* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Fibromyalgia and the Social Construction of Disease
Survey
Document related concepts
Transcript
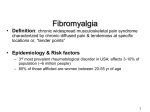
Fibromyalgia and the Social Construction of Disease Salahuddin Kazi, MD • In 1990 the American College of Rheumatology published criteria for the classification of fibromyalgia • Fibromyalgia was defined as a syndrome of widespread pain associated with characteristic tender points Pain Fatigue Sleep Disorder Fibromyalgia Chronic Fatigue Syndrome Irritable Bowel Syndrome Migraine Headaches Interstitial Cystitis Fibromyalgia is a controversial disorder Valid Disease Construct OR Universal Stress + Doctor + Social Sanction “Fibromyalgia” Doctors are ambivalent about fibromyalgia • Diagnosed by self-report • Objective findings limited to tender points • No characteristic laboratory or imaging abnormalities • Overlap with other syndromes • No specific treatment The argument • If fibromyalgia is a true disease, there ought to be observable pathologic lesions • But what do we mean by “disease”? Fibromyalgia – key features • Fibromyalgia is characterized by widespread chronic muscle pain • The pain worsens with activity • Patients cannot distinguish well between myalgia and arthralgia – often describe joints as being swollen – burning, numbness, tingling and heaviness of the limbs are common complaints Fibromyalgia – key features • Fatigue is very frequent (90%) and may be the presenting complaint • Sleep disorders are universally reported • Mood disturbance, cognitive impairment, headache, Raynaud’s phenomenon and pre-syncope are also very prevalent • Some patients meet formal criteria for depression Fibromyalgia – key features • Many individuals meet criteria for other unexplained clinical syndromes – irritable bowel syndrome, chronic fatigue syndrome, migraine headaches and interstitial cystitis • Physical examination is largely normal except for the finding of characteristic tenderness at defined points • Laboratory studies are within normal limits Fibromyalgia - epidemiology • Fibromyalgia is more common in women • Prevalence increases linearly with age – 2% at age 20 and 8% at age 70 • Peak presentation is in the fourth and sixth decades of life • In 50%, onset is attributed to trauma or a flu-like illness Chronic fatigue syndrome Sore Throat Muscle Pain Multi-Joint Pain Fatigue Headaches Tender Lymph Nodes Post Exertional Malaise Unrefreshing Sleep Unexplained clinical syndromes • Fibromyalgia • Chronic fatigue syndrome • Irritable bowel syndrome • Multiple chemical sensitivity • Migraine headaches • Interstitial cystitis • Chronic nonbacterial prostatitis • Chronic pelvic pain • Chronic low back pain • Post-concussion syndrome • Interstitial cystitis • Temporomandibular disorder Tender Points Sleep Disturbance Pain The history of fibromyalgia and chronic fatigue syndrome • 1869 • 1904 • 1930’s • 1938 • 1976 • 1980’s • 1990’s Neurasthenia Fibrositis Epidemic neuromyasthenia Benign myalgic encephalomyelitis Post viral syndrome Referred muscle pain Fibromyalgia Chronic EBV infection Chronic fatigue syndrome Fibromyalgia – ACR definition Myofascial pain syndrome Pathophysiology of fibromyalgia: evolving views • • • • Disease of muscle Psychiatric disorder Disease of pain perception Neuroendocrine disease Pathophysiology of fibromyalgia: evolving views • • • • Disease of muscle Psychiatric disorder Disease of pain perception Neuroendocrine disease Is there muscle pathology in fibromyalgia? • Stockman,1904 - biopsy studies of palpable tender nodules in patients with fibrositis “inflammatory hyperplasia” • Two subsequent studies could not confirm these findings Is there muscle pathology in fibromyalgia? • Collins,1940 - review of original specimens found no evidence of inflammation • Contemporary muscle biopsy studies have revealed either normal findings or nonspecific ultrastructural changes • Studies of muscle metabolism and MR spectroscopy have also failed to demonstrate abnormalities in muscle metabolism Pathophysiology of fibromyalgia: evolving views • • • • Disease of muscle Psychiatric disorder Disease of pain perception Neuroendocrine disease Is fibromyalgia a psychiatric disorder? • Prior to the 1980’s the concept of “psychogenic rheumatism” was prevalent: – dramatic urgency to be seen by the doctor – written list of complaints – large volume of previous investigations brought to the first clinic visit Fibromyalgia and the MMPI • Payne, 1982 - higher MMPI scores in fibromyalgia patients when compared with patients with arthritis • Fibromyalgia patients scored higher on the hypochondriacal and hysteria scales but not on the depression scale Fibromyalgia and the MMPI • Smythe suggested that the MMPI will rate any patient with chronic pain high on the hysteria and hypochondriasis scales • Pincus reported that elevated MMPI scores for hypochondriasis, depression and hysteria correlated with disease activity in patients with rheumatoid arthritis Fibromyalgia - history of depression • Clarke - fibromyalgia patients from general practice – No increase in rates of psychologic disturbance • 50%-70% of patients with fibromyalgia report a personal history of depression • Current major depression is found in not more than 36% of patients Fibromyalgia and depression: prospective data • A prospective study of 175 women with self-reported pain – designed to examine etiologic