* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download (Renal haemodynamic and GFR).
Cushing reflex wikipedia , lookup
Cardiac output wikipedia , lookup
Intracranial pressure wikipedia , lookup
Circulatory system wikipedia , lookup
Haemodynamic response wikipedia , lookup
Biofluid dynamics wikipedia , lookup
Renal function wikipedia , lookup
Blood pressure wikipedia , lookup
Hemodynamics wikipedia , lookup
Blood pressure measurement wikipedia , lookup
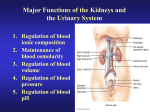
Renal Physiology 2: Renal Haemodynamic & Glomerular Filtration Rate Dr Ahmad Ahmeda [email protected] Mobile No: 0536313454 1 Learning Objectives • Describe that the mechanism of urine formation include three basic processes; glomerular filtration, tubular reabsorption and tubular secretion. • Define GFR and quote normal value. • Identify and describe the factors controlling GFR in terms of starling forces, permeability with respect to size, shape and electrical charges and ultra-filtration coefficient. • Describe Intrinsic and extrinsic mechanism that regulate GFR. • Describe autoregulation of GFR & tubuloglomerular feedback mechanism. 2 Blood supply to the kidney • Approximately one-fourth (1200 ml) of systemic cardiac output flows through the kidneys each minute • Arterial flow into and venous flow out of the kidneys follow similar paths • The cortex receives more than 90% of the blood that perfused into the kidney, which is perfused at a rate of about 500 ml/min per 100 gm tissue. (100 times greater than resting muscle blood flow) 3 Blood supply to the kidney • The remainder of the renal blood supply goes to the capsule and the renal adipose tissue. • Some of the cortical blood then passes to the medulla, the outer medulla has a blood flow of 100ml/min per 100 g tissue, and the inner medulla a flow of 20 ml/min per 100 g tissue. • Due to high blood flows to the cortex so, more oxygen than required and that lead to the arterio-venous oxygen difference is only 1-2 % 4 Blood supply to the kidney 5 1= interlobar arteries 1a= interlobar vein 2= arcuate arteries 2a= arcuate vein 3= interlobular arteries 3a= interlobular vein 4= stellate vein 5= afferent arterioles 6= efferent arterioles 7a,7b= glomerular capillary network 8,8a = descending vasa recta 9= ascending vasa recta 6 Capillary Beds of the Nephron • Every nephron has two capillary beds – Glomerulus – Peritubular capillaries • Each glomerulus is: – Fed by an afferent arteriole – Drained by an efferent arteriole • Blood pressure in the glomerulus is high because: – Arterioles are high-resistance vessels – Afferent arterioles have larger diameters than efferent arterioles • Fluids and solutes are forced out of the blood throughout the entire length of the glomerulus 7 Capillary Beds • Peritubular beds are low-pressure, porous capillaries adapted for absorption that: – Arise from efferent arterioles – adhere to adjacent renal tubules – Empty into the renal venous system • Vasa recta – long, straight efferent arterioles of juxtamedullary nephrons 8 9 Vascular Resistance in Microcirculation • Afferent and efferent arterioles offer high resistance to blood flow • Blood pressure declines from 95mm Hg in renal arteries to 8 mm Hg in renal veins • Resistance in afferent arterioles: – Protects glomeruli from fluctuations in systemic blood pressure • Resistance in efferent arterioles: – Reinforces high glomerular pressure – Reduces hydrostatic pressure in peritubular capillaries 10 11 Measurement of renal blood flow 1) Clearance methods: Use of a substance which is filtered, secreted but not reabsorbed by the nephrons and apply the clearance formula. An example is para-amino-hippuric acid (PAH) which is freely filtered, secreted by the organic pumps of the proximal tubule and is 100% removed on passage through the kidney. 