* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download NTDs and eye health: lessons learnt and opportunities for
Survey
Document related concepts
Transcript
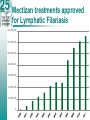
NTDs and eye health: lessons learnt and opportunities for collaboration Adrian D Hopkins Director: Mectizan Donation Program Task Force for Global Health Emory University; Atlanta, USA NTDs and Eye Health Trachoma • Strategy for eliminating blinding Trachoma – – – – Surgery of Trichiasis Antibiotic MDA Facial cleanliness Environmental Change NTDs and Eye Health Onchocerciasis • Strategy for elimination of the disease – MDA – (Rehabilitation of the blind) Other NTDs and MDA • Lymphatic Filariasis – Strategy for Elimination – MDA – Morbidity control • Shistosomiasis – MDA – Water and Sanitation – ?? Snail control • STH – MDA – Water and Sanitation Community Directed Treatment with Ivermectin (CDTI) in action Mectizan treatments approved for Onchocerciasis 160000000 140000000 120000000 100000000 80000000 60000000 40000000 20000000 0 Mectizan treatments approved for Lymphatic Filariasis 140,000,000 120,000,000 100,000,000 80,000,000 60,000,000 40,000,000 20,000,000 0 Other NTDs • NTDs without community diagnosis methods • NTDs with difficult or toxic treatments • NTDs with complicated individual diagnostic tools • These diseases require Intensified Disease Management (IDM) for case finding, laboratory diagnosis and individual care • HAT, Leprosy, Chagas Disease, Leishmaniasis, Leprosy, Buruli Ulcer and others What are NTDs and relationship to Blindness • Both diseases of the poor – More prevalent in the “bottom billion” – Occur where health services are inaccessible – The two major causes of infectious blindness are NTDs for MDA – No simple strategies for some diseases. • Disease management strategies – Community diagnosis – Require community mobilisation – Require a multi-sectorial approach Community involvement Linking CBR, VHWs, and CDDs • Same community but different programmes and different workers. WHY? – Why are there different vertical programmes with different funding sources and controls? – Is it impossible to coordinate eye care with other activities? • Why is CBR not empowering enough to become CDR? Advocacy • Clear simple messages – – – – Tool ready strategies Simple cost strategies Clear results Defined impact • Success in what you can do leads to research funding for what you cannot do • Long-term commitment. – NO 3 year programmes. Needs for Political Commitment • Need wide stakeholder input at international and national level, WHO, governments (MoH M of Finance, M of Education) with NGDOs and WHO in country. • Need peer pressure between governments, using regional meetings (success of APOC) • Need to involve local governments. Local priority setting • Need strong advocacy to medical authorities. Challenges with Integration • Morbidity Control and prevention – – – – – Emphasis on MDA - pill packages & coverage Who will attend to the visually impaired Who will care for eyes and limbs Who will do the health education Who will attend to water and sanitation • Specificity – Reduction to lowest common denominator – No flexibility for alternative drug regimens – What about specific control/elimination parameters Let’s finish the job properly!