factors in the onset of fibromyalgia • Depression developed in 25% of this cohort after a period of 5.5 years • Self-reported depression was the single strongest predictor (six-fold) of new-onset fibromyalgia Fibromyalgia and depression: prevailing views • Depression and fibromyalgia are associated, but the nature of the association and the temporal relationship are unclear • Fibromyalgia and major depression may share a common etiologic abnormality • The greater frequency of depression in fibromyalgia patients in referral-based practices versus fibromyalgia patients in the community reflects differences in health-seeking behaviors Community Fibromyalgia + Depression Fibromyalgia Clinic Health Seeking Fibromyalgia + Depression Is fibromyalgia a somatization disorder? Patients have multiple somatic complaints that suggest organic disease: • • • • • Severe fatigue Abdominal pain Diarrhea Headaches Dizziness • Jaw pain • Paraesthesia • Raynaud’s phenomenon • Dysuria Fibromyalgia and somatization • Most patients with fibromyalgia would not satisfy diagnostic criteria for somatization disorder • Do these patients may have a subsyndromal somatization state? Critics point to the circular nature of the definition of somatization disorder: “a psychiatric diagnosis that depends on the presence of physical symptoms that suggest organic disease and are not explained by a general medical condition would become a nonpsychiatric diagnosis once the general medical condition adequately explains the symptoms” Pathophysiology of fibromyalgia: evolving views • • • • Disease of muscle Psychiatric disorder Disease of pain perception Neuroendocrine disease Fibromyalgia as a chronic pain disorder: epidemiology 2000 Healthy Adults 11.2% reported Chronic Pain 21.5% had >10 Tender Points 63.8% had 1-10 Tender Points Criteria for Fibromyalgia the number of tender points correlated best with depression, fatigue and poor sleep Fibromyalgia as a chronic pain disorder: epidemiology • Wolfe – rural Kansas – widespread pain was more common in women – increased in prevalence with age – peak 23% by the seventh decade The pain-fibromyalgia spectrum Chronic Pain Fatigue Depression Sleep Disorder Fibromyalgia Fibromyalgia: abnormal central sensory processing • Non-nociceptive pain (NNP) – pain elicited by stimulation of fibers that usually relay non-painful signals to the spinal cord – non-noxious stimuli are subverted by abnormal central processing resulting in the experience of pain Chronic pain in fibromyalgia • Several studies of chronic pain in fibromyalgia patients compared with controls show: – dolorimetry reveals a lower pain threshold – elevated substance P levels in the CSF – with isometric muscle contraction, the pain threshold decreases rather than showing the expected increase seen in controls – somatosensory-induced potentials demonstrate increased amplitude following laser stimulation of skin – distinctive regional cerebral blood flow abnormalities Pathophysiology of fibromyalgia: evolving views • • • • Disease of muscle Psychiatric disorder Disease of pain perception Neuroendocrine disease The hypothalamic-pituitary-adrenal (HPA) axis • Primary endocrine stress axis • Adaptational response to stressors • Patients with fibromyalgia have abnormal stress activation Neuroendocrine abnormalities in fibromyalgia • Elevated cortisol levels with a flattened diurnal pattern that are not suppressed by dexamethasone administration • Low 24 hour urinary free cortisol suggesting elevated cortisol secretion during the day and suppressed secretion at night • Markedly enhanced ACTH release when CRH is injected, but with no increase in cortisol levels (suggesting adrenal hyporesponsiveness) Significance of HPA abnormalities • Chronic CRH hyperactivity is driven by stress and pain • CRH is a pleiotropic hormone – changes in the set points of other hormonal axes like growth hormone, gonadotropin and thyroid stimulating hormone may also be of significance Significance of HPA abnormalities • Whether somatic symptoms in fibromyalgia are caused by these abnormalities is unclear • Is the link between somatic complaints and central nervous system changes bidirectional? Stressful life event HPA Axis Genetic vulnerability Abnormal central sensory processing Chronic pain Somatosensory amplification Psychosocial distress Secondary somatic symptoms Acute Pain Summary of the current concept of fibromyalgia • Theories of the pathophysiology of fibromyalgia have moved from a disorder of soft tissues to one of chronic pain • Diagnosis is largely based on patient self-report but an increasing body of literature points to measurable phenomena in the central nervous system and HPA axis • Psychologic disturbances are common in patients with fibromyalgia but the temporal association with disease onset is still unclear Patient Doctor Disease Society Foucault’s “spaces” • Primary spatialization: disease is described and ordered as a concept • Secondary spatialization: disease is given a place within the body • Tertiary spatialization: the disease and the diseased individual are located within the societal body Concept Body Society The birth of biomedicine • Turn of the 18th century • French revolution – Restructuring of French society – Parallel restructuring of the medical paradigm The birth of biomedicine • Medicine changed from a study of symptoms to the precise mapping of signs and symptoms to observable