* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cardiac Medications #2
Electrocardiography wikipedia , lookup
Jatene procedure wikipedia , lookup
Cardiac surgery wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
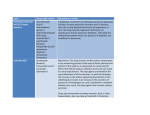
CARDIAC MEDICATIONS Why they do what they do (2014) LEARNING OBJECTIVES Students will be able to: Review the pathological process of Hypertension, Coronary Artery Disease and Heart Failure Discuss the major categories of drugs used for the treatment of Cardiac Disease. Describe the effects of these medications on cardiac function. Describe nursing considerations when administering above medications. WHAT CAN GO WRONG ? Circulation could be impaired by a weakened pumping action (CCF) Irregular heart beat (Arrhythmias ) Narrowed or clogged blood vessels due to fatty deposits - atherosclerosis ( CAD, Hypertension , Stroke ,MI ) Loss of elasticity of vessel walls and increase in pressure of circulating blood on vessel walls (Hypertension) CARDIAC DRUGS AND HYPERTENSION (2013) REGULATION OF BLOOD PRESSURE Blood pressure is the force exerted by the blood against walls of the blood vessells Arterial BP = CO x SVR Regulation involves nervous system, cardiovascular system, renal and endocrine systems Vascular endothelium - endothelin SDL Lewis pg. 832 SDL - HYPERTENSION Major groups of first–line antihypertensives can Can be arranged in order of the first four letters of the alphabet. A - ACE inhibitors , angiotensin 11 receptor antagonists B - β- blockers ***** C - Calcium channel blockers (antagonists) D - diuretics Discuss the above under the headings ,example, mechanism of action, risk factors, precautions, and side effects . Lewis pg : 841 DIURETICS Prescribed to treat Hypertension or to eliminate oedema caused by Heart Failure Most diuretics increase urine output by blocking reabsorption of sodium and chloride They are classified into four categories - Loop - Thiazides - Potassium Sparing - Osmotic THE NEPHRON DIURETICS: TO REDUCE OVERALL VOLUME OF BLOOD Thiazides (chlorothiazide) Inhibit Na reabsorption in the distal convoluted tubule Slow acting Use with caution with Digoxin LOOP DIURETICS (Frusemide) Inhibit sodium and chloride reabsorption at proximal and distal tubules and ascending loop of Henle Promote excretion of water, sodium, chloride and potassium Indicated for acute pulmonary oedema Frumil – loop and K+ sparing POTASSIUM-SPARING DIURETICS ( Amiloride) Act in the distal and collecting renal tubules either directly or by inhibiting aldosterone to inhibit sodium reabsorption and potassium excretion . Need to watch for hyperkalemia and don’t give potassium supplements Monitor electrolytes and fluid intake/output Monitor blood pressure and daily weights Less potent than thiazide and loop diuretics but useful as an adjunct to other diuretic therapy Contraindicated in renal failure. ALDOSTERONE RECEPTOR BLOCKERS (Spironolactone) Also classed as potassium sparing Inhibits Na retaining and K+ excretion effects of aldosterone in distal and collecting tubules. Watch for hyperkalaemia Monitor use with ACE inhibitors Do not combine with other PSD’s OSMOTIC DIURETICS - MANNITOL Elevate osmotic pressure of the glomerular filtrate to hinder reabsorption of solutes and water and promote excretion of water, sodium, potassium, chloride, calcium, phosphorus, magnesium and uric acid Mannitol(Osmitrol) Used mainly for reducing intracranial and intraocular pressure. DIURETICS NURSING INTERVENTIONS Monitor for dehydration - confusion Monitor for electrolyte imbalances especially hypokalaemia which can trigger arrhythmias Monitor for hypotension – teach signs of orthostatic hypotension Monitor weight daily – report weight gain and oedema Listen to chest sounds –> crackles -> overload Take diuretic in morning preferably as need to urinate increases for 6 to 8 hrs. VASODILATORS Dilate peripheral blood vessels by directly relaxing arteriolar smooth muscle Usually used in combination with other antihypertensives as they increase sodium and fluid retention Several classes include Calcium antagonists, nitrates, ACE inhibitors and sympatholytics CALCIUM ANTAGONISTS CALCIUM CHANNEL BLOCKERS Felodipine, Nifedipine, Diltiazem, Verapamil Inhibit the influx of calcium ions into muscle cells; act on vascular smooth muscle (primary arteries) to reduce