* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 10_Infertility
Embryo transfer wikipedia , lookup
Donor Sibling Registry wikipedia , lookup
Progesterone (medication) wikipedia , lookup
Egg donation wikipedia , lookup
In vitro fertilisation wikipedia , lookup
Semen quality wikipedia , lookup
Artificial insemination wikipedia , lookup
Infertility wikipedia , lookup
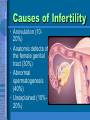
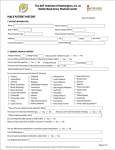
Infertility By as. Stelmakh O. Objectives • Define primary and secondary infertility • Describe the causes of infertility • Diagnosis and management of infertility Infertility - Statistics • causes are identified in 90 % of patients • pregnancy results in 40 % of those • 30 % of couples have male AND female factors • Of 100 subfertile couples the break down is as follows: • 40 % male factor etiology • 20 % female hormonal imbalance • 30 % female peritoneal factor • 5 % ‘hostile’ cervical environment • 5 % unexplained • psychological impact can be significant Infertility • Primary infertility – a couple that has never conceived • Secondary infertility – infertility that occurs after previous pregnancy regardless of outcome Causes for infertility • Male – – – – – – Drugs Tobacco Health problems Radiation/Chemotherapy Age Enviromental factors • Pesticides • Lead • Female – Age – Stress – Poor diet – Athletic training – Over/underweight – Tobacco – STD’s – Health problems Causes of Infertility • Anovulation (1020%) • Anatomic defects of the female genital tract (30%) • Abnormal spermatogenesis (40%) • Unexplained (10%20%) Evaluation of the Infertile couple • • • • History and Physical exam Semen analysis Thyroid and prolactin evaluation Determination of ovulation – Basal body temperature record – Serum progesterone – Ovarian reserve testing • Hysterosalpingogram Abnormalities of Spermatogenesis Normal • Sperm made in seminiferous tubules • Travel to epididymis to mature Normal • Sperm exit through vas deferens • Semen produced in prostate gland, seminal glands, cowpers glands • Sperm only 5% of ejaculation • Sperm can live 5-7 days Semen Analysis (SA) • Obtained by masturbation • Provides immediate information – – – – – • • • • Quantity Quality Density of the sperm Morphology Motility Abstain from coitus 2 to 3 days Collect all the ejaculate Analyze within 1 hour A normal semen analysis excludes male factor 90% of the time Normal Values for SA Volume Sperm Concentration Motility Viscosity Morphology pH WBC – 2.0 ml or more – 20 million/ml or more – 50% forward progression 25% rapid progression – Liquification in 30-60 min – 30% or more normal forms – 7.2-7.8 – Fewer than 1 million/ml Causes for male infertility • 42% varicocele – repair if there is a low count or decreased motility • 22% idiopathic • 14% obstruction • 20% other (genetic abnormalities) Abnormal Semen Analysis • Azoospermia – Klinefelter’s (1 in 500) – Hypogonadotropichypogonadism – Ductal obstruction (absence of the Vas deferens) • Oligospermia – – – – Anatomic defects Endocrinopathies Genetic factors Exogenous (e.g. heat) • Abnormal volume – Retrograde ejaculation – Infection – Ejaculatory failure Evaluation of Ovulation Female Reproductive System • Ovaries – Two organs that produce eggs – Size of almond – 30,000-40,000 eggs – Eggs can live for 12-24 hours Menstruation • Ovulation occurs 13-14 times per year • Menstrual cycles on average are Q 28 days with ovulation around day 14 • Luteal phase – dominated by the secretion of progesterone – released by the corpus luteum • Progesterone causes – Thickening of the endocervical mucus – Increases the basal body temperature (0.6° F) • Involution of the corpus luteum causes a fall in progesterone and the onset of menses Menstrual cycle Serum Progesterone • Progesterone starts rising with the LH surge – drawn between day 21-24 • Mid-luteal phase – >10 ng/ml suggests ovulation Salivary Estrogen: Ovulation Tester- 92% accurate Add Saliva Sample Non-Ovulatory Saliva Pattern High Estrogen/ Ovulatory Saliva Pattern Anovulation Anovulation Symptoms Evaluation* • Irregular menstrual cycles • Amenorrhea • Hirsuitism • Acne • Galactorrhea • Increased vaginal secretions • Follicle stimulating hormone • Lutenizing hormone • Thyroid stimulating hormone • Prolactin • Androstenedione • Total testosterone *Order the appropriate tests based on the clinical indications Fertilization Implantation Anatomic Disorders of the Female Genital Tract Congenital Anatomic Abnormalities Hysterosalpingogram • An X-ray that evaluates the internal female genital tract – architecture and integrity of the system • Performed between the 7th and 11th day of the cycle • Diagnostic accuracy of 70% Hysterosalpingogram • The endometrial cavity – Smooth – Symmetrical • Fallopian tubes – Proximal 2/3 slender – Ampulla is dilated • Dye should spill promptly HSG: Tubal Infertility Some women have trouble getting pregnant because scar tissue prevents eggs from traveling down the fallopian tubes. This scarring can be caused by endometriosis, the overgrowth of tissue that lines the uterus, a history of pelvic infections, or previous surgeries Treatment of the Infertile Couple Inadequate Spermatogenesis • Laparoscopy surgery • Eliminate alterations of thermoregulation • Clomiphene citrate is occasionally used for induction of spermatogenesis – 20% success • In vitro fertilization may facilitate fertilization • Artificial insemination with donor sperm is often successful Intrauterine insemination (artificial insemination) Artificial Insemination • Sperm donation or sperm aspiration In Vitro Fertilization IVF Protocol • GnRH agonist (e.g. Lupron) for 7 days • FSH agonist (follistim, Gonal-F, Repronex) until follicles measure 17-20 mm in diameter • hCG given to induce egg maturation • Egg retrieval (transvaginally) 34-35 h later IVF Protocol, cont’d. • 3 to 5 embryos are injected to increase chances of pregnancy • woman given progestagen to prevent miscarriage Surrogate mother – Woman unable to have children may have IVF in another woman who has the child IVF With Donor Eggs Women who are over 40, have poor egg quality, or have not had success with previous IVF cycles may consider IVF with donor eggs Primary Diagnosis of Women Undergoing ART- 1998 12% 15% 9% 2% 27% 9% 26% Tubal factor Male factor Ovulation dysfxn Endometriosis Unexplained Uterine factor Other Conclusion • Infertility should be evaluated after one year of unprotected intercourse. • History and Physical examination usually will help to identify the etiology. • If patients fail the initial therapies then the proper referral should be made to a reproductive specialist.