* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Creatinine
Survey
Document related concepts
Transcript
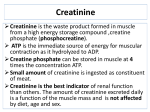
Kidney function test Functions of the kidney Regulation e.g. homeostasis ,water, acid/base Excretion e.g.uric acid, urea, creatinine Endocrine e.g. renin, erythropoietin, 1,25 dihydroxycholecalciferol- conversion only in kidney! When should you assess renal function? Risk factors for kidney disease: – Older age – Family history of Chronic Kidney disease (CKD) – Decreased renal mass – Low birth weight – US racial or ethic minority – Low income – Lower education level – Diabetes Mellitus (DM) – Hypertension (HTN) – Autoimmune disease – Systemic infections – Urinary tract infections (UTI) – Nephrolithiasis – Obstruction to the lower urinary tract – Drug toxicity Uric acid Uric acid is a chemical created when the body breaks down substances called purines. Purines are found in some foods and drinks, such as liver, anchovies, mackerel, dried beans and peas, beer, and wine. Purines are also a part of normal body substances, such as DNA. In humans, approximately 75% of uric acid excreted is lost in the urine; most of the reminder is secreted into the GIT If your body produces too much uric acid or doesn't remove enough if it, you can get sick. High levels of uric acid in the body is called hyperuricemia Normal values fall between 3.0 and 7.0 mg/dL. Note: Normal values may vary slightly from laboratory to laboratory. When is it ordered? when a doctor suspects high levels of uric acid : Gout monitoring test when a patient has undergone chemotherapy or radiation if a patient appears to have failing kidneys Greater-than-normal levels of uric acid (hyperuricemia) may be due to: Alcoholism Diabetes Gout Hypoparathyroidism Lead poisoning Leukemia Nephrolithiasis Polycythemia vera Renal failure Toxemia of pregnancy Purine-rich diet Excessive exercise Chemotherapy-related side effects Lower-than-normal levels of uric acid may be due to: Fanconi syndrome Wilson's disease Syndrome of inappropriate antidiuretic hormone (SIADH) secretion Multiple Sclerosis Low purine die Gout Gout is a kind of arthritis that occurs when uric acid builds up in the joints. In Gout increased serum levels of uric acid lead to formation of monosodium urate crystals around the joints. Acute gout is a painful condition that typically affects one joint. Chronic gout is repeated episodes of pain and inflammation, which may involve more than one joint. The exact cause is unknown. Gout may run in families. It is more common in males, postmenopausal women, and people who drink alcohol Symptoms of acute gouty attacks: Symptoms develop suddenly and usually involve only one or a few joints. The big toe, knee, or ankle joints are most often affected . The pain frequently starts during the night and is often described as throbbing, crushing, or excruciating . The joint appears warm and red. It is usually very tender. There may be a fever . The attack may go away in several days, but may return from time to time. Additional attacks usually last longer . After a first gouty attack, people will have no symptoms. Some people will go months or even years between gouty attacks. Some people may develop chronic gouty arthritis, but others may have no further attacks. Those with chronic arthritis develop joint deformities and loss of motion in the joints. They will have joint pain and other symptoms most of the time. Tophi are lumps below the skin around joints or in other places. They may drain chalky material. Tophi usually develop only after a patient has had the disease for many years. After one gouty attack, more than half of people will have another attack. A tophus on the elbow of a middle aged man with chronic gout . Tests that may be done include: Synovial fluid analysis Gold standard to confirm gout, Urate crystals identified by: - Needle and rod shapes Uric acid - blood Joint x-rays) may be normal) X-ray of gouty uric acid deposit in the big toe (left ) Possible Complications Chronic gouty arthritis Kidney stones Deposits in the kidneys, leading to chronic kidney failure Treatment Treatments for a sudden attack or flare-up of gout : Your doctor will recommend that you take nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, naproxen, or indomethacin as soon as your symptoms begin Your health care provider may occasionally prescribe strong painkillers such as codeine Daily use of allopurinol decrease uric acid levels in your blood Some diet and lifestyle changes may help prevent gouty attacks : Avoid alcohol, sardines, oils, organ meat (liver, kidney, and sweetbreads( Limit how much meat you eat at each meal. Avoid fatty foods such as salad dressings, ice cream, and fried foods Eat enough carbohydrates If you are losing weight, lose it slowly. Quick weight loss may cause uric acid kidney stones to form. Specimen Serum or plasma may be used; slight but insignificant positive bias (0.2 mg/dL) has been noted in plasma specimens as compared with serum. Stability in serum / plasma: 6 months at -20°C 7 days at 4-8°C 3 days at 20-25°C Enzymatic Colorimetric 1-Uric acid + H2O + O2 Uricase Allantion + CO2 + H2O2 2-TBHBA + 4- Aminoantipyrine + 2H2O2 Quinoneimine + 3 H2O POD -Uric acid is oxidized to allantoin by uricase. -The generated hydrogen peroxide reacts with 4aminophenazone/ESPT to quinoneimine. Note: Uric acid may also form kidney stones Although uric acid can act as an antioxidant, excess serum accumulation is often associated with cardiovascular disease. urea Urea is a relatively nontoxic nitrogen containing substance made by the liver to dispose of ammonia resulting from protein metabolism. Its elimination in the urine represents the major route for nitrogen excretion. The reference interval for serum urea of healthy adults is 5-39 mg/dl (slightly higher in males than females) BUN = (blood urea