* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Development QOD Review
Depression in childhood and adolescence wikipedia , lookup
Rett syndrome wikipedia , lookup
Parent management training wikipedia , lookup
Intellectual disability wikipedia , lookup
Learning disability wikipedia , lookup
Child and adolescent psychiatry wikipedia , lookup
Child psychopathology wikipedia , lookup
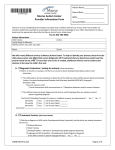
QOD Development During the health supervision visit for an 18month-old boy, his parents express concern that he is vocalizing but not saying any real words. He is holding a small piece of string that he moves back and forth repeatedly. When you call his name, he does not respond. You point to the light in the room and say "look," but he continues to look at the string with a sideways glance. You try to get him to look at you, but he avoids eye contact. Of the following, the MOST likely diagnosis for this boy is 1. 2. 3. 4. 5. Asperger disorder autistic disorder expressive/receptive language disorder obsessive-compulsive disorder Rett syndrome Question 1 Answer B The child described in the vignette shows clinical features of an autistic disorder, a heterogeneous neurodevelopmental disorder (see Table 1 at http://pediatrics.aappublications.org/cgi/content/full/120/5/1183 for complete diagnostic criteria). Affected individuals have impairments in three specific areas: reciprocal social interactions, verbal and nonverbal communication, and range of activities or interests. The clinical presentation is specific to the child, with differing degrees of impairment in each of the three core symptom areas. The hallmark of autism is abnormal social interactions. Children lack the ability to share interests with others (joint attention skills) using verbal or nonverbal communication. They commonly show weakness in eye contact. Their interaction may range from aloofness and an unawareness of other people to having varied or odd interaction with others. Language development commonly is delayed, and children may have immediate or delayed echolalia, unusual intonation, and repetitive speech. Children who have autism may engage in repetitive play and show little imaginative play. They may focus on sensory aspects of objects or develop obsessions about unusual objects (stop signs, elevators). They often have difficulty handling transitions and may engage in repetitive hand or body movements. Many affected children have cognitive impairment. Children who have subthreshold clinical features (some but not all of the features) may receive the diagnosis of pervasive development disorder-not otherwise specified within the autism spectrum. Red flags of development that warrant further evaluation for possible autism include: No babbling by 9 months No gesturing by 12 months No single words by 16 months No functional nonecholalic 2-word phrases by 24 months Any loss of language or social skills at any age Neither a diagnosis of expressive language disorder nor obsessive-compulsive disorder would account for the impaired social engagement exhibited by the boy in the vignette. Individuals who have Asperger syndrome (Asperger disorder in DSM-IV TR) have impairments in social interaction and restricted interests and activities, but they have relatively preserved cognitive and language functioning, in contrast to the delays in developing language reported for the child in the vignette. Rett syndrome almost exclusively affects females and presents with a slowing of motor development between 6 and 18 months of age. Between ages 1 and 4 years, the child exhibits a decline in social interactions, cognitive abilities, purposeful hand movements, and speech. American Board of Pediatrics Content Specification: Know the clinical features of autism spectrum disorder During the health supervision visit for a 4-year-old girl, her father reports that she has developed a stutter over the past 9 months. He explains that she is a little frustrated by the difficulty in expressing herself but otherwise seems happy and well-adjusted. In talking with the father, you also note that he has a mild stutter. He speaks to the child slowly and deliberately and encourages her to take her time when speaking to you. Of the following, the risk factor that MOST strongly suggests the need for speech therapy for this girl is the 1. 2. 3. 4. 