pathologic lesions • Doctors began to care for indigent patients in a hospital setting • The doctor became dominant in the doctor-patient relationship The biomedical model of disease • Disease is caused by an observable pathologic lesion in the body • The presence of a pathologic lesion is revealed in two ways: – symptoms, the patient’s perception that body function is not normal – signs, the physician’s observation that signifies that an underlying lesion exists Assessing symptoms • Patients subject their symptoms to some form of evaluation prior to seeking medical advice • Community surveys suggest that the ratio of symptom episodes to consultation is much higher than one would expect Symptom : consultation ratio Headache 184:1 Backache 52:1 Emotional problem 46:1 Abdominal pain 28:1 Sore throat 18:1 Pain in chest 14:1 The active decision to seek medical advice for symptoms is known as illness behavior – Trivial symptoms – Trivialize symptoms Decision to see the doctor • Perceived interference with vocational or social activity • Perceived interference with social or personal relations • The occurrence of an interpersonal crisis • Failure of symptoms to resolve by the end of a self-determined arbitrary period • Coercion from friends or relatives (sanctioning) Not all persons with fibromyalgia are “patients” • Community surveys: – fibromyalgia non-patients > fibromyalgia patients • A history of depression > current depression – history of depression is a marker for persons more likely to seek health care • The “onset” of fibromyalgia following an interpersonal crisis – a stressful life event, and not the disease itself, precipitates a consultation Parson’s “sick role” • Strong position of social authority of the doctor to legitimize illness • Allows the patient to ease from a “well person” to a “patient” Benefits of the “sick role” • The patient is temporarily excused from performing his or her normal social role • The patient is not held responsible for his or her illness Sick role: patient’s obligations • The patient must want to get well (the sick role is of temporary status) • The patient must cooperate with the treatment plan Parson’s model fails in chronic illnesses • Inability of the patient to fulfill the two obligations • The sick role is not temporary • Lack of cure makes cooperating with treatment difficult to sustain Parson’s model also fails when: • Patients have multiple complaints without a readily identifiable lesion • The patient does not accept a shared belief in the biomedical model of disease The doctor as an agent of social control • Doctors utilize the biomedical rule of medicine to judge patients as ill or well – Conferring/withholding “sick role” status • This judgment occurs independently of the patient’s own beliefs The doctor as an agent of social control • Patients may be judged ill even though they may view themselves as well – screening asymptomatic patients • judged to be well, even when they see themselves as ill – no biological explanation for the patient’s symptoms Good patients, bad patients and great patients Lober-1975: study of inpatients in a general hospital • good patients – trusting, cooperative, non-complaining, non-demanding • great patients – seriously ill patients who were cheerful, cooperative, uncomplaining, and objective about their illness • difficult or problem patients – not seriously ill but were demanding, emotional, and uncooperative – frequently discharged early, given sedatives, or referred to psychiatry “Difficult patients” in primary care Hahn-1996: • 15% of patients were viewed by doctors as difficult patients • More likely to have: – psychiatric disorder – functional impairment – greater health-care utilization – higher dissatisfaction with their care So, what’s “difficult”? • “Difficult” because patients have presented with “problems of living” rather than defined diseases • The question of secondary gain – the hope of attaining the benefits of the sick role • The doctor is reticent to exercise his or her unique social authority to grant these benefits • The doctor views such patients as “difficult” because they do not fulfill the construct of the biomedical model Patients with fibromyalgia are “difficult” • A chronic illness without a readily identifiable lesion • Multiple somatic complaints • Higher incidence of psychiatric disorders • Greater health care utilization • Dissatisfaction with their care • Advice of the doctor is often not followed The patient with fibromyalgia may present with a comprehensive belief system that rivals the biomedical scientific belief system of the doctor While on the surface the doctor-patient relationship is seemingly about common interests and goals cause diagnosis diagnosis cause therapy therapy Medical epidemiology Lay epidemiology Disease and labeling theory • A doctor’s decision to interpret an individual’s particular biologic state as being abnormal (diseased or ill) constitutes a label (diagnosis) • In social theory, labeling has a negative connotation • Individuals deemed abnormal are labeled “abnormal” • If this abnormality is also socially abnormal, it can cause deviance Deviance • Primary deviance – defining a biologic state as abnormal • Secondary deviance – change in patient behavior as a consequence of labeling (diagnosis) • Strong social pressures to conform to the label reinforce secondary deviance – “self-fulfilling prophecy” Fibromyalgia the