* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Ipoglicemia neonatale persistente: considerazioni su un
Survey
Document related concepts
Transcript
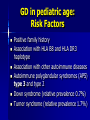
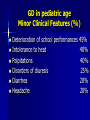
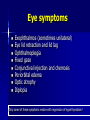
GRAVES’ DISEASE IN ADOLESCENTS Filippo De Luca Pediatric Unit Department of Pediatrics University of Messina, Italy Graves’ Disease (GD) in pediatric age Epidemiology GD accounts for more than 95% of hyperthyroidism cases in childhood Prevalence of GD is approximately 0.02 in childhood, accounting for fewer than 5% of the total cases of GD Female-to-male ratio of 3-6:1 Incidence rate: 0.8/100.000/year Peak Incidence in children aged 10-15 years Monozygotic twins show 50% concordance for GD GD in pediatric age: Risk Factors Positive family history Association with HLA B8 and HLA DR3 haplotype Association with other autoimmune diseases Autoimmune polyglandular syndromes (APS) type 3 and type 2 Down syndrome (relative prevalence 0.7%) Turner syndrome (relative prevalence 1.7%) Pathogenetic Peculiarities of GD In contrast to other autoimmune diseases (HT, celiac disease, type 1 diabetes), GD is traditionally considered an autoantibody-mediated T-helper (TH2) Recent studies cast doubt on this traditional classification and the existence of a clear demarcation between HT and GD In hyperthyroid patients with GD in the active phase, TH1 rather than TH2 cells predominate among peripheral blood lymphocytes After initiation of methimazole, an ongoing transition from TH1 to TH2 occurs Inukai et al Eur J Endocrinol 2007, 156:623 Relationship between Hashimoto (HT) and Graves In pairs of identical twins, one can develop HT and the other GD GD and HT frequently aggregate in the same families They can coexist in the same gland They can occur in the same patient They have the same predisposing HLA aplotype (DR3) HT antecedents in the clinical history of children and adolescents with GD In a study population of 106 children and adolescents with GD, we report a frequency of HT antecedents in 4% of cases The prevalence of this sequence of events is more frequent in Down syndrome (20%) Our reports confirm the existence of a continuum between HT and GD within the spectrum of autoimmune thyroid diseases De Luca et al, Horm Res Paed 2010, 73:473 De Luca et al, EJE 2010,162:591 GD in pediatric age Major Clinical Features (%) Goiter 100% Nervousness and Irritability 100% Tachycardia 90% Hyperreflexia and Hypertension 80% Tremor 75% Excessive sweating 70% Weight loss without loss of appetite 65% Hyperkinesia and behavioral disorders 60% GD in pediatric age Minor Clinical Features (%) Deterioration of school performances 45% Intolerance to heat 40% Palpitations 40% Disorders of diuresis 25% Diarrhea 20% Headache 20% Basedow Ophthalmopathy in pediatric age Frequency varies widely in different series (35-70%) Quite rare and rarely severe in children Especially rare disorders of ocular motility and function More common in countries with higher incidence of youth smoking habit Krassas et al, Eur J Endocrinol 2004, 150:407 Eye symptoms Exophthalmos (sometimes unilateral) Eye lid retraction and lid lag Ophthalmoplegia Fixed gaze Conjunctival injection and chemosis Periorbital edema Optic atrophy Diplopia Only some of these symptoms resolve with regression of hyperthyroidism! Clinical examination of thyroid Goiter is mandatory for the diagnosis of GD! It is rarely detectable from the beginning of clinical picture (this justifies any delay in diagnosis) It is widely diffused and symmetrical A murmur can be detected in cases of major thyromegaly (thyroid enlargement) Clinical picture onset Often insidious , especially in children Initially the most typical symptoms are rare (goiter and ophthalmopathy) Atypical symptoms are more prevalent, especially behavioral disorders, deterioration of school performances and hyperactivity syndrome Growth and pubertal development in GD Acceleration of growth