* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download pedsPhysAirway
Prenatal nutrition wikipedia , lookup
Maternal health wikipedia , lookup
Transmission (medicine) wikipedia , lookup
Patient safety wikipedia , lookup
Prenatal testing wikipedia , lookup
Fetal origins hypothesis wikipedia , lookup
Prenatal development wikipedia , lookup
Neonatal intensive care unit wikipedia , lookup
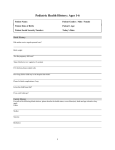
Pediatric Fundamentals McGraw-Hill 2002 Pediatric Fundamentals Objectives Explain and apply to your anesthetic practice selected elements of pediatric Growth and development Cardiovascular physiology Respiratory physiology including Airway maintenance Pediatric Fundamentals – Prenatal Growth and Development Prenatal Embryonic period first 8 weeks Organogenesis 4th – 8th weeks Ectoderm Mesoderm Endoderm Pediatric Fundamentals – Prenatal Growth and Development Organogenesis 4th – 8th weeks Mesoderm somites myotomes -> segmental muscles of trunk dermatomes -> dermis of scalp, neck, trunk sclerotomes -> vertebral bodies, arches abnormal induction -> spinal bifida Pediatric Fundamentals – Prenatal Growth and Development Developmental Abnormalities congenital diaphragmatic hernia (CDH) esophageal atresia spina bifida Hirschsprung’s disease omphalocele gastroschisis Pediatric Fundamentals – Prenatal Developmental Abnormalities Congenital diaphragmatic hernia (CDH) 1 in 2,500 live births 85% left side of diaphragm defect in closure of pleuroperitoneal canal impaired lung growth prenatal (intrauterine) repair possible Pediatric Fundamentals – Prenatal Developmental Abnormalities Esophageal atresia failure of proliferation of esophageal endoderm in 5th week 5 types – some with associated tracheoesophageal fistula + E = H-type (7%) 10% 1% 80% 2% Pediatric Fundamentals – Prenatal Developmental Abnormalities Spina bifida failure of closure of posterior neural tube during 3rd embryonic week mild: spina bifida occulta severe: meningomyelocele 80% lumbosacral in utero repair described Pediatric Fundamentals – Prenatal Developmental Abnormalities Hirschsprung’s disease defect in neural crest migration leads to paralysis of that segment of colon with subsequent proximal dilation Pediatric Fundamentals – Prenatal Developmental Abnormalities Omphalocele 1 in 2,500 live births failure of return of midgut from yolk sac to abdomen by 10 weeks often associated with other abnormalities Pediatric Fundamentals – Prenatal Developmental Abnormalities Gastroschisis 1 in 10,000 live births abdominal wall defect between developing rectus muscles just lateral to umbilicus right side may be due to abnormal involution of right umbilical vein during 5th and 6th weeks usually not associated with other defects Pediatric Fundamentals – Prenatal Growth and Development Consequences of maternal disorders on intrauterine development epilepsy history of previous child with neural tube defect diabetes mellitus substance abuse alcohol tobacco cocaine benzodiazepines infectious diseases rubella toxoplasmosis human immunodeficiency virus (HIV) herpes simplex Pediatric Fundamentals –Consequences of Maternal Disorders Epilepsy Congenital anomalies 2 to 3 times more frequent Appear to associated with increase risk of malformation: phenytoin valproic acid multidrug therapy Neural tube defects (e.g. spina bifida) valproic acid carbamazepine low dose folate may decrease risk Pediatric Fundamentals – Consequences of Maternal Disorders History of previous neural tube defect: Risk of subsequent neural tube defect increased 10 times Pediatric Fundamentals – Consequences of Maternal Disorders Diabetes mellitus Increased incidence of stillbirth congenital malformations risk of major malformation (8 times greater) hypertophic cardiomyopathy in IDM increased rate of high birth weight Pediatric Fundamentals – Consequences of Maternal Disorders Substance abuse alcohol Fetal alcohol syndrome intrauterine growth retardation (IUGR) microcephaly characteristic facies CNS abnormalities with intellectual deficiency Increased incidence of other major malformations Pediatric Fundamentals – Consequences of Maternal Disorders Tobacco Cocaine prematurity clinical seizures EEG