5. age of onset child's reaction to stuttering child's sex father's stutter time since onset Question 2 Answer D • The onset of stuttering typically occurs during the period of intense speech and language development as the child progresses from two-word utterances to the use of complex sentences, generally between the ages of 2 and 5 years but sometimes as early as 18 months. About 5% of all children go through a period of stuttering that lasts 6 months or more. The sex ratio for stuttering appears to be equal at the onset of the disorder, but studies indicate that three to four times as many boys continue to stutter. Between 75% and 80% of children who start to stutter stop within 12 to 24 months without speech therapy. Children who begin stuttering before the age of 3½ years and girls are more likely to outgrow stuttering. Strong evidence shows that almost all children who stutter have a family member who stutters. Studies have shown that individuals who stutter have a large degree of within-word dysfluencies compared with their typical peers. Examples are: 1) repetition of individual sounds or syllables such as "W-w-w-what is he doing?", 2) prolongation of words such as "Wwwwwwhat is he doing?, and 3) blocks or pauses such as ". . . What is he doing?" Such dysfluencies may be associated with eyelid closing and physical tension around the lips. The standard criteria for diagnosing a child who has stuttering or is at risk to develop stuttering is an average of at least three withinword dysfluencies in 100 words of conversation. Although the girl described in the vignette does not have a strong negative reaction to her speech impediment, her father stutters, placing her at risk for problematic stuttering and indicating the need for speech therapy. Criteria for referring children who stutter for speech therapy are presented in (Item C107). Referral should be made for children who have severe stuttering problems, those who have mild stuttering problems that do not improve markedly within 6 to 8 weeks, or those whose parents are very concerned. Referral also is indicated for children who have associated behaviors (eg, head, body, or limb movement; audible breathing prior to the disfluencies; and observable muscle tension in the orofacial region). In time, such children may develop anxiety about stuttering that could contribute to the chronicity of the disorder. American Board of Pediatrics Content Specification: Know the indications for referral of a child to a speech pathologist for evaluation of stuttering Item C107 The parents of a newborn in whom a congenital severe-profound hearing loss has been diagnosed are seeking guidance about how to promote their infant's language development. You recommend enrollment in an early intervention program and obtaining hearing aids when the infant is young. His parents have never been exposed to an individual who has a hearing loss. They ask your opinion on the best approach for him to learn language. Of the following, the MOST important factor in language development of an infant or young child who has hearing loss is the use of 1. 2. 3. 4. 5. a high amount of verbal/nonverbal (gestures) communication between parents and child an oral-aural method emphasizing the teaching of speech and the use of a child's residual hearing hand-cued speech (using combined speech and hand cues) manually coded English between parents and child the bilingual (ASL and English)-bicultural (hearing and deaf culture) approach Question Answer A Multiple factors contribute to a family's decisions regarding their child who has confirmed hearing loss. Language-based early intervention results in superior expressive and receptive communication abilities compared with those of children identified at later stages of development. Family involvement, including verbal and nonverbal (gestures) communication, has a more significant positive effect on language development than any specific type of intervention. Hand-cued speech (www.cuedspeech.org) consists of eight different handshapes (represent consonants) and four different hand locations around the speaker's face (represent vowels). Manually coded English employs a visual representation of the spoken English language. Signs and finger spelling are used to represent spoken English. The goal of the oral-aural method of communication is to develop spoken language and gain inclusion in the mainstream both in school and society. People who employ this auditory-oral approach use their aided residual hearing as well as reading of speech, facial expressions, and naturally occurring gestures. Such an approach requires consistent use of hearing aids/FM technology and provision of auditory training and speech therapy as well as lip-reading. The bilingual-bicultural (Bi-Bi) philosophy of the National Association of the Deaf (www.nad.org) promotes communication in two languages (visual and a form of spoken) for children who are deaf so they can be a part of both deaf and hearing communities. The Bi-Bi approach supports early language learning through American Sign Language (ASL) and a form of spoken English taught as a second language later in elementary school. Of note, children who have hearing loss of less than 90 dB usually benefit from conventional amplification systems. For children who have severe-to-profound sensorineural hearing loss affecting both ears, cochlear implantation may be considered. This procedure leads to the ability to perceive sound signals. Although results