* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download cholesteatoma
Survey
Document related concepts
Transcript
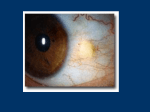
cholesteatoma ธิดา เหล่าไพบูลย์ อาจารย์ที่ปรึ กษา อ.สุ ธี ไกรตระกูล 24/05/60 1 cholesteatoma • Aural cholesteatomas are epidermal inclusion cysts of the middle ear or mastoid • They contain the desquamated debris (principally keratin) from their keratinizing, squamous epithelial lining. 24/05/60 2 Misnomer ? • "cholesteatoma" coined by the German physiologist Johannes Müller in 1838, is a misnomer • because this entity does not contain cholesterol • the white-yellow keratin flakes found within cholesteatomas grossly resemble cholesterol crystals 24/05/60 3 Congenital cholesteatomas PATHOGENESIS • originate : keratinizing epithelium [epidermoid cysts ] within the middle ear cleft, – "skin in the wrong place “ – pearl-like masses behind an intact membrane 24/05/60 4 Congenital cholesteatomas • Most involve the anterior superior quadrant of the middle ear • DDX : myringosclerosis by pneumatic otoscopy 24/05/60 5 Congenital cholesteatomas • Potsic et al. staging system: – stage I : one quadrant – stage II : multiple quadrants without ossicular involvement – stage III, ossicular involvement without mastoid extension – stage IV, mastoid involvement – correlation between stage and risk of residual disease; stage IV carries a 67% risk of residual cholesteatoma 24/05/60 6 MANAGEMENT Congenital cholesteatomas • prompt surgical excision • high-resolution CT scanning of the temporal bone : – extension into the attic and mastoid – Children with extensive disease : second-stage 6 to 12 months after the initial surgery • look for regrowth of microscopic residual disease • reconstruct the ossicular chain. – long-term follow-up : recurrent disease. 24/05/60 7 acquired cholesteatoma 24/05/60 8 The pathogenesis of acquired cholesteatoma There are four basic theories : (1) invagination of the tympanic membrane (retraction pocket cholesteatoma) (2) basal cell hyperplasia (3) epithelial ingrowth through a perforation (the migration theory) (4)squamous metaplasia of middle ear epithelium 24/05/60 9 Invagination of the tympanic membrane • The invagination : attic cholesteatomas • eustachian tube dysfunction (or OME) with resultant negative middle ear pressure • repeated inflammation • The pars flaccida, being less fibrous and less resistant to displacement 24/05/60 10 invagination of the tympanic membrane • retraction pocket deepens • Bacteria can infect the keratin matrix biofilm • primary acquired cholesteatoma results • in the posterosuperior quadrant 24/05/60 11 2. The epithelial invasion Theory • perforation in the tympanic membrane • keratinizing squamous epithelium migrates into the middle ear from • "contact inhibition." • concept of increased migration of the epithelium in those with cholesteatoma 24/05/60 12 2. The epithelial invasion Theory • Cholesteatomas originating after temporal bone fractures • allow ingrowth of keratinizing epithelium by contact guidance • Dimethylbenzanthracene (DMBA) – chemical carcinogen – advancing of the keratinizing squamous epithelium into or under the mucosal layer middle ear cavity and eustachian tube 24/05/60 13 3.Basal Cell Hyperplasia Theory • epithelial cells (prickle cells) of the pars flaccida • invade – subepithelial tissue – lamina propria – basement membrane 24/05/60 14 3.Basal Cell Hyperplasia Theory • formation of microcholesteatomas • perforate secondarily through the tympanic membrane • an attic cholesteatoma. 24/05/60 15 3.Basal Cell Hyperplasia Theory • Substance in cholesteatoma matrix – cytokeratin (CK) 10 ,13 16 – fibronectin and tenascin – Action • Hyperproliferation • Migration • altered differentiation of keratinocytes 24/05/60 16 4. Squamous Metaplasia Theory • inflammation • simple squamous or cuboidal epithelium of the middle ear cleft • metaplastic transformation into keratinizing epithelium. • and contact with the tympanic membrane. 