spasms and promote vasodilatation Decrease contractility, workload and Oxygen demands May enhance serum Digoxin levels Watch for rapid drop in BP if given IV Avoid grapefruit if on Nifedipine CARDIAC MEDICATIONS Coronary Artery Disease CASE STUDY Jane Hart 55, has a history of hypertension and hyperlipidaemia. She is admitted to the emergency unit with chest discomfort. A 12 lead ECG shows atrial fibrillation, and ST elevation in in the inferior leads. She has bilateral crackles in her lung bases with an S3 heart sound. Cardiac enzymes are raised and a diagnosis of ACS with AF and heart failure is made. THE OVERALL GOAL IN MANAGING CORONARY ARTERY DISEASE To reduce 5-year cardiovascular risk to less than 15% with medications (NZGG, 2003). Ensure individuals with total cholesterol greater than 8mmol/L undergo risk assessment and lipid modifying treatment. Ensure BP less than 170/100 drug treatment DIFFERENT DRUG EFFECTS: Inotropic: relating to or influencing the force of contraction Chronotropic: influencing the rate; especially the heart beat Dromotropic: affecting the rate of electrical impulses in the heart muscle. Affects conduction velocity of the AV node Jarvis, 2000, Figure 17-8. p. 505. WHAT IS THE GOAL OF MEDICAL MANAGEMENT OF CAD Dissolve clots (save muscle) Maximize blood flow to heart muscle Maximize preload Minimize the afterload Maximize cardiac contractility (inotropic effect) Reduce chances of clot formation Reduce overall blood volume if overloaded Heart rate between 60-80 beats/min to maximize cardiac output and filling pressures Treat arrhythmias WHAT DRUGS HELP MEET THESE GOALS? Dissolve existing clots quickly—tPA, Metalyse (TNK) - Streptokinase ->Thrombolytics Maximize preload— I.V. fluids, volume expanders Minimize afterload — Ace inhibitors, Maximize cardiac contractility— Digoxin, Dopamine Maximize blood flow to heart— vasodilators Nitrates CONTINUED …………. Inhibit factors necessary for platelet aggregation - antiplatelets (aspirin) reduce overall fluid volume in overload – diuretics Keep heart rate between 60 -80 b/min – (Beta blockers and Calcium-channel blockers ) Antiarrhythmics – amiodarone, lignocaine, atropine CLOTTING MECHANISM Platelets accumulate release chemicals that activate blood clotting factors factors together with vit K act on fibrinogen convert to fibrin fibrin enmeshed with platelets form clots http://www.youtube.com/watch?v=xNZEERMSeyM THROMBOLYTIC DRUGS (CLOT BUSTERS) tPA - tissue plasminogen activators Increase blood level of plasmin Breaks down fibrin threads Metalyse – New Streptokinase not drug of choice Alteplase - (rt-PA) can be given if pt had Streptokinase http://www.bioportfolio.com/leaddiscovery/thrombolysis.gif ANTIPLATELET AGENTS Low dose Aspirin Clopidogrel (Plavix ) Aspirin blocks the formation of thromboxane A2 inhibiting platelet aggregation (sticking together) A single daily dose of around 80mg can effectively sustain the desired antiplatelet effect Risk of bleeding ANTICOAGULANTS Heparin IV, Clexane, warfarin Binds to anti-thrombin, inactivating coagulation factors and thrombin, thereby blocking the conversion of fibrinogen to fibrin Prevent formation of a clot or stabilize existing clots so that they do not break away and cause embolism Do not dissolve clots SIDE EFFECTS: ANTICOAGULANTS, THROMBOLYTICS AND ANTIPLATELETS Bleeding Stroke Reperfusion arrhythmias Hypotension Allergic reactions SDL- THROMBOLYTICS, ANTIPLATELETS AND ANTICOAGULANTS Discuss the above drugs under the following headings : Examples Mechanism of action Risk factors Precautions and nursing considerations Side effects ACE INHIBITORS (pril) Accupril, Captopril Used to treat both hypertension and ACS Inhibit the conversion of angiotensin I to angiotensin II, thus blocking the release of aldosterone, thereby reducing sodium and water retention Decrease pulmonary congestion and peripheral oedema Potassium-sparing so watch for hyperkalemia Discontinue if pt complains of dry irritating cough ( caused by inhibiting breakdown of bradykinins and kinins ANGIOTENSIN 11 RECEPTOR ANTAGONISTS (ARB’S) Selectively bind to Angiotensin 11 receptors in vascular smooth blood vessels to prevent vasoconstriction. Prevents the release of aldosterone in the adrenal cortex caused by the reaction of these receptors with angiotensin 11 End in “sartan” eg. Losartan, candesartan, eprosartan