* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Dental Emergencies - Calgary Emergency Medicine
Special needs dentistry wikipedia , lookup
Auditory system wikipedia , lookup
Dental implant wikipedia , lookup
Dental degree wikipedia , lookup
Remineralisation of teeth wikipedia , lookup
Focal infection theory wikipedia , lookup
Tooth whitening wikipedia , lookup
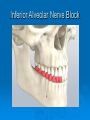
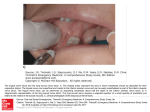
Dental Emergencies Scott Farquharson Sept 24th 2009 Topics Covered Dental trauma Dental infections Dental blocks Pediatrics Dental Anatomy Primary Eruption from 7-30 months 20 teeth, 10 upper, 10 lower 2X ( 4 incisors, 2 canines, 4 molars) Permanent Begin formation 3-4 months Eruption 7-21 years 32 teeth ( including wisdom teeth) 2x ( 4 incisors, 2 canines, 4 premolars, 6 molars) Dental Anatomy Dental Trauma Fractures of teeth Alveolar Fractures Luxation Intrusion or concussion Avulsion Primary vs Permanent Fractures of Permanent Teeth Enamel (Ellis 1) Chipped tooth Painless unless associated with other injuries Large chips can be saved for reattachment Non urgent dental referral for cosmetic purposes Fractures of Permanent Teeth Enamel and Dentin ( Ellis 2) 70 % of dental fractures Pain with hot or cold Dentin is yellow colored Panorex to R/O other injury Increased risk of pulp infection/desiccation Dental evaluation in 24hrs Protection with dental cement Consider antibiotics Fractures of Permanent Teeth Pulp involvement May be visible (Ellis 3) • Can see blood May be below gums (root fracture) • Only seen with x-ray Very painful as nerve exposed Treatment as Ellis 2 Will need extraction or root canal Fractures of Permanent Teeth Alveolar Fractures Associated with fractures, luxated or avulsed teeth small fractures involving 1 or 2 teeth can be treated by a dentist Large areas of alveolar bone damage can cause significant cosmetic deformity and oral surgery should be consulted Root Fracture Luxation “Loose tooth” Extrusion – dislodgement from alveolar bone Lateral luxation – lateral displacement with alveolar fracture Both should have x-rays Reposition with firm pressure – may require local anesthesia Temporary splinting in ED Permanent splinting/treatment by dentist Concussion and Intrusion Displacement of tooth into socket Concussion – pain with no movement Intrusion – more severe displacement involving root fracture and/or alveolar fracture Intrusion is differentiated on x-ray and requires repositioning Avulsion Complete displacement of tooth from alveolar socket Best chance of saving tooth if reimplanted in under 3 hrs Transport in sterile saline, milk, Hank solution or in buccal sulcus not ice or water Avoid disruption of periodontal ligament fibers on root Clean with normal saline Rinse clot from socket splint Primary Vs Permanent Avulsed primary teeth should not be reimplanted to avoid damage to underlying teeth Primary teeth have more pulp and less dentin and are more at risk for infection Luxations in young children are at greater risk of avulsion and aspiration – consider urgent dental splinting. Enamel injuries can cut mucosa in young children and may need to be filed down Final Thoughts Pen or amoxicillin usually sufficient Consider clindamycin or EES if allergic Don’t forget tetanus immunization Dental Infections Periapical abscess Pericoronitis Dry socket Buccal/facial cellulitis Complications Periapical Abscess Complication of carries/pulpitis Inflammation and abscess formation in periodontal and buccal tissues lymphadenopathy Streptococcus mutans Painful – relieved by I&D Definitive treatment is root canal (removal of the pulp and filling of the empty pulp chamber and canal ) Periapical Abscess Periapical Abscess Pericoronitis Most common in wisdom teeth bacterial plaque and food debris accumulate beneath the flap of gum covering the partially erupted tooth. Pain, bad taste, pus, local inflammation can progress to cellulitis Salt mouthwashes, irrigate under flap ABX Pericoronitis Dry Socket- Alveolar Osteitis Complication of tooth extraction Clot covering alveolar bone is displaced Exposed alveolar bone becomes inflamed Normal post extraction pain decreases over 48hrs Dry socket pain increases at 24-72 hrs Can progress to osteomyelitis Dry Socket Analgesia – Nsaids, Narcotics, Nerve block Referral back to dentist in 24 hrs Will need frequent packing ABX? If caught early and timely follow up is available probably not needed Complications Dental infections can progress to life threatening complications Facial or buccal cellulitis Submandibular space infections (Ludwig’s angina) Parapharyngeal space infections Airway compromise Orbital infections CNS infections Mediastinal infections Cavernous sinus thrombosis Complications Signs of more serious illness Systemic symptoms – fever/chills Trismus Displacement of tongue Altered LOC/delirium Eye