abnormalities neurobehavioral abnormalities cerebral hermorrhagic infarction Benzodiazepines: no clear teratogenic link sedation and/or withdrawal symptoms reported Pediatric Fundamentals – Consequences of Maternal Disorders Infectious disease Rubella Chromosomal abnormalities IUGR Ocular lesions Deafness Congenital cardiomyopathy Especially with infections before week 11 Pediatric Fundamentals – Consequences of Maternal Disorders Infectious disease Toxoplasmosis IUGR Nonimmune hydrops Hydrocephalus Microcephaly Later neurologic damage Prompt spiramycin Rx until after delivery decreases risk 50% Pediatric Fundamentals – Consequences of Maternal Disorders Infectious disease Human immunodeficiency virus (HIV) Transmission to fetus: 12 – 30% less if mother taking Zidovudine (no teratogenesis reported) First signs appear at 6 months of age Median survival 38 months Pediatric Fundamentals – Consequences of Maternal Disorders Infectious disease Herpes simplex Neonatal infections Two-thirds caused by asymptomatic genital infection High morbidity and mortality Seizures Psychomotor retardation Spasticity Blindness Learning disabilities Death Maternal active infection: C-section indicated to decrease risk Pediatric Fundamentals – Consequences of Maternal Disorders IUGR 3-7% of all pregnancies Major cause of perinatal morbidity and mortallity Prognosis depends on specific cause Up to 8% have major malformations Head growth important determinant of neurodevelopmental outcome (IUGR + HC < 3rd%ile -> abnormal neurodevelopment likely) Hemodynamic changes and/or infectious disease often involved Pediatric Fundamentals - Prematurity Definitions premature: gestational age less than 37 weeks or 259 days moderately premature: 31-36 weeks severely premature: 24-30 weeks postterm: greater than 41 weeks low birth weight (LBW): < 2,500 Gm (only a bit over half of LBW infants are premature) very low birth weight (VLBW): < 1,500 Gm newborn: first day of life neonate: first month of life infant: first year of life Pediatric Fundamentals - Prematurity 5-10% of live births High morbidity and mortality due to immature organ systems Responsible for 75% of perinatal deaths Immediate/early complications hypoxia/ischemia intraventricular hemorrhage sensorineural injury respiratory failure necrotizing enterocolitis cholestatic liver disease nutrient deficiency social stress Pediatric Fundamentals - Prematurity Special considerations Respiratory breathing may initially be exclusively nasal spontaneous neck flexion may cause airway obstruction and apnea diaphragm is most important respiratory muscle fewer diaphragmatic type I fibers (10% vs 25%) maternal betamethasone or dexamethasone 48 hours before delivery increases surfactant production and decreases mortality after 30 weeks gestation Pediatric Fundamentals - Prematurity Special considerations Respiratory apneas 25% of all prematures alleviated with caffeine or theophylline PEEP stimulation may be exacerabated by general anesthesia especially infants < 50 weeks postconceptional age Pediatric Fundamentals - Prematurity Special considerations Cardiovascular PDA - treatment fluid restriction diuretics indomethacin surgical ligation Cardiac output relatively dependent on heart rate Immature sympathetic innervation Pediatric Fundamentals - Prematurity Special considerations Renal urine flow begins 10-12 weeks gestation decreased in premature (compared to full term) GFR renal tubular Na threshold glucose threshold bicarbonate threshold relative hypoaldosteronism with increased risk of hyperkalemia tubular function develops significantly after 34 weeks Pediatric Fundamentals - Prematurity Special considerations Nervous system Brain has 2 growth spurts 1. neuronal cell multiplication 15-20 weeks gestation 2. glial cell multiplication 25 weeks to 2 years of life Blood vessels more fragile increased risk of intracerebral hemorrhage Periventricular leukomalacia ischemic cerebral complication 12-25% of LBW infants increase risk of mental handicap Retinopathy of prematurity Pediatric Fundamentals - Prematurity Special considerations Thermal problems Immature thermoregulation system Body heat loss by evaporation conduction