24/05/60 17 4. Squamous Metaplasia Theory • infection and inflammation, • lysis of the tympanic membrane and perforation • typical appearance of an attic cholesteatoma. 24/05/60 18 Diagnosis acquired cholesteatoma • otoscopic examination – typical attic retraction : posterosuperior portion of tympanic membrane • surgical exploration 24/05/60 19 Diagnosis acquired cholesteatoma • High-resolution CT scanning temporal bone – is useful for operative planning – recommended for all revision mastoid operations • MRI temporal bone 24/05/60 20 symptoms of acquire cholesteatoma • Asymptomatic • slowly progressive conductive hearing loss • chronic otitis with purulent otorrhea : most 24/05/60 21 acquired cholesteatoma • malodorous otorrhea : anaerobic bacteria • misdiagnosed : external otitis careful follow-up canal débridement of a patient with otorrhea 24/05/60 22 Middle ear atelectasis • longstanding eustachian tube dysfunction • Negative pressure in middle ear • atelectasis develops • tympanic membrane becomes retracted onto the promontory and the ossicles of the middle ear • tympanic membrane is not adherent to the medial wall of the middle ear • mucosal lining of the middle ear is intact. 24/05/60 23 DDX acquired cholesteatoma • adhesive otitis media – middle ear space is totally obliterated – tympanic membrane is adherent to the ossicles and promontory – mucosal surfaces are not present – erosion of the long process of the incus and the stapes suprastructure 24/05/60 24 four stages of tympanic membrane retraction stage I, retracted tympanic membrane stage II, retraction with contact onto the incus 24/05/60 25 four stages of tympanic membrane retraction stage III, middle ear atelectasis stage IV, adhesive otitis media 24/05/60 26 Management middle ear atelectasis • ventilating tubes • Myringoplasty – hearing loss – ossicular erosion 24/05/60 27 secondary acquired cholesteatoma • keratinizing epithelium has migrated through a perforation into the middle ear 24/05/60 28 secondary acquired cholesteatoma "aural polyp." • An infected cholesteatoma • granulation tissue at the junction between an eroding cholesteatoma and bone. • The presence of an aural polyp in a chronically infected ear should be considered to be a cholesteatoma until proven otherwise. • cholesteatoma cannot be seen otoscopically but will be discovered during tympanomastoid surgery. 24/05/60 29 secondary acquired cholesteatoma • Cholesteatomas are prone to – recurrent infection – erode the bone of the ossicles and the otic capsule. – exhibit typical growth patterns into the temporal bone. • The pars flaccida may invaginate into – Lateral most portion of the epitympanum (Prussak's space) – recesses of the epitympanum posteriorly, lateral to the body of the incus, inferiorly into the middle ear by way of the pouch of von Tröltsch – anteriorly into the protympanum 24/05/60 30 Prussak space 24/05/60 31 • Prussak’s space connected to Posterior Pouch von Troeltsch which opens up into Mesotympanum 24/05/60 32 The Prussak’s space connects • anterior pouch von Troeltsch and the mesotympanum (Anterior Tympanic Space) • Posterior Pouch Von Troeltsch connections to the Posterior 24/05/60Tympanic Space. 33 Posterior mesotympanic cholesteatoma • retraction of the posterior portion of pars tensa • invades – sinus tympani – facial recess – Extension to mastoid occurs medial to ossicle heads 24/05/60 34 Anterior epitympanic cholesteatoma • Invagination of epitympanum anterior to malleus head and neck creates a cholesteatoma sac • threatens horizontal facial nerve and geniculate ganglion. • Forward extension into supratubal recess is common 24/05/60 35 BACTERIOLOGY OF INFECTED CHOLESTEATOMAS 24/05/60 36 Complications • bone erosion – Ossicles : most incus – otic capsule : most lateral semicircular canal – facial nerve canal – tegmen tympani – tegmen mastoideum 24/05/60 37 Complications – Sensorineural hearing loss : • secondary suppurative labyrinthitis • cochlear hair cell loss adjacent to cholesteatoma 24/05/60 38 Extratemporal (extracranial) complications Subperiosteal abscess • Cholesteatoma can block the aditus ad antrum • preventing communication of the infected contents of the mastoid with the middle ear space and the eustachian tube • This obstruction increases the possibility of infectious decompression through the mastoid cortex. 