* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Rheumatologic Emergencies - Calgary Emergency Medicine
Survey
Document related concepts
Hospital-acquired infection wikipedia , lookup
Globalization and disease wikipedia , lookup
Germ theory of disease wikipedia , lookup
Osteochondritis dissecans wikipedia , lookup
Kawasaki disease wikipedia , lookup
IgA nephropathy wikipedia , lookup
Multiple sclerosis research wikipedia , lookup
Multiple sclerosis signs and symptoms wikipedia , lookup
Behçet's disease wikipedia , lookup
Schistosomiasis wikipedia , lookup
Sjögren syndrome wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Tennis elbow wikipedia , lookup
Ankylosing spondylitis wikipedia , lookup
Transcript
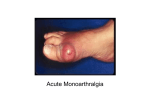
Rheumatologic Emergencies Sarah McPherson May1, 2002 MONOARTICULAR ARTHRITIS Case: 70 year old man presents with a red hot swollen knee x 24 hr. He tells you that the affected knee is a prosthetic joint. What is the likely diagnosis? How should you manage this case? Septic Arthritis Common joints involved: Adult: Knee, wrist, ankle Children: Knee, Hip IVDU: axial skeleton (vertebral, SI, sternoclav) Risk Factors: Very old and young Chronic debilitating disease IVDU Immunosuppressive therapy Prosthetic joint or post arthrocentesis Septic Arthritis Joint aspiration: A must do!!!! KNEE: Extend knee, insert needle from the medial side between posterior surface of the patella and intercondylar femoral notch at midpoint to superior pole of the patella WRIST: Flex wrist with ulnar deviation. Insert needle distal to Lister’s tubercle ulnar to extensor pollicus longus Septic Arthritis ELBOW Flex elbow . Insert needle from lateral side distal to lateral epicondyle and direct medially ANKLE Plantar flex foot. Insert needle into hollow at anterior edge of the medial malleolus medial to anterior tibial tendon. Will have to insert needle 2-3 cm NORMAL SYNOVIAL FLUID ANALYSIS Clear < 200 WBC/mm3 < 25 PMN no crystals Septic Arthritis Management: Non-prosthetic joint: Daily aspiration Iv Ancef for 3 weeks Prosthetic joint Daily aspiration or I&D IV vancomycin and po Ciprofloxacin Gout Risk factors: Obesity Hypertension Diabetes Alcohol consumption Loop diuretics Lead exposure Gout Management: NSAIDs: Indomethacin 50 mg tid X 3-5 days Colchicine: 0.6 mg q1h until pain subsides max 4-6 mg Side Effects: GI upset, Steroids If resistant to above; 40 mg qd X 3-5 days POLYARTHRITIS Case: 26 yr old woman presents with myalgias and arthritis of the right wrist and left knee X 1 wk. She notes that 2 days ago she also had pain in her left hand but that had resolved. On exam she is febrile and you notice red pustular lesions on the sides of her fingers. Gonnococcal Arthritis Fever, chills, arthralgia progressing to arthritis Wrist, knee, and ankle most commonly affected 2/3 will have characteristic rash (necrotic pustules on distal extremities & fingers) Gonococcal Arthritis Diagnosis: initially clinical diagnosis Confirm with C&S from urethral, rectal and pharyngeal swabs Treatment: Ceftriaxone 1 gr iv X 24-48 hr Follow with Cefixime 400mg bid or Cipro 500mg bid to complete 7 days antibx Case: 65 yr old man presents with a headache and achy joints for just over 24 hrs. He describes a red lesion on his thigh that has been growing in size for the past 3 days. Lyme disease From tick bites in areas where Borrelia burdorferi is endemic ~ 50% of people remember bite Presentation: Lesion at bite site that rapidly grows in size and multiplies Red boarder with central clearing Fever, migratory tenosynovitis, polyarthrits, headache At 4 weeks may have neurologic and cardiac abnormalities 50-60% arthritis at 6 months, may be recurrent Lyme disease Treatment: Shortens duration of symptoms and prevents later disease Doxycycline 100mg bid X 2-4 weeks Amoxicillin 500mg tid X 2-4 weeks (pregnant and lactating women, children < 5 yrs) Reiter’s Syndrome Reactive arthritis from GI/GU infections (Chlamydia, Shigella, Salmonella, Yersinia, Campylobacter) Asymmetric polyarthritis mainly of weight bearing joints ~ 2-6 weeks post urethritis or dysentery Reiter’s Syndrome Physical exam: Polyarthritis Ocular findings (conjuntivitis, uveitis, corneal ulcers) Oral ulcers (10% of patients) Sores on glans penis (20% patients) Saugelike fingers and toes Low back pain Reiter’s syndrome Management: Indomethacin up to 250 mg/d If Chlamydial tetracylines may shorten duration Will last 4-7 months May be recurrent Bursitis & Tendinitits Shoulder – major causes of pain: Elbow Lateral epicondylitis, olecranonbursitis Hip Subacromial bursitis, supraspinatuns tendinitits, bicipital tendinitis, rotator cuff Trochanteric, ischial, iliopsoas bursitis Knee Prepatellar, infrapatellar, anserine bursitis Bursitis & Tendinitis MANAGEMENT Conservative Ice, rest, NSAID’s Early ROM exercises for shoulder and elbow Olecranon and prepatellar bursitis Aspirate Cefazolin 1g iv q8hr SLE – the diagnosis (need > 4) Malar rash Discoid rash Photosensitivity Oral ulcers Arthritis Serositis Pleuritis Percarditis Renal disorder Neurologic disorder Hematologic disorder Seizures Psychosis Anemia Leukopenia Thrombocytopenia Blood tests ANA, anti-Sm Ab, antiDNA Ab, False + VDRL/RPR SLE - treatment NSAID’s : first line (don’t use if low platelets, GI involvement, renal disease) Corticosteroids: Minor: Prednisone 0.5 mg/kg/d Major: Prednisone 1g/kg/d Cerebritis or worsening glomerulonephritis: methylprednisolone 1 g iv Antimalarial Immunosuppression agents SLE – complications of immunosuppressive agents Cyclophosphamide Hemorragic cystitis Bladder carcinoma SIADH GI distress Alopecia Myelosuppression Neoplasia Infection Azathioprine GI distress Myelosuppression Hepatitis Pancreatitis Aseptic meningitis Neoplasia Infection Drugs that can cause a Lupuslike Syndrome Procainamide Quinidine Hydralazine Isoniazid Penecillin Sulphonamides Tetracycline Dilantin And the list goes on….. Vasculides Wegener’s Medium vessel disease Upper resp tract, Lower resp tract, then glomerulonephritis (85%), ocular findings and cerebral vasculitis (33%) Diagnosis: elevated ESR, + c-ANCA, - ANA, hematuria, active urine sediment CXR: sharply demarcated pulmonary nodules Management: steroids & cyclophosphamide, iv steroid for flares of glomerulonephritis Vasculides Henoch-Schonlein Purpura Usually affects children Triggers: viral infections, insect stings, drugs Presentation: purpuric rash, lower limb arthralgia, GI complaints (80%), gomerulonephritis (50%) Management: conservative, severe arthralgia or abdo pain give 1mg/kg/d prednisone, admit with iv steroids if renal involvement