convection radiation Pediatric Fundamentals - Growth and Development Maturational change in form and function Prenatal Growth Gestational age (wks) Mean birth wt (Gm) 25 850 28 1000 30 1400 33 1900 37 2900 40 3500 Postnatal Growth Birth weight doubles by 5 months triples by 1 year Birth length doubles by 4 years Pediatric Fundamentals - Growth and Development Maturational change in form and function Percent body water Term newborn 80 1 year old 70 Adult 60 Surface area:Weight premature > full term > infant > child greater surface area greater evaporative heat loss rapid hypothermia if unprotected Girls Boys Puberty onset 11 years 11½ years Peak growth Tanner stage 3 Tanner stage 4 Pediatric Fundamentals - Growth and Development Fluid requirements Metabolism of one calorie of energy consumes one ml of H2O, so fluid requirements thought to reflect caloric requirement: Body weight (kg) Calories needed (kcal/kg/day) = Fluid requirement (ml/kg/day) 0-10 100 10-20 1000 + 50/(kg>10) > 20 1500 + 20/(kg>20) Dividing by 24 (hours/day) yields the famous 4:2:1 Rule for hourly maintenance fluid: 4 ml/kg/hr 1st 10 kg + 2 ml/kg/hr 2nd 10 kg + 1 ml/kg/hr for each kg > 20 Pediatric Fundamentals - Growth and Development Airway/respiratory system Gas exchange first possible approximately 24 weeks gestation Surfactant production appears by approximately 27 weeks produced of Type II pneumocytes exogenous form available Number (and size) of alveoli increase to age 8 years (size only after 8 years) First breaths of air pneumothorax or pneumomediastinum less than 1% several hours to reach normal lower lung fluid levels some expelled during birth canal compression transient tachypnea of newborn (TTN) increased incidence after C-section Pediatric Fundamentals - Growth and Development Respiratory rate/rhythm pauses up to 10 seconds normal in prematures without cyanosis or bradycardia Age (years) Normal Rate 1-2 20 - 40 2-3 20 – 30 7-8 15 - 25 Obligate nose breathing especially prematures able to mouth breath if nares occluded 80% of term neonates almost all term infants by 5 months Pediatric Fundamentals - Growth and Development Airway differences – infant vs adult epiglottis and tongue relatively larger glottis more superior, at level of C3 (vs C4 or 5) cricoid ring narrower than vocal cord aperture until approx 8 years of age 4.5 mm in term neonate 11 mm at 14 years Pediatric Fundamentals - Growth and Development Cardiovascular system In utero circulation placenta -> umbilical vein (UV)-> ductus venosus (50%) -> IVC -> RA -> foramen ovale (FO) -> LA -> Ascending Ao -> SVC -> RA -> tricuspid valve -> RV (2/3rds of CO) -> main pulmonary artery (MPA) -> ductus arteriosus (DA) (90%) -> descending Ao -> umbilical arteries (UAs)-> Pediatric Fundamentals - Growth and Development Cardiovascular system Transition to postnatal circulation Loss of large low-resistance peripheral vascular bed, the placenta (UV, UAs constrict over several days) With first air breathing marked drop in pulmonary vascular resistance with greatly increased pulmonary blood flow LA pressure > RA pressure closes FO Elevated PaO2 constricts DA hours to days Hgb F impairs postnatalO2 delivery Higher newborn resting cardiac index with decreased ability to further increase Pediatric Fundamentals - Growth and Development Cardiovascular system Normal murmurs up to 80% of normal children vibratory Still’s murmur basal systolic ejection murmur physiologic peripheral pulmonic stenosis (PSS) venous hum carotid bruit S3 Murmur only in diastole = abnormal Pediatric Fundamentals - Growth and Development Gastrointestinal notes Gastric pH higher at birth; decreases over several weeks Young infants diminished lower esophageal sphincter tone 50% have daily emesis (usually remits by 18 months) more show reflux if esophageal pH monitored only 1 in 600 develop complications of reflux Physiologic jaundice Colic < 3 months Umbilical hernia common frequently resolve spontaneously Teeth primary: 7 months to 2 or 3 years permanent: 6 years to 20 years Pediatric Fundamentals - Growth and Development Renal system Urine production begins first trimester Newborn GFR low (correlates with gestational age/size in prematures) rises