are highly variable, the procedure is most successful when undertaken early in life. American Board of Pediatrics Content Specification Know the major approaches to education of the deaf child A well-nourished, healthy child comes to your office for his 2-year health supervision visit. You find that he has failed an autism-specific screening tool (the Modified Checklist for Autism in Toddlers) completed by his parents while in the waiting room. Results of a previous audiology evaluation are normal. His head circumference and growth parameters are normal. Findings on a general physical examination are unremarkable, and the neurologic examination produces nonfocal findings. Muscle mass, strength, and tone are within normal limits. His deep tendon reflexes are physiologic and symmetric. Of the following, the MOST appropriate next step is 1. 2. 3. 4. 5. early intervention referral genetics evaluation head MRI metabolic evaluation sleep-deprived EEG Question 4 Answer A The boy described in the vignette has failed The Modified Checklist for Autism in Toddlers (M-CHAT). The M-CHAT is an autism-specific screening tool that has a sensitivity of 0.85 and a specificity of 0.93. The sensitivity measures the percentage of individuals correctly identified as having autism (85%). The specificity measures the percentage of individuals who are correctly identified as not having autism (93%). The results described for the boy in the vignette suggest that he has autism, and the clinician should not wait to confirm the diagnosis before referring the child for early intervention services. Such services are beneficial in addressing the child's deficits. If the diagnosis is confirmed, the interventions may be altered to a more specific intervention for autism spectrum disorder (ASD). ASDs are biologically based neurodevelopmental disorders. Although genetic evaluation may be indicated, especially when there is a family history of autism, referral for early intervention is more likely to improve the child's prognosis than genetic evaluation. Some of the conditions that are associated with autism include fragile X syndrome, tuberous sclerosis, fetal alcohol syndrome, Angelman syndrome, and Rett syndrome. There are only a few reports of mitochondrial or metabolic abnormalities being associated with ASD, and most affected children have normal immune function. No relationship has been demonstrated between autism and the measles, mumps, rubella vaccine or thimerosal. There is no evidence that sleep-deprived electroencephalography and magnetic resonance imaging for children who have ASDs is needed in the absence of specific clinical findings (eg, seizures, hypopigmented macules). Because metabolic abnormalities rarely are associated with autism, metabolic evaluation also is not warranted. American Board of Pediatrics Content Specification: Know the medical causes of autism spectrum disorder A baby girl for whom you provide care has been referred on her newborn hearing screen. Physical examination results are within normal limits. When she is referred on a follow-up hearing screen at 2 weeks of age, you recommend auditory brainstem response testing, which subsequently reveals absent hearing in both ears. A careful family history is negative for any individuals who have deafness. The parents ask you what could have caused deafness in their baby. Of the following, the likelihood that this infant has a genetic cause for deafness is CLOSEST to 1. 2. 3. 4. 5. <1% 5% 25% 50% 75% Question 5 Answer D The incidence of prelingual, moderate-to-profound sensorineural hearing loss (=40 dB) is 1 in 500 in developed countries, making it the most common birth defect in these regions. Approximately 1 in 1,000 newborns is deaf (hearing loss in the severe-to-profound range of 71 to 90 dB). Fifty percent of all prelingual, moderate-to-profound hearing loss is genetic, 25% is nongenetic (eg, having bacterial and viral causes), and 25% is idiopathic (Item C183). Of the genetic forms of deafness, 30% are syndromic, and 70% are nonsyndromic. Syndromic causes of deafness include conditions such as Usher, Waardenburg, and Treacher-Collins syndromes. Nonsyndromic causes can be autosomal recessive (75% to 85%), autosomal dominant (15 % to 24%), and X-linked (1% to 2%). A critical aspect of the evaluation of any child who has prelingual hearing loss is defining the type of loss as clearly as possible. Careful audiologic evaluation should be undertaken in concert with examination by an otolaryngologist. Affected individuals should undergo computed tomography scan of the temporal bones to look for malformations of the inner ear. The information gleaned from these studies helps to guide the evaluation because different gene mutations are associated with different clinical manifestations. It is important to obtain a careful, three-generation pedigree, with attention to any individuals who have hearing loss, vision loss, dysmorphic