24/05/60 39 Subperiosteal abscess • systemic symptoms – fever and malaise • local signs – protruding auricle that is laterally and inferiorly displaced – fluctuant, erythematous, tender area behind the ear. • CT scan can demonstrate abscess – cortical defect in the mastoid 24/05/60 40 Subperiosteal abscess • abscess is drained • mastoidectomy is performed and the cholesteatoma matrix is removed in the standard manner. 24/05/60 41 Bezold's abscess • cervical abscess deep to the sternocleidomastoid • mastoid cortex is violated at its tip, as opposed to its lateral cortex • Partway : – direct extension – mastoid vein phlebitis • more common AOM with mastoiditis • complication of COM with cholesteatoma 24/05/60 42 Bezold's abscess • A contrasted CT scan of the neck and mastoid : – rim-enhancing abscess with surrounding inflammation – bony dehiscence in the tip of the mastoid, • Management : – drainage of the cervical abscess through a transcervical approach – combined with a cortical mastoidectomy 24/05/60 43 Labyrinthine fistulae • most common complications of chronic otitis with associated cholesteatoma • The risk of significant sensorineural hearing loss as a result of surgical manipulation makes the open labyrinth – pressure from the cholesteatoma 24/05/60 44 Labyrinthine fistulae • horizontal semicircular canal is the most common • Erosion of the bone of the otic capsule – activated mediators from the matrix 24/05/60 45 Diagnosis Labyrinthine fistulae • subjective vertigo : 62% to 64% of patients • positive fistula test on examination : 32% to 50% of patients • sensorineural hearing loss is found in most of these patients (68%), • this classic picture is not sensitive in the preoperative identification of a fistula 24/05/60 46 Labyrinthine fistulae • the ability to detect fistulae accurately on preoperative CT has been reported as 57% to 60% • in current reports CT scans are no more sensitive than history and physical examination in detecting labyrinthine fistulae. • The definitive diagnosis : intraoperatively 24/05/60 fistula (arrow) of lateral semicircular canal from cholesteatoma 47 Management Labyrinthine fistulae A tympanomastoidectomy • the most appropriate approach to the fistula is to perform a canal wall down mastoidectomy • remove the bulk of the cholesteatoma, and leave the fistula covered with the matrix exteriorizing it into the cavity • then re-operation 9-12 months after first operation 24/05/60 48 Labyrinthine fistulae • In small fistula (<2mm) 2 , cholesteatoma matrix gently removed from fistula +repaired with soft tissue graft (eg, fascia, Intraoperativepicture perichondrium), bone of a horizontal canal fistula pate 24/05/60 49 Facial paralysis • usually occurs with a dehiscent fallopian canal within its tympanic segment, • allowing direct contact of inflammatory mediators • dehiscent nerve, • bony erosion. slowly progressive facial paralysis Diagnosis 24/05/60 50 Facial paralysis • The diagnosis facial paralysis – COM, or cholesteatoma – CT scan is not required, it can be useful in therapeutic planning and patient counseling – cholesteatoma involves the fallopian canal ass. • labyrinth • tegmen 24/05/60 51 Facial paralysis • Coronal CT scan demonstrating involvement of tympanic facial nerve (arrow) from cholesteatoma (arrow heads) causing lateral semicircular canal fistula 24/05/60 52 Management • mastoidectomy is performed to remove the cholesteatoma or granulation tissue that is contacting the facial nerve. • The nerve is approached on both sides of the involvement • diamond burr is used to expose the epineurium on either side of the diseased segment. • Once the proximal and distal segments of the fallopian canal have been opened • blunt dissection is used to remove the disease from the epineurium. 