sharply first 2 weeks adult values by age 2 years limited concentrating ability (600 vs adult 1200 mOsm/kg) ability to dilute urine relatively intact Pediatric Fundamentals - Growth and Development Hematologic system Infant Hgb F – higher O2 affinity Hgb A production largely replaces Hgb F by 4 months Hgb/Hct decrease to nadir at about age 2 months exaggerated in prematures (low total body Fe stores) Blood volume (ml/kg) Prematures 105 Term newborn 85 Adult 65 Pediatric Fundamentals - Growth and Development Neuro notes Nervous system anatomically complete at birth except: Myelination rapid for 2 years complete by 7 years Posterior fontanelle closed by 6 weeks Anterior fontanelle closed by 18 months Primitive reflexes disappear in few months Pediatric Fundamentals - Growth and Development Developmental pediatrics Approach to patient depends on stage of development Stranger anxiety 7 months 25% 9 50 12 75 Toddlers magical thinking (belief that own thought or deed causes external events) temper tantrums (aggravated if tired, ill, uncomfortable) Toilet training ability develops by 18 months usually complete by 2 to 3 years (day before night) bedwetting 15 - 20 % at 5 years with gradual decrease to 1% at 15 years 6 -11 years - concrete operations phase can consider different points of view develop explanation based on observation beginning logical reasoning but still tend to dogmatic 11 and older - development of abstract thinking Adolescent - increasing need for autonomy, participation in care http://metrohealthanesthesia.com/edu/ped/pedspreop3.htm Pediatric Fundamentals - Growth and Development Developmental pediatrics History and physical notes Newborn – pregnancy and delivery Infancy – developmental milestones Toddler – poor localization of symptoms and very suggestible (e.g., pharyngitis or pneumonia presenting as abdominal pain or distress) Older child – involve in discussion/decision Preadolescent and older – consider interview without parents Exam opportunistic approach in infants and young children observation essential distraction useful Pediatric Fundamentals – Heart and Circulation Embryology 1. Cardiovascular system begins forming at 3 weeks (diffusion no longer adequate) 2. Angiogenetic cell cluster and blood islands -> intraamniotic blood vessels 3. Heart tube 4. Heart begins to beat 22 – 23 days 5. Heart looping -> 4 chambers, 27 – 37 days 6. Valves 6 – 9 weeks Pediatric Fundamentals – Heart and Circulation Transitional circulation Placenta Out and Lungs In PVR drops dramatically (endothelial-derived NO and prostacyclin) FO closes DA closes 10-12 hours to 3 days to few weeks prematures: closes in 4-12 months PFO potential route for systemic emboli DA and PFO routes for R -> L shunt in PPHN Pediatric Fundamentals – Heart and Circulation Persistent pulmonary hypertension of the newborn (PPHN) Old PFC misnomer Primary Secondary meconium aspiration sepsis birth asphyxia Treatment cardiopulmonary support inhaled NO ECMO Pediatric Fundamentals – Heart and Circulation Nitric oxide (NO) – cGMP transduction pathway l-arginine ↓ eNOS (endothelial NO synthetase) oxidation of quanidine N moiety NO activates ↓ GTP ↓ sGC (soluble guanylate cyclase) cGMP (cyclic-3’,5’-guanosine monophosphate) activates ↓ protein kinase PDE (phosphodiesterase) GMP Pediatric Fundamentals – Heart and Circulation Neonatal myocardial function Contractile elements comprise 30% (vs 60% adult) of newborn myocardium Alpha isoform of tropomyosin predominates more efficient binding for faster relaxation at faster heart rates Relatively disorganized myocytes and myofibrils Most of postnatal increase in myocardial mass due to hypertrophy of existing myocytes Diminished role of relatively disorganized sarcomplasmic reticulum (SR) and greater role of Na-Ca channels in Ca flux so greater dependence on extracellular Ca may explain: Increased sensitivity to calcium channel blockers (e.g. verapamil) hypocalcemia digitalis Pediatric Fundamentals – Heart and Circulation Myocardial energy metabolism Young infant heart lactate: primary metabolite later: glucose oxidation and amino acids (aa’s) metabolize glucose and aa’s under hypoxic conditions (may lead to greater