features, early death, birth defects, and intellectual disabilities. Referral to a geneticist is important to determine if there is a recognizable pattern of features or any genetic testing that could be helpful. The gene loci for nonsyndromic deafness are designated "DFN" (for DeaFNess). The loci are categorized as DFNA (autosomal dominant), DFNB (autosomal recessive), and DFN (X-linked). Some genes can be involved in both dominant and recessive forms of deafness, depending on the specific mutation(s), and some mutations cause both sensorineural and conductive hearing loss. Although there are exceptions, most autosomal dominant loci cause postlingual hearing impairment, and most autosomal recessive loci cause severe-to-profound prelingual deafness. X-linked (DFN) loci are associated with both pre- and postlingual hearing loss. Because the many molecular genetic testing options can be somewhat confusing, consultation with a clinical geneticist is strongly recommended. Numerous laboratories offer panels of common mutations. In many populations worldwide, approximately 50% of individuals who have prelingual, autosomal recessive nonsyndromic hearing loss have GJB2 mutations; the remainder may have a mutation in any number of genes that may have been described as causing deafness in only one or two families. American Board of Pediatrics Content Specification: Know the common causes of congenital deafness Item C183 • A 9-year-old boy comes to your office for a health supervision visit. He has difficulty seeing large print and recently began learning Braille in school. As an infant, he had severe retinopathy of prematurity, and he has had long-standing difficulty seeing, even with corrective lenses. His parents have been told that their son is considered legally blind. They ask what this designation means. Of the following, the BEST response is that legal blindness means 1. 2. 3. 4. 5. ability to detect only the direction of a light source corrected vision of 20/70 or worse in the best eye corrected vision of 20/200 or worse in the best eye no residual visual function in either eye uncorrected vision of 20/100 or worse in the best eye Answer C • The child described in the vignette is legally blind, defined as a corrected vision of 20/200 or worse in the best eye. Approximately 75% of legally blind individuals have some residual visual ability. Students may be classified as educationally visually impaired if their corrected vision is 20/70 or worse in the best eye. Children who have visual impairment need to learn in specialized environments to motivate them to move and improve their abilities to interpret sensory information accurately. Young infants should be encouraged to be mobile and orient themselves to the environment using touch, smell, and auditory input. Beginning in preschool, the goal is to teach skills that promote independence in the performance of daily activities. Depending on the degree of any associated impairments, the child may attend a regular school program with input from a teacher of the visually handicapped. The educational program should emphasize sensory experiences and auditory programs. The school-age child should have an Individualized Educational Plan. Again, depending on any associated impairments, the child may participate in regular community-based classroom activities, focusing on reading, writing, travel needs, and eventually vocational training and independent living. Braille is used for nonvisual communication and audio recordings supplement reading. American Board of Pediatrics Content Specification(s): Know the major approaches to the education of visually impaired children • A 2-year-old boy is mildly delayed in reaching his gross motor milestones, but his language development is appropriate for his age. He can speak in three- to four-word sentences. His parents are concerned that he will have academic difficulties due to his motor deficiencies. His neurologic examination yields nonfocal results. Of the following, the MOST appropriate response is that 1. 2. 3. 4. 5. gross motor development is an accurate predictor for school success his delays are associated with learning disabilities his delays will result in poor handwriting skills his mildly delayed gross motor skills suggest a diagnosis of cerebral palsy language development is an accurate predictor of intellectual function Answer E • A child's language development in infancy and early childhood correlates closely with cognitive development and, thus, is a better predictor of cognitive function than gross motor development. The acquisition and use of language is critical to a child's development in the areas of cognitive and social development. Phonemic awareness is the ability to attend to phonemes (speech sounds) that are used in syllables and words and is a critical language skill in the development of reading. The delay in achieving gross motor milestones described