* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Pulmonary-vasc
Cardiovascular disease wikipedia , lookup
Electrocardiography wikipedia , lookup
Cardiac surgery wikipedia , lookup
Heart failure wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Myocardial infarction wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Atrial septal defect wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
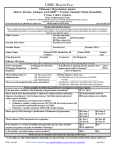
Pulmonary Hypertension and Right Heart Failure Pulmonary venous hypertension (Cardiac) • LVF-ischaemic • Mitral Regurgitation / Stenosis • Cardiomyopathy-eg alchohol ,viral Pulmonary arterial hypertension • Hypoxic – COPD , OSA , Fibr Alveolitis • Multiple Po Emboli • Po vasculitis –eg SLE , PAN ,Systemic Sclerosis • Drugs –eg appetite suppressants • Cardiac Left to right shunt – ASD , VSD • Primary pulmonary hypertension (only after excluding all of above) Clinical Signs of Pulmonary Hypertension and Right Heart Failure • Central cyanosis if hypoxic • Dependent oedema • Raised JVP with V waves (due to secondary tricuspid regurg) • Right ventricular heave at left parasternal edge • Murmur of tricuspid regurgitation • Load P2 • Enlarged liver (pulsatile ) Investigation of Pulmonary Hypertension • • • • • • • • ECG CXR SaO2 and arterial blood gases Pulmonary function Echocardiogram / Cardiac Catheterisation D dimers and VQ scan if PE suspected CT Pulmonary Angiogram Auto-antibodies if vasculitis suspected Primary pulmonary hypertension • Diagnosis by exclusion of other secondary causes • Progressive SOBOE and signs of right heart failure • Pharmacologic Treatment -prophylactic anticoagulation [warfarin] -O2 if hypoxic -Po Vasodilators :Endothelin antagonist (Oral Bosentan) , PDE5-inhibitor (Oral Sildenafil), iv Epoprostenol THROMBOEMBOLIC LUNG DISEASE • Pulmonary infarction -in situ -venous emboli • Virchow’s Triad -Stasis -Vessel wall damage -Hypercoagulablity RISK FACTORS FOR DVT AND PE #1 •Thrombophilia- FH,freq,site,age •Contraceptive pill ,HRT •Pregnancy •Pelvic obstruction-eg uterus,ovary,lymph nodes •Trauma-eg RTA RISK FACTORS FOR DVT AND PE #2 • Surgery- eg pelvic,hip,knee • Immobility-eg bed rest,long haul flights • Malignancy • Myocardial infarction • Po hypertension/vasculitis DVT • Proximal (Ileofemoral) -most likely to embolise -most likely to lead to chronic venous insufficiency and venous leg ulcers • Distal (Polpiteal) -least likely to embolise Clinical presentation of DVT • Whole leg or calf involved depending on site • Swollen,hot,red,tender • Differential:Popliteal synovial rupture[Bakers cyst],Superficial thrombophlebitis,Calf cellulitis Investigation of DVT • Ultrasound Doppler leg scan(1st line) -Non invasive -Exclude popliteal cyst, pelvic mass • CT scan of ileofemoral veins,IVC and pelvis • Constrast venography -Invasive,contrast(irritant,allergy) -Rarely indicated Pulmonary Emboli • Predisposing DVT may be silent • Clinical presentation depends on size: • Large-cardiovascular shock,low BP,central cyanosis,sudden death • Medium-pleuritic pain,haemoptysis,breathless • Small recurrent-progressive dyspnoea, pulmonary hypertension and right heart failure Diagnosis of PE #1 • Clinical SignsTachycardia,Tachypnoea,Cyanosis,Fever Low BP,Crackles, Rub, Pleural effusion • Arterial blood gases-PaO2,Sao2 (Type 1 resp failure:PaCO2 normal or low) • CXR-Normal early on before infarction -Basal atelectesis,Consolidation , Pleural effusion after infarction Diagnosis of PE #2 Investigations • ECG :Acute Rt heart strain pattern (S1,Q3,T3 , T inv in V1-3) • D-dimers usually raised • Isotope lung scan (Ventilation/Perfusion) • Perfusion defect before infarction • Perfusion+Ventilation matched defect after infarction V/Q isotope scan in Recurrent Po emboli Multiple filling defects (arrows) on perfusion (Q) scan Mismatched to ventilation (V) scan Dyspnoea ,Hypoxia,Cardiomegaly ,Po Hypertension and Large RV on Echo , Restrictive Lung Vols with Low DLCO ,Hypoxia Diagnosis of PE #3 • CT pulmonary angiogram to image pulmonary artery filling defect • Leg and pelvic ultrasound to detect silent DVT • Echocardiogram to measure pulmonary artery pressure and RV size • Gas transfer factor (TLCO) to measure perfusion defect CT Po Angiogram in Acute Massive PE Occluded Rt main Po Artery (arrow ) and filling defect Lt Po artery Acute Dyspnoea ,Hypoxia ,Low BP , Acute Rt Heart Strain on ECG Raised D dimers .No clot seen in IVC or ileofemoral veins Treated with Thrombolysis and Low MW Heparin Investigation of underlying cause of PE • If no obvious underlying cause –eg surgery /pregnancy /malignancy /immobility • Look for underlying Ca – Clin exam ,CXR,PSA,CA125,CEA,Pelvic USS • Autoantibodies (SLE) – Antinuclear ,AntiCardiolipin • Coagulation factor screen – Antithrombin3,Protein C/S, Factor 5/8 Prevention of DVT • • • • Early post-op mobilisation TED compression stockings Calf muscle exercises Subcutaneous low dose low mol wt heparin perioperatively • Dabigatran - direct thrombin inhibitor Rivaroxaban - direct inhibitor of activated factor X- both given orally for prophylaxis of venous thromboembolism in adults after hip or knee replacement surgery Treatment of DVT/PE #1 • Anticoagulation prevents clot propagation-tips balance to thrombolysisbody dissolves clot • Initiate with parenteral heparin-fast acting-via antithrombin-3 • Usually therapeutic dose of s/c low mol wt heparin ( Dalteparin “Fragmin”) Treatment of DVT/PE #2 • Low mol wt heparin –once daily injection ,no monitoring –no hassle • IV infusion unfractionated heparin -more hassle-need to monitor clotting, increased bleeding risk- rarely used nowadays Treatment of DVT/PE #3 • Start concurrent oral warfarin-takes 3 days-antagonises vit K1 dependent prothrombin • After 3-5 days stop heparin-when INR>2 • Need to monitor APTT with unfractionated -but not with low mol wt heparin Treatment of DVT/PE #4 • Continue Warfarin for 3-6 months • Monitor Warfarin with INR-Target range 2.53.5 • Interactions which increase anticoagulation -Alcohol,Antibiotics ,Aspirin,NSAIDs, Amiodarone, Cimetidine,Omeprazole ,etc etc • Look in BNF for possible interactions Treatment of DVT/PE #5 • Thrombolysis-Streptokinase or TPA • Only for large life threatening PE-ie low BP and severe hypoxaemia due to main pulmonary artery occlusion • IVC filter to prevent embolisation from large ileofemoral/IVC clot - for recurrent PE’s • Thrombo-embolectomy –rarely indicated • Aspirin –no role – anti-platelet Overanticoagulation • Address underlying cause-eg drug interaction,chronic liver disease,CHF • If bleeding then stop anticoagulant and reverse effect • Low MW Heparin has a long half life • Warfarin has a long half life • May need cover with prothrombin complex concentrate or fresh frozen plasma • Reverse warfarin with vitamin K1(especially if chronic liver disease) • Reverse heparin with protamine