus, leukocoria • Management: Prompt referral to ophthalmologist Chemical Injury • Immediate irrigation indicated: • Retract lids: – Double lid eversion with small vein retractor • • • • • Check pH (pH of tears is 7.3-7.7) Topical anesthetic 20-30 min. or irrigation Recheck pH Cycloplegic drops prevent adhesions between the iris and lens Chemical Injury • Strong Alkalis (pH >11.5) penetrate the eye rapidly and cause intraocular inflammation. • Complications include: infection, glaucoma, conjunctival and corneal scarring Prevention of Eye injury • Protective eyewear should be worn by athletes and patients that are one-eyed – Criteria is visual acuity less than 20/40 in the poorer eye--loss of the good eye would render patient unable to drive legally • Recommended eyewear is frames or goggles with polycarbonate lenses – Need plano lenses if contacts are worn References: • • • • • • • • • • • • • Arbour, JD, Brunette, I, Boisjoly, HM, et al. Should we patch corneal erosions?. Arch Ophthalmol 1997; 115:313 Bienfang, D.C. Overview of diplopia. Online available @ uptodate.com. 12/1/2008. Calhoun, J. Eye examinations in infants and children. Peds in Review 1997; 18:28. Hulbert, MF. Efficacy of eyepad in corneal healing after corneal foreign body removal. Lancet 1991; 337:643. Iqbal, S. Approach to acute vision loss in children. Online available at uptodate.com 6/15/2009 Jackson, H. Effect of eye-pads on healing of simple corneal abrasions. Br Med J 1960; 5200:713. Jacobs, D et al. Corneal abrasions and corneal foreign bodies. Online available @ uptodate.com 11/20/2008 Hodge, C and Lawless, M. Ocular Emerencies. Aust. Fam. Phys. 2008; 37:506 Kaiser, PK. A comparison of pressure patching versus no patching for corneal abrasions due to trauma or foreign body removal. Corneal Abrasion Patching Study Group. Ophthalmology 1995; 102:1936 Klein, B. and Sears, M. Consultation with the specialist: eye injury. Peds in Review 1992;13:127. Luke, A. and Micheli, L. Sports Injuries: Emergency Assessment and Field-side care. Peds In Review 1999;20:291. Stout, Ann. Corneal Abrasions. Peds in Review. 2006; 27:433 Tingley, D.H. Eye trauma: corneal abrasions. Peds in review 1999;20:320