for the boy in the vignette has the weakest correlation with general intellectual functioning and, therefore, is not a strong predictor of school success. He has mildly delayed gross motor skills and a nonfocal neurologic examination. As a result, he does not meet the criteria for a diagnosis of cerebral palsy. Handwriting skills are affected by weakness in fine (not gross) motor development. American Board of Pediatrics Content Specification(s): Understand that language development in infancy and early childhood is a better predictor of cognitive function than motor development • Results of a cognitive test given to a 7-year-old girl indicate functioning in the moderate intellectual disabilities range (intelligence quotient between 40 and 50). Her parents ask what the future holds for their child academically and vocationally. Of the following, the MOST likely expectation is that the child 1. 2. 3. 4. 5. can achieve a third- to sixth-grade reading level by adolescence can be employed in a competitive unskilled or semiskilled job can work in a sheltered workshop that provides close supervision will only be able to learn to read simple signs such as stop and exit will require help with activities of daily living from caregivers when an adult Answer C • The American Association on Intellectual and Developmental Disabilities (AAIDD) defines intellectual disability (ID) as a disability "characterized by significant limitations both in intellectual function and in adaptive behavior as expressed in conceptual, social, and practical adaptive skill. This disability originates before the age of 18." Children who have mild ID (IQ, 50-55 to 70) and no comorbid disorders are selfsufficient in activities of daily living (ADL) and communication. They can be expected to learn at one half to two thirds normal velocity. They can reach a third- to sixthgrade reading level by late adolescence and can be expected to be employed in competitive unskilled, semiskilled, or in some cases, skilled jobs. The prevalence rate of mild ID is 20 to 30 per 1,000, and affected children often are identified in kindergarten and early elementary school. Individuals who have moderate ID (IQ, 35-40 to 50-55), such as the girl described in the vignette, are able to do ADL and express basic needs. They learn at one third to one half velocity. They can be expected to achieve a first- to third-grade reading level. They may be able to function in a supportive employment setting, but more often they work in sheltered workshops that provide constant supervision. In adulthood, they often live in group homes. The prevalence rate of moderate ID is 5 per 1,000, and the condition most often is identified in preschool. • Children who have severe ID (IQ, 20-25 to 35-40) have limited language skills and need support with ADL. They might be able to learn to read simple signs such as stop and exit. They will continue to need help with ADL from caregivers as adults. The prevalence rate of severe ID is 3 per 1,000, and affected children are identified before age 3 years. These individuals often have identified genetic, medical, and neurologic causes. Children who have profound ID (IQ, <20-25) require assistance for ADL. They have the highest rates of identified genetic, medical, and neurologic causes. The prevalence rate of profound ID is 1 to 2 per 1,000, and affected children are identified prior to age 2 years. American Board of Pediatrics Content Specification(s): Distinguish between mild and moderate intellectual disabilities with regard to the potential for educational and independence/vocational achievement During a health supervision visit, a mother reports that her child is only understood about 75% of the time when she speaks to other adults. Of the following, this finding is MOST expected for a typically developing child who is 1. 2. 3. 4. 5. 18 months old 24 months old 30 months old 36 months old 48 months old Answer D • A helpful rule regarding the development of articulation is the Rule of Fourths. The average 2-year-old child should be understood by strangers half the time (2/4), the average 3-year-old child should be understood ¾ of the time, and the average 4year-old should be understood all the time (4/4). The girl in the vignette is described as being understood by a stranger 75% of the time, which is typical for a child of 3 years. Children may have difficulty with the pronunciation of certain sounds until they are 7 years of age, but 100% of speech should be understood by age 4 years. In normal speech development, the first eight consonant sounds that develop are m, b, y, n, w, d, p, and h. The last eight consonants are sh, th (as in thirty), s, z, th (as in the), zh sound typically spelled as s (as in pleasure), l, and r, which develop by age 7. American Board of Pediatrics Content Specification(s): Know the progression of speech intelligibility and that deviation from the progression is abnormal (eg, 0% of intelligibility to strangers is 2/4 at 2 years, ¾ at 3 years, 4/4 at 4 years) • • A 7-year-old boy has mild intellectual impairment and an autism spectrum disorder. He has a pleasant disposition and no aggressive behaviors, but he has trouble paying attention in the classroom and difficulty staying in his seat. Both teacher report and parent rating forms document highly significant hyperactivity and difficulty paying attention. His parents are concerned that his activity level is affecting his ability to learn. They ask if any medication can help him attain school success. Of the following, the MOST appropriate response is to 1. 