nitrogen) The real urea concentration is BUN x 2.14 Increased BUN = Azotemia Causes: – Increased protein catabolism: Increased dietary protein Severe tress: MI, fever, etc Rhabdomyolysis Upper GI bleeding – Impaired renal function Pre renal azotemia: renal hypoperfusion Renal azotemia: acute tubular necrosis Post renal azotemia: obstruction of urinary flow Decreased BUN Decreased dietary protein Increased protein synthesis ( Pregnant women , children ) severe liver disease SIADH Overhydration (IV fluids) The key to identifying the azotemia as prerenal is the increase of plasma urea without parallel increase of plasma creatinine. With obstruction, both plasma urea and creatinine increase, but there is greater rise of urea than of creatinine because the obstruction of urine flow backpressure on the tubule and back diffusion of urea into blood from the tubule. BUN / Creatinine Ratio Pre-renal BUN is more susceptible to non-renal factors Post-renal Both BUN and Creat. are elevated Increased BUN Normal Creat Increased BUN Increased Creat Specimen -Serum and heparinized plasma can be used for the urease/GLDH methods. -Fluoride will inhibit the urease reaction; therefore methods employing urease cannot use serum preserved with fluoride. -Ammonium heparin also cannot be used as an anticoagulant for urease methods. -Stability in serum or plasma: 7 days at 4–8°C 1 year at -20°C -Because of urea’s susceptibility to bacterial degradation, serum and urine samples should be kept at 4° to 8° C until analysis. Urease/GLDH Method -The method is optimized for 2-point kinetic measurement. -Decrease in absorbance at 340 nm is proportional to concentration of urea. creatinine Creatine is synthesized in the kidneys and liver It is then transported in blood to other organs such as muscle and brain, where it is phosphorylated to phosphocreatine, a highenergy compound. Interconversion of phosphocreatine and creatine is a particular feature of metabolic processes of muscle contraction Creatinine -Creatinine is a non-protein nitrogen waste product formed in muscle. Creatine Phosphate – phosphoric acid = Creatinine Creatine – water = Creatinine -Creatine is synthesized in liver from some a.a (glysine, methionine, arginine). -Filtered by kidney and excreted in the urine. -Creatinine filters easily into the glomerular filtrate and is not reabsorbed by the tubule. -The plasma levels of creatinine are related to the muscle mass. 1 to 2% of muscle creatine spontaneously converts to creatinine daily and released into body fluids at a constant rate. Endogenous creatinine produced is proportional to muscle mass, it is a function of total muscle mass the production varies with age and sex creatinine The breakdown product of creatine phosphate released from skeletal muscle at a steady rate. It is filtered by the glomerulus. It is generally a more sensitive and specific test for renal function than the BUN. Normal range is 0.6-1.3 mg/dL– *non pregnant state-* Increased serum creatinine: – Impaired renal function – Very high protein diet – Vary large muscle mass: body builders, giants, acromegaly patients – Rhabdomyolysis/crush injury – Athletes taking oral creatine – Drugs: • Probenecid • Cimetidine • Triamterene • Trimethoprim • Amiloride Specimen -One can analyze serum, plasma, or diluted urine. -The common anticoagulants (fluoride and heparin) do not cause interference, though heparin, which can be formulated as the ammonium salt, must be avoided in enzymatic methods that measure ammonia production. -Storage 7 days at 4-25oC At least 3 months at -20oC Specimen -Urine should be diluted 1:100 -Bacterial contamination has been found to falsely lower creatinine values measured using the Jaffé reaction. -The mechanism of this interference appears to be bacterial production of a substance that retards the rate of the Jaffé reaction. Enzymatic Method Creatinine aminohydrolase Creatinine + H2O Creatine +ATP Creatine Creatine Kinase Creatine-P + ADP Pyruvate Kinase ADP + Phosphoenolpyruvate Pyruvate + NADH Lactate dehydrogenase ATP + Pyruvate Lactate + NAD+ -The difference in absorbance at fixed times during conversion is proportional to the concentration of creatinine in the sample. Principle of of Clearance Some substances when filtered enter the tubules are not reabsorbed and so 100% excreted= GFR (inulin= gold standard for GFR, creatinine (but this one partially reabsorbed, particularly in uremia, then clearance <GFR Some substances are filtered, enter tubules, and more of the substance is secreted enters the tubules by excretion. Clearance>GFR Some substances are filtered, enter tubules, but are completely reabsorbed, so they did not reach the final urine (e.g. cystatin C) Clearance is defined as the (hypothetical) quantity of blood or plasma completely cleared of a substance per unit of time. The most frequently used clearance test is based on the measurement of creatinine. The 'clearance' of creatinine from plasma is directly related to the GFR if: The urine volume is collected accurately There are no ketones or heavy proteinuria present to interfere with the creatinine determination. It should be noted that the GFR decline with age (to a greater extent in males than in females) and this must be taken into account when interpreting results. Creatinine clearance in adults is normally about of 120 ml/min Plasma creatinine Plasma creatinine concentration is inversely related to the GFR But GFR can decrease by 50% before plasma creatinine concentration rises beyond the normal range this means that a normal plasma creatinine does not necessarily imply normal renal function, A Raised creatinine usually indicates impaired renal function Changes in plasma creatinine concentration can occur, independently of renal function, due to changes in muscle mass. Decrease can occur as a result of starvation and in wasting diseases, immediately after surgery.