tolerance of ischemic insults) Gradual transition to adult: fatty acid primary metabolite by 1-2 years Pediatric Fundamentals – Heart and Circulation Normal aortic pressures Wt (Gm) 1000 2000 3000 4000 Age (months) 1 3 6 9 12 Sys/Dias 50/25 55/30 60/35 70/40 mean 35 40 50 50 Sys/Dias mean 85/65 50 90/65 50 90/65 50 90/65 55 90/65 55 Pediatric Fundamentals – Heart and Circulation Adrenergic receptors Sympathetic receptor system Tachycardic response to isoproterenol and epinephrine by 6 weeks gestation Myocyte β-adrenergic receptor density peaks at birth then decreases postnatally but coupling mechanism is immature Parasympathetic, vagally-mediated responses are mature at birth (e.g. to hypoxia) Babies are vagotonic Pediatric Fundamentals – Heart and Circulation Normal heart rate Age (days) 1-3 4-7 8-15 Rate 100-140 80-145 110-165 Age (months) Rate 0-1 100-180 1-3 110-180 3-12 100-180 Age (years) 1-3 3-5 5-9 9-12 12-16 Rate 100-180 60-150 60-130 50-110 50-100 Pediatric Fundamentals – Heart and Circulation Newborn myocardial physiology Type I collagen (relatively rigid) predominates (vs type III in adult) Cardiac output Starling response Compliance Afterload compensation Ventricular interdependence Neonate HR dependent limited less limited high Adult SV & HR dependent normal normal effective relatively low So: Avoid (excessive) vasoconstriction Maintain heart rate Avoid rapid (excessive) fluid administration Pediatric Respiratory Physiology Pediatric Respiratory Physiology Prenatal – Embryo Ventral pouch in primitive foregut becomes lung buds projecting into pleuroperitoneal cavity Endodermal part develops into airway alveolar membranes glands Mesenchymal elements develop into smooth muscle cartilage connective tissue vessels Pediatric Respiratory Physiology Prenatal Development Pseudoglandular period – starting 17th week of gestation Branching of airways down to terminal bronchioles Canalicular period Branching in to future respiratory bronchioles Increased secretary gland and capillary formation Terminal sac (alveolar) period 24th week of gestation Clusters of terminal air sacs with flattened epithelia Pediatric Respiratory Physiology Surfactant Produced by type II pneumocytes appear 24-26 weeks (as early as 20 weeks) Maternal glucocorticoid treatment 24-48 hours before delivery accelerates lung maturation and surfactant production Premature birth – immature lungs -> IRDS (HMD) due to insufficient surfactant production Pediatric Respiratory Physiology Prenatal Development Proliferation of capillaries around saccules sufficient for gas exchange 26-28th week (as early as 24th week) Formation of alveoli 32-36 weeks saccules still predominate at birth Pediatric Respiratory Physiology Prenatal Development Lung Fluid expands airways -> helps stimulate lung growth contributes ⅓ of total amniotic fluid prenatal ligation of trachea in congenital diaphragmatic hernia results in accelerated growth of otherwise hypoplastic lung (J Pediatr Surg 28:1411, 1993) Pediatric Respiratory Physiology Perinatal adaptation First breath(s) up to 40 (to 80) cmH2O needed to overcome high surface forces to introduce air into liquid-filled lungs adequate surfactant essential for smooth transition Elevated PaO2 Markedly increased pulmonary blood flow -> increased left atrial pressure with closure of foramen ovale Pediatric Respiratory Physiology Postnatal development Lung development continues for 10 years most rapidly during first year At birth: 20-50x107 terminal air sacs (mostly saccules) only one tenth of adult number Development of alveoli from saccules essentially complete by 18 months of age Pediatric Respiratory Physiology Infant lung volume disproportionately small in relation to body size VO2/kg = 2 x adult value => ventilatory requirement per unit lung volume is increased less reserve more rapid drop in SpO2 with hypoventilation Pediatric Respiratory Physiology Neonate Lung compliance high elastic fiber development occurs postnatally static elastic recoil pressure is low Chest wall compliance is high cartilaginous ribs limited thoracic muscle mass More prone to atalectasis and respiratory insufficiency especially under general anesthesia Infancy and childhood