* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Knee Anatomy
Survey
Document related concepts
Transcript
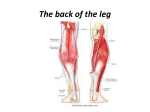
Knee Anatomy Reza Omid, M.D. Assistant Professor Orthopaedic Surgery Shoulder & Elbow Reconstruction Sports Medicine Keck School of Medicine of USC Bony Anatomy Tibiofemoral joint Patellofemoral joint Femoral Condyles – A– Lateral Condyle » Smaller radius of curvature » Smaller in all dimensions » Extends more anteriorly – B – Medial Condyle » Larger radius of curvature » Extends more distally – C – Intercondylar notch Tibial Plateau – D – Medial Plateau » Greater surface area » Concave » Circular shape – E – Intercondylar Eminence – F – Lateral Plateau » Smaller surface area » Convex » Oval shape Patella – Sesamoid bone in quadriceps – Dividing central ridge – Comprised of seven facets » Medial and Lateral facets divided into 3rds » 7th facet is most medial (odd facet) – Medial half usually smaller – Thick hyaline cartilage (5.5mm) Femoral Sulcus – Lateral wider and higher – Both with sagittal convexity Screw Home Mechanism • Knee achieves terminal extension via the “screw home mechanism • The tibia externally rotates in relation to the femur. • When the knee needs to flex, the popliteus contracts which causes internal rotation of the tibia and in essence unlocking the knee and allowing it to bend Bony Alignment Popliteal Artery Originates at the adductor hiatus and passes through the popliteal fossa, then deep to the fibrous arch over the soleus muscle Divides into the anterior and posterior tibial arteries at the distal aspect of the popliteus muscle Popliteal Artery • The popliteal artery is 9mm posterior to the posterior cortex of the tibia at 90° of flexion and even closer in extension. • Place retractors biased to the medial side when possible. Skin Blood Flow • If two longitudinal incisions are present, the more lateral incision should be used (if allows adequate exposure) because most of blood supply comes in medially. • The lateral skin edge is more hypoxic than the medial skin edge so keep this in mind when placing sutures. Tibial Nerve • Initially lateral to the popliteal artery • Crosses at midpoint to end medial to the artery at soleus arch Common Peroneal Nerve • Lateral aspect of the popliteal space • Medial and posterior to the biceps femoris tendon Infrapatellar Branch of Saphenous Patellofemoral Biomechanics Joint Reactive Force – In flexion, patella compressed onto femur creating joint reactive force – Stair climbing – 3.5 X BW – Deep bends – 7-8 X BW Menisci • • Primarily type I collagen with fibers arranged obliquely, radially, and vertically Outer 10% to 30% has blood supplied from the perimeniscal capillary plexus off the superior and inferior medial and lateral genicular arteries Meniscus Function Load Transmission – 50% load transmitted in extension – 85% load transmitted at 90 degrees flexion – Resection of 15-34% increases pressure 350% Secondary Stabilization – Medial meniscus provides anterior restraint » Especially in ACL deficient knee Lateral Meniscus • • • • • Loose peripheral attachment allows greater translation during motion – Average excursions of the menisci with knee flexion » 5.2 mm for the medial » 11 mm for the lateral Bare area anterior to popliteus tendon Two highly variable meniscofemoral ligaments attach it to medial femoral condyle: Anterior – Humphrey Posterior – Wrisberg’s Ligaments Tensile strengths of various knee ligaments: • MCL ~ 4400-5000N • PCL ~2500-3000N • ACL ~ 2200-2500N • LCL ~750N Anterior Cruciate Ligament – 26-38 (33) mm in length » ACL graft selection you aim for at least 100110mm graft length because it needs about ~33mm for the tibial tunnel, ~33mm for the femoral tunnel and ~33 for the graft itself – 11 mm in width – Primary restraint » Anterior translation of tibia (74-85%) » Normal 3-5mm of translation – Secondary restraint » Internal rotation » Varus/Valgus » Hyperextension Anterior Cruciate Ligament Two bands – Anteromedial band taut in flexion – Posterolateral band taut in extension Anterior Cruciate Ligament Femoral Attachment – – – – Posterior portion of medial surface of LFC Oriented in line of axis of femur in extension Footprint in shape of circular segment Posterior convexity 4 mm anterior to articular surface – Surface area measures 16-24 x 11 mm – Lateral to midline on AP view – Posterosuperior on lateral view Anterior Cruciate Ligament Tibial Attachment – – – – – – – Anterolateral to medial spine Insertion has oval shape Sections attach to bone, AHLM, PHLM 15 mm posterior to anterior tibia 17-30 x 11 mm surface area Just lateral to midline on AP 40% back on lateral view Lateral Bifurcate Ridge – Running perpendicular to the lateral intercondylar ridge) seperates the origins of the anteromedial and posterolaterla bundles. Lateral Intercondylear Ridge • Resident’s ridge on the lateral femoral condylar wall denotes the lateral intercondylear ridge and marks the most anterior and superior extent of the femoral origins of the ACL. Anterior Cruciate Ligament Blood Supply – ACL completely ensheathed in fold of synovial membrane – Although intraarticular, technically extrasynovial – Main supply is middle geniculate with smaller contribution from both inferior geniculates Innervation – Branches of tibial nerve – Very