Results in decrease in blood pressure due to decrease in peripheral resistance and blood volume Used for patients intolerant to ACE inhibitors INOTROPES Inhibits the sodium-potassium pump, causing an increase in intracellular sodium levels Increased sodium levels force sodium out of the cell in exchange for calcium Higher intracellular calcium levels increase the force of contraction, increasing cardiac output Digoxin (cardiac Glycoside ) also blocks the slow calcium channels of the AV nodes, slowing the HR CARDIAC GLYCOSIDES Digitalis (Digoxin) – Lanoxin Act by influencing movement of ions in and out of the myocardial fibres (calcium and sodium) Improve pumping action of the heart reduce the flow of electrical impulses through the AV node slowing ventricular contraction increase contractility improve efficiency of each heart beat NITRATES GTN – Nitroglycerin – relaxes smooth muscle Cause vasodilatation reducing the amount of blood returning to the heart from the venous system (Venous filling ) thus decreasing preload. This decreases the work of the heart and the demand of the myocardium for oxygen. Demands must not exceed supply. Dilate the peripheral arteries, decreasing the resistance against which the left ventricle must pump (decreases afterload). Dilates coronary arteries and collateral vessels SDL – GTN education plan NITRATES The following are categories of medicines that can increase or decrease the effects of nitrates. Because there are so many kinds of medicines within each category, not every type of medicine is listed by name. Tell your doctor about every medicine that you are taking, even if it is not listed below. Viagra (sildenafil), Levitra (vardenafil), or Cialis (tadalafil). Do not take Viagra, Levitra, or Cialis within 24 hours of taking nitrates. When these erectile dysfunction medicines are mixed with nitrates, the combination can lower your blood pressure and make you dizzy, lightheaded, or faint. In some cases, patients have died after mixing erectile dysfunction medicines with nitrates. Medicines to treat high blood pressure Certain heart medicines Over-the-counter cough, cold, and flu medicines Over-the-counter herbal cough, cold, and flu medicines While taking nitrates, you should avoid smoking. Smoking can decrease the effect of the medicine. You should also avoid alcohol, because it can increase the effect of the medicine. BETA-BLOCKERS (LOLS) Block beta-adrenergic receptors of CNS Blockage of beta-1 receptors causes a decrease in contractility, decrease in heart rate, blood pressure and a slowing of impulse of conduction through the AV node (negative inotrope, chronotrope, dromotrope) These 3 mechanisms of action combine to decrease myocardial oxygen demand helping to prevent angina BETA BLOCKERS CHOLESTEROL (LIPID) LOWERING DRUGS HYPOLIPIDAEMIC DRUGS Statins - Simvastatin (Lipex ),Lipitor (common) Reduce levels of fats in the blood by interfering with absorption of bile salts in the bowel (carry large amounts of cholesterol) Prevent conversion of fatty acids to lipids in the liver Reduce plasma lipids and lipoproteins Block the production of LDLs and increase receptor activity that removes LDLs (SDL) CHOLESTEROL (LIPID) LOWERING DRUGS HYPOLIPIDAEMIC DRUGS ANTIARRYTHMIC DRUGS Act by impeding the movement of ions across the membrane of myocardial cells Affects action potential Treat ectopic beats stabilises the excitable myocardial tissue Suppresses automaticity, depresses rate of depolarisation, slows impulse conduction, prolongs action potential and increases refractory period. ( SDL) Amiodarone ADRENALINE Adjunctive in the treatment of cardiac arrest Sympathomimetic β and α effects Influence both BP and tissue perfusion stimulation of receptors in myocardium result in increased rate, and force of contraction Increased CO results in increased BP Cardiac Medications Congestive Heart Failure AIMS OF TREATMENT - CHF Treat underlying cause Relieve symptoms by reducing workload of the heart. Improve quality of life Prevent readmission to hospital, and/or recurrent ischaemic events Reduce mortality Drugs used to treat CHF ACE Inhibitors Beta Blockers Diuretics Vasodilators Inotropes (e.g. Dopamine) Digitalis POTASSIUM CHLORIDE Intracellular ion Transmission of nerve impulses Contraction of cardiac muscles Levels 4.0-4.5 Hypokalaemia=potassium deficit SDL