static recoil pressure steadily increases compliance, normalized for size, decreases Pediatric Respiratory Physiology Infant and toddler more prone to severe obstruction of upper and lower airways absolute airway diameter much smaller that adult relatively mild inflammation, edema, secretions lead to greater degrees of obstruction Pediatric Respiratory Physiology Control of breathing – prenatal development fetal breathing during REM sleep depressed by hypoxia (severe hypoxia -> gasping) may enhance lung growth and development Pediatric Respiratory Physiology Control of breathing – perinatal adaptation Neonatal breathing is a continuation of fetal breathing Clamping umbilical cord is important stimulus to rhythmic breathing Relative hyperoxia of air augments and maintains rhythmicity Independent of PaCO2; unaffected by carotid denervation Hypoxia depresses or abolishes coninuous breathing Pediatric Respiratory Physiology Control of breathing – infants Ventilatory response to hypoxemia first weeks (neonates) transient increase -> sustained decrease (cold abolishes the transient increase in 32-37 week premaures by 3 weeks sustained increase Ventilatory response to CO2 slope of CO2-response curve decreases in prematures increases with postnatal age neonates: hypoxia shifts CO2-response curve and decreases slope (opposite to adult response) Pediatric Respiratory Physiology Periodic breathing apneic spells < 10 seconds without cyanosis or bradycardia (mostly during quiet sleep) 80% of term neonates 100% of preterms 30% of infants 10-12 months of age may be abolished by adding 3% CO2 to inspired gas Pediatric Respiratory Physiology Central apnea apnea > 15 seconds or briefer but associated with bradycardia (HR<100) cyanosis or pallor rare in full term majority of prematures Pediatric Respiratory Physiology Postop apnea in preterms Preterms < 44 weeks postconceptional age (PCA): risk of apnea = 20-40% most within 12 hours postop (Liu, 1983) Postop apnea reported in prematures as old as 56 weeks PCA (Kurth, 1987) Associated factors extent of surgery anesthesia technique anemia postop hypoxia (Wellborn, 1991) 44-60 weeks PCA: risk of postop apnea < 5% (Cote, 1995) Except: Hct < 30: risk remains HIGH independent of PCA Role for caffeine (10 mg/kg IV) in prevention of postop apnea in prematures? (Wellborn, 1988) Pediatric Respiratory Physiology – Pulmonary and Thoracic Receptors Upper airway Pharyngeal receptors -> inhibition of breathing closure of larynx contraction of pharyngeal swallowing muscles Pediatric Respiratory Physiology – Pulmonary and Thoracic Receptors Upper airway - Larynx three receptor types pressure drive (irritant) flow (or cold) response to stimulus apnea coughing closure of glottis laryngospasm changes in ventilatory pattern newborn increased sensitivity to superior laryngeal nerve stimulus -> ventilatory depression or apnea H2O more potent stimulus than normal saline ([Cl-]) Pediatric Respiratory Physiology – Pulmonary and Thoracic Receptors Infant (especially preterm) reflex response to fluid at entrance to larynx Normal protective swallowing central apnea (H2O > NS) sneezing laryngeal closure coughing or awakening (less frequent) During inhalation induction pharyngeal swallowing reflex abolished laryngeal reflex intact -> breath holding or central apnea positive pressure ventilation may -> push secretions into larynx -> laryngospasm Pediatric Respiratory Physiology – Pulmonary and Thoracic Receptors Laryngospasm Sustained tight closure of vocal cords by contraction of adductor (cricothyroid) muscles persisting after removal of initial stimulus More likely (decreased threshold) with light anesthesia hyperventilation with hypocapnia Less likely (increased threshold) with hypoventilation with hypercapnia positive intrathoracic pressure deep anesthesia maybe positive upper airway pressure Hypoxia (paO2 < 50) increases threshold (fail-safe mechanism?) So: suction before extubation while patient relatively deep and inflate lungs and maybe a bit of PEEP at time of extubation Pediatric Respiratory Physiology – Pulmonary and Thoracic Receptors Slowly adapting (pulmonary stretch) receptors (SARs) Posterior wall of trachea and