2. 3. 4. 5. begin an atypical antipsychotic begin a trial of a serotonin reuptake inhibitor begin a trial of stimulant medication explain that medication would be ineffective due to his intellectual disability reassure the family that he is doing his best and have them return in 6 months Answer C • The child described in the vignette has an autism spectrum disorder, symptoms of hyperactivity, and a short attention span. According to his teacher and parents, these symptoms are affecting his ability to learn at school. Therefore, a trial of a stimulant medication is indicated to target the symptoms. Stimulants can be effective, even in individuals who have intellectual disabilities. In 2005, the Research Units on Pediatric Psychopharmacology Autism Network studied methylphenidate in the treatment of children who had autism spectrum disorders. The results indicated drug efficacy, but with reduced effectiveness and a less satisfactory adverse effect profile. The most reported adverse effect was decreased appetite. The boy is having significant difficulty, and simply reassuring the family will not help his functioning at school. An atypical antipsychotic is not indicated in this situation because the child is not exhibiting aggressive or self-injurious behaviors, irritability, or explosive outbursts. Serotonin reuptake inhibitors are indicated for the treatment of obsessive-compulsive behaviors, anxiety, or symptoms of low mood, symptoms not exhibited by the boy in the vignette. American Board of Pediatrics Content Specification(s): Understand that children with intellectual disabilities and/or autism spectrum disorder who have symptoms of hyperactivity and short attention span may respond to medication • A 13-year-old boy who has an autism spectrum disorder is displaying severely aggressive behavior to his parents and teachers. When frustrated, he has tantrums, and when upset, he hits himself and throws objects. This behavior has continued even after intensive behavioral and educational interventions. His parents wish to begin medication to help handle him safely at home. Of the following, the MOST appropriate medication with which to begin a trial is 1. 2. 3. 4. 5. atypical antipsychotic lithium melatonin serotonin reuptake inhibitor stimulant medication Answer A • The significant behaviors exhibited by the boy described in the vignette include explosive outbursts, aggression, and self-injurious behaviors. Behavioral and educational approaches are the starting point for intervention. Because the child's behavior places him at risk for harming himself or others, pharmacologic therapy should be initiated. Medications that target irritability, aggression, explosive outbursts, and self-injurious behaviors include atypical antipsychotics and anticonvulsant mood stabilizers. An atypical antipsychotic is an appropriate choice for this boy. The most common adverse effects noted with these medications are weight gain, increase in appetite, and fatigue. Anticonvulsant mood stabilizers also may be used to treat target behaviors as well as bipolar symptoms and repetitive behaviors. Alpha-2 agonists such as long-acting guanfacine may be used to target attention-deficit/hyperactivity disorder (ADHD) symptoms, aggression, and sleep dysfunction. Stimulant medications and selective norepinephrine reuptake inhibitors are used for ADHD symptoms of hyperactivity, impulsivity, inattention, and distractibility. They are not used to target primarily aggressive behaviors or self-injurious behaviors. Lithium is used for bipolar disorder and has a low therapeutic-to-toxic ratio. Selective serotonin reuptake inhibitors are used to treat repetitive behaviors, anxiety, and depressive symptoms. Many selective serotonin reuptake inhibitors are used offlabel. Melatonin is a naturally occurring hormone that is not regulated by the United States Food and Drug Administration, but it is available over the counter in the United States. Several studies have indicated its usefulness in promoting sleep but not for aggression or self-injurious behaviors. American Board of Pediatrics Content Specification(s): Know the role of medications in the autism spectrum disorders • You are seeing a 3-year-old boy for a health supervision visit. He has a vocabulary of 50 words that he says clearly, and he is just beginning to combine words. He follows simple two-step commands. Past medical history reveals that he was born at term and had no perinatal problems. He has no history of recurrent ear infections and achieved gross motor milestones at appropriate ages. He resides in a bilingual household. According to the family history, his father also experienced delayed speech development. His older brother received speech therapy in elementary school, and his older sister had difficulty with reading comprehension but does well in math. Of the following, the MOST likely cause of this boy's language delay is 1. 