few pain receptors in substance of ACL Posterior Cruciate Ligament – 38 mm in length – 13 mm in width – Narrowest diameter at midsubstance – Anterolateral band » More robust, Taut in flexion – Posteromedial band » Thinner, Taut in extension Posterior Cruciate Ligament Femoral Attachment – Lateral surface MFC – Shape of circular segment – Distal margin 3 mm proximal to articular surface Posterior Cruciate Ligament Tibial Attachment – Depression between tibial plateaus – 1 cm distal to tibial articular surface – Can have contributions to PHLM as well as meniscofemoral ligaments – Average width 13 mm PCL Biomechanics Function – Primary restraint » Posterior translation of tibia (90-95%) » Greatest translation occurs at 75 degrees flexion – Secondary restraint » Varus/valgus » External rotation Medial Structures Layer 1: Deep fascia and Sartorius Layer 2: Superficial MCL, MPFL Layer 3: Joint capsule, Deep MCL Pes Anserinus Medial Ligaments • Superficial MCL (Medial Collateral Ligament) • Originates on medial epicondyle – avg: 3.2 mm proximal and 4.8 mm posterior to medial epicondyle • Tibial insertions (2) distal and proximal – Proximal: anterior arm of the semimembranosus tendon – Distal: broad-based, just anterior to the posteromedial crest of the tibia, most located within the pesanserine bursa • Posterior Oblique Ligament (POL) • superficial, central (main component), and capsular arms • Deep MCL – Divided into meniscofemoral and meniscotibial ligaments MCL MCL Biomechanics Stability – Most important in flexion when posterior structures relaxed – Valgus rotation – External rotation – Medial/Lateral translation Superficial MCL most important for stability (57-78%) Sectioning Deep MCL does not result in instability if Superficial MCL intact Medial Patellofemoral Ligament Runs transversely in Layer 2 Originates from adductor tubercle, femoral epicondyle, and superficial MCL Proximal fiber inserts on undersurface of VMO and vastus intermedius Distal fibers insert on superomedial patella Width averages 1.3 cm MPFL MPFL Biomechanics Soft tissue restraint of extensor mechanism Patella subluxes most easily at 20° knee flexion MPFL resists patellar lateral subluxation greatest in extension Primary stabilizer followed by patellomeniscal, patellotibial, and medial retinaculum Lateral Structures Layer 1 – IT band – biceps tendon – – – – – – – Layer 2 Lateral retinaculum patellofemoral ligaments Layer 3 Joint capsule LCL arcuate ligament fabellofibular ligament popliteofibular ligament Lateral Structures Layer 1 IT band biceps tendon Layer 2 Lateral retinaculum patellofemoral ligaments Layer 3 Joint capsule LCL arcuate ligament fabellofibular ligament popliteofibular ligament Iliotibial Band Coalescence at greater trochanter of tensor fascia lata, gluteus medius and gluteus maximus IT band continues distally to form the: – IT tract » Inserts distally on Gerdy’s tubercle and on distal femur through intermuscular septum – Iliopatellar band » Inserts on lateral patella resisting medial directed forces IT Band Biomechanics Functions – – – – Stabilizes against varus opening Knee extensor in extension Knee flexor in flexion External rotator of tibia in >40 flexion Lateral Collateral Ligament Arises in fovea slightly proximal (1.4 mm) and posterior (3.1 mm) to lateral epicondyle Attaches to V-shaped plateau of fibular head (8.2mm distal to anterior edge) Surrounded by biceps femoris tendon distally Average length 59-71 mm AP diameter 3.4 mm ML diameter 2.3 mm LCL Origin • • Posterior (4.6 mm) and proximal (1.3 mm) to the lateral femoral epicondyle Posterior and superior to the insertion of the poplitieus (18mm away from each other) LCL Biomechanics Tightest in extension, 0-30 degrees Becomes looser in flexion >30 degrees Primary restraint to varus Secondary restraint to ER and posterior translation Posterolateral Corner • FCL • Popliteus tendon • Popliteofibular lig Posterolateral Corner Static Stabilizers (highly variable) – – – – – – – – LCL Fabellofibular ligament Short lateral ligament Popliteofibular ligament Arcuate ligament Posterolateral capsule Posterior horn lateral meniscus Lateral coronary ligament Posterolateral Corner Dynamic Stabilizers – IT band – Lateral gastrocnemius – Biceps femoris – Popliteus Popliteus Complex Dynamic – Popliteus muscle Static – Popliteofibular ligament – Popliteotibial fascicle – Popliteomeniscal fascicle Popliteus Muscle • • Originates from posteromedial surface of proximal tibia Tendon passes in hiatus of coronary ligament, crosses under LCL, inserts on lateral femoral condyle 3-5 mm proximal to articular surface Popliteofibular ligament Average length 42 mm Descends from popliteus muscle (at musculotendinous junction) to posterosuperior fibular head Composed of anterior and posterior fascicle Functions as pulley to the popliteus Arcuate Ligament Fibers oriented in various directions Y-shaped configuration over popliteus Medial limb terminates into oblique popliteal ligament Lateral limb invariable present, and is less distinct Fabellofibular vs Short Lateral Ligament Fabellofibular ligament – Present when fabella present (8-16%) – Courses from fabella to fibular head Short lateral ligament – Present when fabella absent – Courses from lateral femur to fibular head – Represents a homologue of the fabellofibular ligament