major bronchi Stimulus distension of airway during inspiration hypocapnia Response inhibit inspiratory activity (Hering-Breuer inflation reflex) May be related to adult apnea with ETT cuff inflated during emergence from anesthesia and rhythmic breathing promptly on cuff deflation Pediatric Respiratory Physiology – Pulmonary and Thoracic Receptors Rapidly adapting (irritant) receptors (RARs) Especially carina and large bronchi Stimulus lung distortion smoke inhaled anesthetics histamine Response coughing bronchospasm tracheal mucus secretion Likely mediate the paradoxical reflex of Head: with vagal afferents partially blocked by cold, inflation of lungs -> sustained contraction of diaphragm with prolonged inflation may be related to sigh mechanism (triggered by collapse of parts of lung during quiet breathing and increasing surface force) neonatal response to mechanical lung inflation with deep gasping breath Pediatric Respiratory Physiology – Pulmonary and Thoracic Receptors C-fiber endings (J-receptors) Juxta-pulmonary receptors Stimulus pulmonary congestion edema micro-emboli inhaled anesthetic agents Response apnea followed by rapid, shallow breathing bronchospasm hypersecretion hypotension bradycardia maybe laryngospasm Pediatric Respiratory Physiology – Chemical Control of Breathing Central Chemoreceptors Near surface of ventrolateral medulla Stimulus [H+] (pH of CSF and interstitial fluid; readily altered by changes in paCO2) Response increased ventilation, hyperventilation Pediatric Respiratory Physiology – Chemical Control of Breathing Peripheral Chemoreceptors Carotid bodies 3 types of neural components type I (glomus) cells type II (sheath) cells sensory nerve fiber endings carotid nerve -> C.N. IX, glossopharyngeal nerve Stimulus paCO2 and pH paO2 (especially < 60 mmHg) Response – increased ventilation Contribute 15% of resting ventilatory drive Neonate: hypoxia depresses ventilation by direct suppression of medullary centers Pediatric Respiratory Physiology – Chemical Control of Breathing Pediatric Respiratory Physiology – Chemical Control of Breathing Chronic hypoxemia (for years) Carotid bodies lose hypoxemic response E.g., cyanotic congenital heart disease (but hypoxic response does return after correction and restoration of normoxia) Pediatric Respiratory Physiology – Chemical Control of Breathing Chronic respiratory insufficiency with hypercarbia Hypoxemic stimulus of carotid chemoreceptors becomes primary stimulus of respiratory centers Administration of oxygen may -> hypoventilation with markedly elevated paCO2 Pediatric Respiratory Physiology – Assessment of Respiratory Control CO2 response curve Pediatric Respiratory Physiology – Assessment of Respiratory Control Effects of anesthesia on respiratory control Shift CO2 response curve to right Depress genioglossus, geniohyoid, other phayrngeal dilator muscles -> upper airway obstruction (infants > adults) work of breathing decreased with jaw lift CPAP 5 cmH2O oropharyngeal airway LMA Active expiration (halothane) Pediatric Respiratory Physiology – Lung Volumes and Mechanics of Breathing = 60 ml/kg infant after 18 months increases to adult 90 ml/kg by age 5 = 50% of TLC may be only 15% of TLC in young infants under GA plus muscle relaxants = 25% TLC Pediatric Respiratory Physiology – Lung Volumes and Mechanics of Breathing Elastic properties, compliance and FRC Neonate chest wall compliance, CW = 3-6 x CL, lung compliance tending to decrease FRC, functional residual capacity By 9-12 months CW = CL Dynamic FRC in awake, spontaneously ventilating infants is maintained near values seen in older children and adults because of 1. continued diaphragmatic activity in early expiratory phase 2. intrinsic PEEP (relative tachypnea with start of inspiration before end of preceding expiration) 3. *sustained tonic activity of inspiratory muscles (probably most important) By 1 year of age, relaxed end-expiratory volume predominates Pediatric Respiratory Physiology – Lung Volumes and Mechanics of Breathing Under general anesthesia, FRC declines by 10-25% in healthy adults with or without muscle relaxants and 35-45% in 6 to 18 year-olds In young infants under general anesthesia