label • Patients with widespread pain and multiple tender points – labeled as suffering from fibromyalgia • Social meaning and significance of the applied label (secondary deviance) – change in behavior – pressure to conform to the diagnosis Is fibromyalgia a deviant label? Critics of fibromyalgia, the label: – The doctor is creating secondary deviance – The labeled patient falls into a self-fulfilling prophecy trap – The label (not the underlying biologic state) perpetuates the illness behavior – By declaring “normal aches and pains” a disease, doctors are promoting the sick role and creating unnecessary somatization Patients may also reject fibromyalgia • Avoidance of stigmatization • Adoption of a more “acceptable” disease – “Systemic lupus erythematosus” • Fibromyalgia + positive ANA – “Lyme disease” • Fibromyalgia + positive Lyme titre Fibromyalgia: a useful construct? • Patients are comforted when they can give their symptoms a name • The conferring of the sick role relieves them of personal responsibility for the cause of their symptoms • These set of symptoms can be studied in a uniform manner Is fibromyalgia a disease, a syndrome or an assortment of unexplained symptoms? What is disease? • The traditional view: – disease is a biological problem – excludes conditions without known biological mechanisms – assumes that the line between physiology (normal) and pathology (abnormal) is welldemarcated Are psychiatric conditions diseases? • No clearly defined biological mechanisms • Manifestations are principally in altered behavior – Cause or consequence of labeling? • Szasz has argued that psychiatrists do not identify real disease, they simply label inappropriate behavior and call it disease Is disease dis-ease? • Dis-ease: lack of feeling well constitutes disease • Unacceptable to doctors because – Definition of disease is firmly in the grasp of the patient – Synonymous with the lay concept of illness – Objectivity succumbs to subjectivity – Presymptomatic disease states cease to exist Disease as social variance Disease Abnormal Social Disadvantage Normal Abnormal Variation from normal is only a disease if it creates social disadvantage Disease and social norms • Osteoarthritis may be viewed as a normal consequence of aging • Dyslexia would not be a disease in a preliterate society • Is obesity a disease? • How is insanity defined? Fibromyalgia can be viewed as a disease based on the social construct (because it causes social disadvantage) BUT Fibromyalgia is typically considered a nondisease because it resists biologic reductionism and is often viewed as a collection of unexplained symptoms The usual fate of unexplained symptoms Unexplained symptoms Referral to psychiatry Somatosensory Amplification loop Doctor shop Patient wants to avoid the stigma of a psychiatric label Adopt a disease with a more socially acceptable label Dissatisfaction with care Secondary deviance Join an advocacy group lobby for reform Explaining unexplained symptoms • One third of all symptoms in primary care settings are unexplained • Unexplained symptoms were originally considered functional disturbances of the brain – reversible Explaining unexplained symptoms • Unexplained symptoms became the province of psychiatry – hardwired • Somatization was proposed as the mechanism by which mental disorders became physical symptoms • Sharpe has suggested that we resurrect the original meaning of the term “functional” • It is difficult to accommodate fibromyalgia in the biomedical disease construct since it is a subjective diagnosis • Biomedical science thrives on objectivity • But is biomedicine itself influenced by social forces? Is the biomedical model impervious to social forces? • Paradigms vs. independent scientific inquiry (Kuhn vs. Popper) • “Reality” and the “knowledge” that explains it - is socially determined Paradigms vs. independent thought • Scientific inquiry is based on prevalent paradigms • Prevailing paradigms are subject to social influence • Unexplained phenomena are “puzzles” not independent “problems” • New paradigms are adopted when the unexplained is explained • A new cycle starts Paradigm Puzzle Solution Kuhn • Scientific growth is series of temporarily valid solutions that provide successively better explanations • The scientist is one of many working to validate an established paradigm • Truth is relative and it subject to newer, better paradigms when appropriate vs. Popper • Scientific growth is a journey towards an infinite absolute truth • The scientist functions in an atomistic, individualistic fashion • Truth is absolute Neurasthenia and chronic fatigue: a biosocial model Neurasthenia Chronic Fatigue Syndrome Era 19th Century 20th Century Prevailing scientific paradigms •Electricity •Thermodynamics •Evolution •Infection •Immunity •Environmental toxins Mechanism •Consumption of finite nervous energy •Survival of the fittest •Chronic infection •Immunosuppression •Chemical sensitivity Social cause •Demands and stresses of modern times •Demands and stresses of modern times Conclusions • Fibromyalgia is a complex biosocial construct shaped by the interaction between biology and sociology • It can only be resolved by creating an alliance between classical biomedical thought and the forces that influence the expression of illness in society Conclusions Fibromyalgia Search for Pathology HPA axis Social Factors Neurobiology of pain Biosocial Model of Disease