24/05/60 53 24/05/60 54 24/05/60 55 Congenital cholesteatoma of the temporal bone ? • divided into four anatomic groups: 1. middle ear DDX congenital auditory canal cholesteatomas 2. perigeniculate area 3. petrous apex 4. cerebellopontine angle. 24/05/60 56 Perigeniculate and petrous apex cholesteatomas • present – insidious or rapidly progressive facial nerve paralysis – Sensorineural hearing loss from labyrinthine or internal auditory canal erosion is common – conductive hearing loss also may result from cholesteatoma extension into the middle ear or blockage of the eustachian tube. 24/05/60 57 Perigeniculate and petrous apex cholesteatomas – Facial twitching may occur in the presence of congenital cholesteatomas and with facial nerve neuromas. – Vestibular dysfunction may complete the symptom complex. – the cholesteatoma may erode into the middle or posterior fossa and expand markedly before producing symptoms 24/05/60 58 Perigeniculate and petrous apex cholesteatomas • left cerebellopontine cistern congenital epidermoid cyst • A, Axial computed tomography (CT). Displacement of the pons DDX :arachnoid cyst • B, Axial magnetic resonance imaging T1-weighted, no contrast. – This slightly higher signal on T1-weighted images is helpful in separating epidermoid cysts from arachnoid cysts.. 24/05/60 59 Perigeniculate and petrous apex cholesteatomas • MRI will provide further definition – congenital cholesteatomas • almost always slightly higher signal T1-weighted images • moderately high signal on T2-weighted images – bone marrow fat • high signal on T1-weighted images • fade dramatically on T2-weighted images. – Typical effusions • low signal on T1-weighted MRI • high signal on T2-weighted MRI. – Giant cholesterol cysts :show capsular enhancement. 24/05/60 60 Surgical management of a congenital cholesteatoma • complete removal of the cholesteatoma matrix • The isolated middle ear cholesteatoma – removed transtympanically – Routine middle ear reconstructive techniques may be used if ossicles are eroded or removed or if the tympanic membrane is sacrificed. 24/05/60 61 Perigeniculate and petrous apex cholesteatomas • congenital cholesteatomas of the perigeniculate area or petrous apex – Transmastoid – middle cranial fossa approach – the transsphenoidal approach – combination of these procedures 24/05/60 62 Cholesteatoma vs. Temporal bone fracture There are four pathogenic mechanisms for posttraumatic cholesteatoma formation: (1) epithelial entrapment in the fracture line (2) ingrowth of epithelium through the unhealed fracture line or a rent in the tympanic membrane (3) traumatic implantation of tympanic membrane skin into the middle ear (4) trapping of epithelium medial to a stenosis of the EAC. 24/05/60 63 posttraumatic cholesteatoma formation • The typical location : epitympanum and the antrum. The fracture line along the posterior superior canal wall and scutum expands and then closes • Traumatic implantation of tympanic membrane skin will result in cholesteatoma formation within the mesotympanum. • Blast injuries can result in the displacement of keratinizing stratified squamous epithelium into the mastoid air cells, the mesotympanum, the epitympanum, and even intracranially 24/05/60 64 Management posttraumatic cholesteatoma formation • careful follow-up – Débridement – stenting when narrowing progresses : ear mold – canal is adequately dilated : Oto-Wicks (Meditronic Xomed, Jacksonville, Fl) 24/05/60 65 Management posttraumatic cholesteatoma formation • canalplasty – Complete stenosis – dilation is not possible 24/05/60 66 24/05/60 67