2. 3. 4. 5. a bilingual household being third born genetic predisposition hearing loss his sex Answer C • The most likely cause for the delay in language development described for the boy in the vignette is genetic, based on the strong family history of language delays and reading difficulty. Children who have specific language impairment or a reading disorder often have family histories that suggest a genetic basis for the problems. The rate of reading disorder in parents of affected children ranges from 25% to 60%. A child who has a family history of both protracted language problems and learning issues has greater risk for language-based learning difficulties. A language delay of greater than 25% (calculated as a language level of below 27 months in a 36-month-old child) should be evaluated and not disregarded because the child is a boy, second or third born in a family, or part of a household in which more than one language is spoken. Language development in boys averages only a 1- to 2-month lag behind girls. Current research suggests that monolingual and bilingual children meet major language developmental milestones at similar times. A child raised in a bilingual home may use the two languages during a conversation, which has been found to be a sign of mastery of both languages. The child's total vocabulary size and length of utterance (number of words in a sentence) should be normal by age 2 to 3 years. • • Other causes of delayed language development include genetic and chromosomal disorders as well as neurologic disorders such as cerebral palsy. An autism spectrum disorder should be suspected when language is both deviant and delayed. Global developmental delay may be suspected if delays in motor or cognitive development also are apparent. Universal screening of newborns detects most infants who have moderate, severe, or profound sensorineural hearing loss, although such screening may miss individuals who have mild-to-moderate, progressive, or acquired hearing loss. Hearing loss is a particular concern if the child has difficulty saying or hearing the sounds s, th, and f (high-frequency sounds). American Board of Pediatrics Content Specification(s): Know the causes of delayed language development Understand the importance of family history in the diagnosis of language disorders • An 8-year-old boy has an above-average intelligence quotient, but he is struggling in school and consistently brings home failing grades. He is generally well behaved, but he gets angry with the poor grades. He enjoys being with his friends and is active in afterschool activities. Of the following, the MOST appropriate intervention is to 1. 2. 3. 4. 5. have the parents set up a behavioral chart to encourage him to improve his grades reassure the parents that he is smart and schedule a follow-up appointment in 6 months refer him for psychoeducational evaluation refer him to a psychiatrist tell the parents to punish him if he continues to fail Answer C • The boy described in the vignette has above-average intelligence but is having academic difficulties, warranting psychoeducational evaluation for a learning disability. The reported prevalence of dyslexia (specific reading disability) ranges from 5% to 17% in the general population. The rate of dyscalculia (specific learning disability in mathematics) is 4% to 6%. Individuals may have learning difficulties that occur independent of intelligence. Frequently, individuals who have high intelligence are not identified as having a learning issue or are considered to lack motivation. Such children who have above-average intelligence may have uneven profiles when evaluating their cognitive, social, and emotional development. The boy in the vignette should not be expected to improve spontaneously. The academic difficulty is not within his control and would not be remediated via discipline or use of a behavior chart. He is not showing evidence of a primary mood disorder for which a referral to a psychiatrist would be indicated. Additional causes of school failure are attention-deficit/hyperactivity disorder, sensory deficits (eg, diminished visual or auditory acuity), disordered sleep, or epilepsy. An older child should be evaluated for use of illicit drugs or alcohol. American Board of Pediatrics Content Specification(s): Recognize that children with above average intelligence may have academic failure and learning disabilities • A mother is concerned that her 6-year-old boy has been struggling to learn his alphabet and numbers in kindergarten. He is in good health, and results of his vision and hearing screens are normal. His preschool teacher commented last year that he was a bit shy but enjoyed being with the other children. Of the following, the MOST appropriate next step is to 1. 