and bone maturation is commonly found Even in pre-pubertal-onset cases, final height is not significantly impaired despite initial bone age advancement Target heights do not differ between males and females Segni et al, Thyroid 1999,9:871 Lazar et al, JCEM 2000, 85:3678 Cassio et al, Clin Endocrinol 2006,64:53 GD peculiarities in Down syndrome No typical female predominance More prevalent than in the general population HT may often precede GD Prevalence of ophthalmopathy is low Response to drug therapy is not poor Goday-Arno et al Clin Endocrinol 2009, 71:110 De Luca et al, EJE 2010,162:591 The detection of autoantibodies to thyrotropin-receptor antibody (TRAb) Commonly used: - in clinical practice for the diagnostic assessment of GD - in differential diagnosis between toxic multinodular goiter and autonomous adenoma. New TRAB assays have specificity and sensitivity > 90% It could have a prognostic value, either at the onset of GD or during treatment Cardia et al, Thyroid 2004, 14: 295 Cappelli et al, Endocrin J 2007, 54:713 TrAb positivity Graves’ Disease Hashimoto’s Thyroiditis Other diagnostic tests in GD (1) Thyroid function tests are crucial for diagnosis confirmation and in d.d. between GD and other cases of hyperthyroidism Evaluation of anti-peroxidase antibody is not very specific, and antithyroglobulin even less so Other diagnositic tests in GD (2) Echographic picture is not different from that of HT Scintigraphy has lost much of its traditional value but may be useful with suspected toxic adenoma Neonatal GD Incidence of < 1% of all pediatric cases No gender predominance Caused by transplacental passage of TSI Clinical signs: tachycardia, hypertension, tremors and hyperphagia without weight gain Goiter and exophthalmos may be absent Complications: craniosynostosis and mental retardation Spontaneous resolution after 3-4 months Subclinical hyperthyroidism More frequent in older patients The only biochemical sign is the suppression of TSH with normal FT4 and FT3 values Increased risk of osteopenia and atrial fibrillation Spontaneous remission in 40% of cases Antithyroid therapy is justified in only the patients aged > 65 yr and in those with cardiovascular and/or osteoporosis problems Ginsberg, Can Med Ass J 2003, 4:168 Hashitoxicosis Not a disease in itself but is the hyperthyroid phase of HT Detectable in 10-15% of all cases at onset of HT Short duration (usually< 6 months) Concurrent with an increase in TPOA and TGA and only rarely in TRAB Generally auto-resolution occurs, developing into euthyroidism or hypothyroidism Responds to antithyroid therapy Toxic adenoma Very rare in pediatric age Mostly benign (not always!) Hashitoxicosis can present in a biochemical fashion that is similar to Graves disease Negative autoimmunity Typical scintigraphic image Other rare causes of hyperthyroidism Exogenous hyperthyroidism Hyperthyroidism in McCune Albright syndrome (MAS) Jod-Basedow thyrotoxicosis HCG producing tumors TSH-secreting pituitary tumor GD Therapy (1) In our very recent multicenter experience methimazole treatment (initial and maintenance dosages 0.46±0.1 and 0.15±0.03 mg/kg/day, respectively) induced a significant remission rate even during the first therapeutical cycle The prevalence of relapse rates after withdrawal of the 1° methimazole cycle was relatively high (31.2%) and further pharmacological cycles were needed in most cases De Luca et al, EJE 2010:162:591 GD Therapy (2) Persistent remission rates after prolonged methimazole withdrawal were 26.7% Non-pharmacological therapies were needed in 11% of cases Definitive remission rates after at least 2 years from withdrawal or after nonpharmacological therapies were obtained in 37.7% of cases De Luca et al, EJE 2010:162:591 Conclusions In young patients, methimazole therapy may be effective to induce transient GD remission but several and prolonged therapeutical cycles are often needed The prevalence of side effects is very low (3.8%) De Luca et al, EJE 2010:162:591