especially with muscle relaxants FRC may = only 0.1 - 0.15 TLC FRC may be < closing capacity leading to small airway closure atalectasis V/Q mismatch declining SpO2 Pediatric Respiratory Physiology – Lung Volumes and Mechanics of Breathing General anesthesia, FRC and PEEP Mean PEEP to resore FRC to normal infants < 6 months 6 cm H2O children 6-12 cm H2O PEEP important in children < 3 years essential in infants < 9 months under GA + muscle relaxants (increases total compliance by 75%) (Motoyama) Pediatric Respiratory Physiology – Dynamic Properties Poiseuille’s law for laminar flow: where R = 8lη/πr4 For turbulent flow: R resistance l length η viscosity R α 1/r5 Upper airway resistance adults: nasal passages: 65% of total resistance Infants: nasal resistance 30-50% of total upper airway: ⅔ of total resistance NG tube increases total resistance up to 50% Pediatric Respiratory Physiology Anesthetic effects on respiratory mechanics Relaxation of respiratory muscles -> decreased FRC cephalad displacement of diaphragm contributes to decreased FRC much less if patient not paralyzed airway closure atalectasis minimized by PEEP 5 cm H2O in children process slowed by 30-40% O2 in N2 (vs 100% O2) V/Q mismatch Endotracheal tube adds the most significant resistance Pediatric Respiratory Physiology Anesthetic effects on respiratory mechanics Endotracheal tube adds the most significant resistance Pediatric Respiratory Physiology Ventilation and pulmonary circulation Infants: VA per unit of lung volume > adult because of relatively higher metabolic rate, VO2 relatively smaller lung volume Infants and toddlers to age 2 years: VT preferentially distributed to uppermost part of lung Pediatric Respiratory Physiology Oxygen transport (Bohr effect) = 27, normal adult (19, fetus/newborn) Pediatric Respiratory Physiology Oxygen transport Bohr effect increasing pH (alkalosis) decreases P50 beware hyperventilation decreases tissue oxygen delivery Hgb F reacts poorly with 2,3-DPG P50 = 19 By age 3 months 9 months P50 = 27 (adult level) P50 peaks at 29-30 Pediatric Respiratory Physiology Oxygen transport If SpO2 = 91 then = PaO2 = Adult 6 months 6 weeks 6 hours 60 66 55 41 Pediatric Respiratory Physiology P50 Oxygen transport Hgb for equivalent tissue oxygen delivery Adult 27 8 10 12 > 3 months 30 6.5 8.2 9.8 < 2 months 24 11.7 14.7 17.6 Implications for blood transfusion older infants may tolerate somewhat lower Hgb levels at which neonates ought certainly be transfused Pediatric Respiratory Physiology Surfactant Essential phospholipid protein complex Regulates surface tension Stabilizing alveolar pressure LaPlace equation P = nT/r where P ressure r adius of small sphere T ension n = 2 for alveolus Surface tension: 65% of elastic recoil pressure Pediatric Respiratory Physiology Surfactant Produced by cuboidal type II alveolar pneumocytes (27th week) Lecithin (phosphatidylcholine, PC)/sphingomyelin (L/S) ratio in amniotic fluid correlates with lung maturity Pediatric Respiratory Physiology Surfactant Synthesis increased by glucocorticoids thyroxine heroin cyclic adenosine monophosphate (cAMP) epidermal growth factor tumor necrosis factor alpha transforming growth factor beta Synthetic surfactant used in treatment of premature infants with surfactant deficiency PPHN CDH meconium aspiration syndrome ARDS (adults and children) Pediatric Respiratory Physiology – Selected Points Basic postnatal adaptation lasts until 44 weeks postconception, especially in terms of respiratory control Postanesthetic apnea is likely in prematures, especially anemic Formation of alveoli essentially complete by 18 months Lung elastic and collagen fiber development continues through age 10 years Young infant chest wall is very compliant and incapable of sustaining FRC against lung elastic recoil when under general anesthesia, especially with muscle relaxants leading to airway closure and ‘progressive atalectasis of anesthesia’ Mild – moderate PEEP (5 cmH2O) alleviates Hemoglobin oxygen affinity changes dramatically first months of life Hgb F – low P50 (19) P50 increases, peaks in later infancy (30) implications for blood transfusion More Pediatric Airway Info at MetroHealthAnesthesia.com