2. 3. 4. 5. evaluate the boy for attention-deficit/hyperactivity disorder reassure the parents and schedule a 6-month follow-up appointment refer the boy for behavioral counseling refer the boy for psychoeducational evaluation refer the boy for vision therapy Answer D • Approximately 5% to 17.5% of individuals in the United States have learning disabilities (depending on the definition used). Dyslexia (reading disability) is seen in approximately 80% of individuals who have learning disabilities. Children in preschool may present with delays in speech and language and may have difficulty following directions and classroom routine. The boy described in the vignette may have a learning disability, suggested by the difficulty he is having in learning the alphabet or numbers in kindergarten. Other indicators of learning disabilities are difficulty paying attention, learning new skills, and connecting letters to sounds. There also may be poor coordination, including difficulty pasting, coloring, and writing. Therefore, reassurance of the parents is not appropriate. The boy requires a formal psychoeducational evaluation that includes cognitive and academic assessment. The evaluation should be performed in a timely manner so that his learning difficulty does not lead to frustration and poor self-image. If the evaluation identifies issues with attention or self-esteem, behavioral counseling and further assessment for attentiondeficit/hyperactivity disorder should be pursued. Currently, no scientific evidence supports the position that subtle eye or visual problems cause learning disabilities or that vision therapy improves academic achievement. Other than convergence-insufficiency treatment, therapy to improve visual function is not supported and is poorly validated. Convergence insufficiency occurs when an individual is focusing at a near object and the eyes do not turn in properly. Treating this disorder with eye-focusing exercise can make reading more comfortable, but it does not improve decoding or comprehension of reading. American Board of Pediatrics Content Specification(s): Identify the indicators of learning difficulties (eg, preschool delay in speech and language, failure to learn letters and numbers by the end of kindergarten, failure to learn to read simple words by the end of first grade) • A 10-year-old boy has been receiving specialized educational services in school due to a learning disability. His parents encourage after-school or sports activities to promote positive self-esteem. They realize that academics are a challenge for him, and they express concerns about his future as an adult. Of the following, the factor that has been shown to have the MOST positive effect on prognosis for such a child is 1. 2. 3. 4. 5. early intervention therapy father's level of education having two or more siblings high intelligence quotient strong family support Answer E • The presence of strong family support has been shown to have a positive effect on the prognoses of children who have learning disabilities, such as the boy described in the vignette. This effect is greater than that associated with the parent's education, number of siblings in the family, intelligence quotient score, or early educational intervention. Parent involvement and collaboration with physicians and schools is critical to ensure appropriate services. Support in the home via interactive learning activities (use of readers, audiobooks) is especially important for children who have learning disabilities because they often are overwhelmed, disorganized, and frustrated in learning situations. Specific academic support such as one-on-one tutoring in the home frequently is sought to help focus on homework. Family support can augment specialized educational intervention. Educational strategies such as remediation work targeting the underlying cognitive function that is impaired and phonologic programs (those that improve word decoding) have shown efficacy up to the sixth grade. If the area of weakness is unlikely to be corrected, circumvention strategies are useful in improving the outcome. Such strategies include using a keyboard or verbal exams for a child who has motor dysgraphia, using audiobooks for a child who has dyslexia, and using a calculator for the child who has dyscalculia (math disorder). American Board of Pediatrics Content Specification(s): Recognize factors that affect prognosis in a learning-disabled child