pain Require systemic ABX ENT consult Possible CT imaging Airway management Antibiotics Broad range of pathogens Simple infections Mainly streptoccocal Bacteroides sp. Anaerobes Pen V or amoxil I prefer Amox/Clav or clinda Infections extending to facial or buccal cellulitis IV 2nd generation cephalosporin + metronidazole HPTP Dental Nerve Blocks Supraperiosteal Anesthesia for individual tooth Inferior Alveolar nerve block Nerve Block Anesthesia for lower teeth Supraperiosteal Nerve Block Select the area to be anesthetized and dry it with gauze. Ask the patient to close the jaw slightly to relax the facial musculature. Grasp the mucous membrane of the area with a piece of gauze. Pull the gauze (and the mucous membrane) out and downward in the maxilla and out and upward in the mandible to extend the mucosa fully and to delineate the mucobuccal fold. Puncture the mucobuccal fold with the bevel of the needle facing the bone. Aspirate the area and then deposit approximately 1 to 2 mL of local anesthetic at the apex (area of the root tip) of the involved tooth. It is helpful to place a finger against the outer aspect of the lip overlying the injection site and apply firm and steady pressure against the lip while slowly injecting the local anesthetic into the supraperiosteal site Supraperiosteal Nerve Block Supraperiosteal Nerve Block Inferior Alveolar Nerve Block Inferior Alveolar Nerve Block Palpate the retromolar fossa with the index finger or thumb. Identify the greatest depth of the anterior border of the ramus of the mandible (the coronoid notch). With the thumb in the mouth and the index finger placed externally behind the ramus, retract the tissues toward the buccal (cheek) side, and visualize the pterygomandibular triangle. This technique also moves the operator’s finger safely away from the tip of the needle. Inferior Alveolar Nerve Block Inferior Alveolar Nerve Block Hold the syringe parallel to the occlusal surfaces of the teeth and angled so that the barrel of the syringe lies between the first and second premolars on the opposite side of the mandible. Achieving the proper angle is important to the success of this block. If a large-barrel syringe is used, the corner of the mouth may hamper efforts to obtain the proper angle. Carefully bend the 25-gauge needle about 30 degrees to facilitate achieving the proper angle. The needle cap can be used to bend the needle Inferior Alveolar Nerve Block Make the puncture for the injection in the pterygomandibular triangle, at a point that is 1 cm above the occlusal surface of the molars. If the needle enters too low (e.g., at the level of the teeth), the anesthetic will be deposited over the bony canal and prominence (lingula) that house the mandibular nerve, and not over the nerve itself. There may be slight resistance as the needle passes through the ligaments and the muscles covering the internal surface of the mandible. When there is more solid resistance, the needle has reached the bone. Stop when the needle has reached bone, which signifies contact with the posterior wall of the mandibular sulcus. It is important to feel the bone with the needle ( Inferior Alveolar Nerve Block Inferior Alveolar Nerve Block It is important to feel the bone with the needle. After reaching the bone, withdraw the needle slightly and aspirate to check for possible intravascular placement. Deposit approximately 1 to 2 mL of anesthetic solution; 3 to 4 mL of anesthetic may be required if needle positioning is suboptimal. Inferior Alveolar Nerve Block Inferior Alveolar Nerve Block Failure to feel bone as the needle is advanced generally results from directing the needle toward the parotid gland (too far posteriorly) rather than toward the inner aspect of the mandible. Injecting into the parotid gland can anesthetize the facial nerve Inferior Alveolar Nerve Block One may anesthetize the lingual nerve by placing several drops of anesthetic solution while withdrawing the syringe. The anterior two thirds of the tongue can thus be anesthetized. In actual practice, the lingual nerve is consistently blocked with this procedure owing to the close proximity of both nerves. Inferior Alveolar Nerve Block Complications include inadvertent administration of anesthetic posteriorly in the region of the parotid gland, which will anesthetize the facial nerves. This is an annoying but relatively benign complication that will cause temporary facial paralysis (similar to Bell’s palsy) affecting the orbicularis oculi muscle and results in inability to close the eyelid. Should this occur, the eye must be protected until the local anesthetic has worn off (approximately 2 to 3 hours), and the patient must be reassured. Anesthesia with bupivacaine (Marcaine) presents a more significant problem if this complication occurs, because bupivacaine anesthesia lasts from 10 to 18 hours in some patients.