12 Measurement of renal blood flow • Direct dynamic measurements: Electromagnetic flowmeter • Ultrasound flowmeter • Laser-Doppler flowmetry : Intrarenal haemodynamics 13 Proximal convoluted tubule Bowman’s capsule Afferent arteriole Peritubular capillaries Efferent arteriole Glomerular capillary bed High pressure vascular bed, increasing oncotic pressure Peritubular capillary bed, Low pressure vascular bed, high oncotic pressure. Good for filtration Good for re-absorption 14 Mechanisms of Urine Formation • The kidneys filter the body’s entire plasma volume 40 times each day. • The filtrate: – Contains all plasma components except protein – Loses water, nutrients, and essential ions to become urine • The urine contains metabolic wastes and unneeded substances 15 Mechanisms of Urine Formation • Urine formation and adjustment of blood composition involves three major processes – Glomerular filtration – Tubular reabsorption – Secretion 16 Glomerular Filtration • The first step in urine formation • Blood flows through the glomerulus, allowing protein-free plasma to be filtered through the glomerular capillaries into the Bowman’s capsule. • ~20% of plasma entering the glomerulus is filtered • 125 ml/min filtered fluid 17 Tubular Reabsorption • Movement of substances from tubular lumen back into the blood • Reabsorbed substances not lost in the urine, but are carried by the peritubular capillaries to the venous system • Most of the filtered plasma is reabsorbed 18 Tubular Secretion • The selective transfer of substances from the peritubular capillary into the tubular lumen • Allows for rapid elimination of substances from the plasma via extraction of the 80% of unfiltered plasma in peritubular capillaries and adding it to the substances already in tubule as result of filtration 19 Urine Excretion “The end product” • The elimination of substances from the body in the urine • All plasma constituents filtered or secreted, but not reabsorbed remain in the tubules and pass into the renal pelvis to be excreted as urine and eliminated from the body 20 Types of Tubular Reabsorption • Reabsorption can be transcellular (across the cell) or paracellular (between the cells) • Once the substance has moved pass the tubular epithelium cell into the interstitial space bulk flow then accounts for its movement back into the peritubular capillaries 21 Passive Reabsorption • Bulk flow results from the imbalance of osmotic or hydrostatic forces at the peritubular capillary. Exactly the same as at the peripheral capillary or the glomerulus 22 Active Reabsorption • Major substances are reabsorbed via active transport. These are substances that are needed by the body (e.g. Na+, glucose, aas, other electrolytes) • Sodium reabsorption-99.5% of filtered sodium is absorbed – Proximal tubules (67%) – Loop of Henle (25%) – Distal/Collecting tubules (8%) 23 Active Reabsorption • Active reabsorption is via primary active transport based on ATP hydrolysis (e.g. Na+) or secondary active transport based on an ion gradient (e.g. glucose) • Known transporters: – Na+/K+ ATPase – H+ ATPase – H+/K+ ATPase – Ca++ ATPase 24 Net Filtration Pressure (NFP) • The pressure responsible for filtrate formation • NFP equals the glomerular hydrostatic pressure (HPg) minus the oncotic pressure of glomerular blood (OPg) combined with the capsular hydrostatic pressure (HPc) NFP = HPg – (OPg + HPc) Or NFP = PGC – PBS - OGC 25 Glomerular Filtration Rate • Glomerular filtration rate (GFR) is the rate of production of filtrate at the glomeruli from plasma – Typically 80 – 140 ml/min depending on age, sex etc – Sum of the filtration rates of all functioning nephrons – Index of kidney function 26 GFR • Factors governing filtration rate at the capillary bed are: – Total surface area available for filtration – Filtration membrane permeability – Net filtration pressure • GFR is directly proportional to the NFP • Changes in GFR normally result from changes in glomerular blood pressure 27 GFR • If the GFR is too high: – Needed substances cannot be reabsorbed quickly enough and are lost in the urine • If the GFR is too low: – Everything is reabsorbed, including wastes that are normally disposed of 28 Filtration: glomerular hydrostatic pressure (GHP) push fluid out of vessels capsular hydrostatic pressure (CsHP) push fluid back into vessels net hydrostatic pressure (NHP) NHP = GHP - CsHP 35 = 50 - 15 mm Hg 29 Filtration: blood colloid osmotic pressure (BCOP) proteins in blood (hyperosmotic) draw water back into blood ~ 25 mm Hg 30 Filtration: FP = NHP - BCOP 10 = 35 - 25 mm Hg importance of blood pressure 20% drop in blood pressure 50mm Hg to 40mm Hg filtration would stop 31 • • Driven by Starling forces Pressure inside capillaries > Pressure outside movement of fluid from blood • Forces in capillaries: hydrostatic pressure PGC = + 60mmHg • oncotic pressure GC = - 29 mmHg net outward pressure = 60 – 29 = 31mmHg • Forces in capsule: hydrostatic pressure PBS = -15mmHg • oncotic pressure GBS = 0 mmHg • Overall: 31 – 15 = 16 mmHg outward • Male adults GFR: ~ 90 – 140 ml/min • Female: 80 – 125 ml/min • 125 ml/min usually good average 32 33