* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Shock and Burns
Heart failure wikipedia , lookup
Jatene procedure wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Coronary artery disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiac surgery wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
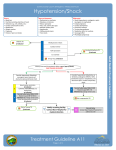
Shock and Burns By: Diana Blum MSN MCC NURS 2140 Shock • Life threatening • Inadequate tissue perfusion that can lead to cell death • Unpredictable • Definition: condition in which tissue perfusion is inadequate to deliver oxygen and nutrients to support vital organs and cellular function. Causes • Death is not a classified as shock but as multiple organ dysfunction. Circulatory Homeostasis Tissue perfusion is driven by blood pressure BP = CO X PVR CO – Cardiac Output PVR – Peripheral Vascular resistance Cardiac Output CO = SV X HR This means that BP= SV X HR X PVR Blood Pressure = Stroke Volume X Heart Rate X Peripheral Vascular Resistance Stroke Volume • Volume of Blood pumped by the heart during 1 cycle What affects Stroke volume? Blood Volume Mechanical Obstruction Rhythm Problems Heart Muscle Damage Stroke Volume Mechanical Obstruction What makes up blood volume Plasma RBCs Platelets WBCs Necessary blood flow components • Adequate cardiac pump • Effective circulatory system • Sufficient blood volume • If one component compromised cell starvation and death can occur. This in turn will cause organ death, and end of life of pt. Heart Rate • Heart rate increases as a compensatory response to Shock • Rarely you get High Output failure Heart rate too fast to allow adequate refilling of heart between beats What Alters PVR? • Circulation cytokines & Inflammatory mediators (e.g. Histamine) • Endotoxins • Drugs (e.g. Nitrates) Nurses must: • • • • Be critical thinkers Be able to act fast Be able to anticipate orders Execute orders in a timely yet quickly manner Normal cell function • Metabolism of energy within cell – Nutrients broken down and stored as ATP • ATP is used for muscle contraction, active transport, conduction of electrical impulses Patho of Shock • Cells lack blood supply • Normal function ceases • Cell swells and membrane becomes permeable – Electrolytes leak out of cell • Mitochondria become damaged • Death of cell occurs Stages • Compensatory • Progressive • Irreversible Compensatory • BP WNL • Body shunts blood from organs in fight or flight response to the brain and heart • s/s: cool, clammy, hypoactive bowel sounds, HR greater than 100, RR greater than 20, decreased urine output, confusion, respiratory alkalosis, Na+ is elevated, BGM is elevated • If treated here, prognosis good • Tx: find cause and fix, IVF, monitor vs, monitor LOC, monitor I/O, promote safety Pathophysiological Response • “Flight or fight response” • Increased Catecholamine release • Activation of Renin-Angiotensin system • Increase glucocorticoid and mineralcorticoid release • Activation of Sympathetic nervous system • In stress situations: – catecholamines, cortisol, glucagons, etc are released • Causes hyperglycemia • Causes insulin resistance • Promotes gluconeogenesis from proteins and fats All this leads to organ failure in the end Progressive • s/s: Hypotension <90/40, interstitial edema, rapid/shallow respirations, crackles, desats, pulmonary edema, dysrhythmias, ischemia, tachycardic, chest pain, agitation, confusion, low U.O. , lethargic, jaundice, bloody diarrhea, metabolic acidosis, mottled, petechiae – Leads to ards – MI is possible – DIC may occur • Overworked heart causes ischemia and myocardial depression leading to heart failure • Prognosis worsens • DX: BNP, CMP, CBC, ABG • TX: mechanical vent, enteral support, Insulin, careful assessments, ICU, Neuro checks, balloon pump, meds, dialysis, infection prevention, family support Irreversible • Organ damage severe • Death imminent • s/s: low BP, necrosis to liver and kidneys, respiratory system fails even on vent, unresponsive • Dx: based on failure to respond to tx • Tx: palliative care, experimental tx, monitor pt, provide comfort, pastoral care Treatment of Shock • IVF and or blood products • Blood if related to this • LR or NS • Intial amount 2-3 liters for an adult with unknown cause • Monitor client closely • Beta and alpha adrenergic receptors – NIPRIDE, levaphed, vasopressin • Pain management • Sympathomimetics – Dopamine, dobutamine, adrenalin, milrinone, amrinone • Nutritional support – Parenteral or enteral • http://www.youtube.com/watch?v=9a7N9 AU1GiQ&feature=related 5 types • • • • • Hypovolemic Cardiogenic Septic Neurogenic Anaphylactic HYPOVOLEMIC Hypovolemic Shock Caused by Body Fluid Loss Site of Fluid Loss Mechanism of Loss Skin Thermal or chemical burn, sweating from excessive heat exposure GI tract Vomiting or diarrhea Kidneys Diabetes mellitus or insipidus, adrenal insufficiency, “salt-losing” nephritis, the polyuric phase after acute tubular damage, and use of potent diuretics Intravascular fluid lost to the extravascular space Increased capillary permeability secondary to inflammation or traumatic injury (eg, crush), anoxia, cardiac arrest, sepsis, bowel ischemia, acute pancreatitis Causes • External fluid loss – – – – – – Trauma Surgery Vomiting Diarrhea Diuresis Diabetes insipidus • Internal fluid shift – – – – – Burns Hemorrhage Ascites Peritonitis Dehydration Treatment • Treat underlying cause • Replace fluid and/or blood • Place in modified tredelenburg (legs elevated) • Meds depending on cause • Blood • Oxygen CARDIOGENIC • Impaired oxygen • 2 types: coronary and non coronary – Coronary: LV damage, MI=greatest risk – Non-coronary: Stress on myocardium (heart disease, acidosis, etc.) – Manifestations: angina, dysrythmia – Dx: cardiac enzymes, ekgs, – Tx: correct underlying cause, O2, pain control, IVF, balloon pump, ICU, CABG, nitro, dobutamine, dopamine, levophed, antiarrythmics, vent Mechanisms of Cardiogenic and Obstructive Shock Type Mechanism Obstructive Mechanical interference Tension pneumothorax, with ventricular filling cava compression, cardiac tamponade, atrial tumor or clot Cardiogenic Cause Interference with ventricular emptying Pulmonary embolism Impaired myocardial contractility Myocardial ischemia or MI, myocarditis, drugs Abnormalities of cardiac Tachycardia, rhythm bradycardia Cardiac structural disorder Acute mitral or aortic regurgitation, ruptured interventricular septum, prosthetic valve malfunction Circulatory shockaka Distributive • Occurs with abnormally placed blood volume • 3 types – Septic – Neurogenic – anaphylactic SEPTIC Management • • • • • • • • • Antibiotics rhAPC Aggressive nutritional support Aseptic technique for procedures Monitor IV lines, indwelling lines, and wounds Monitor LOC Monitor vs—keep temp in check IVF Vasoactive agents like other shocks NEUROGENIC • Vasodilatation occurs – Results of balance loss b/w sympathetic and parasympathetic stimulation • Sympathetic: vascular smooth muscles constrict • Parasympathetic: causes smooth muscle to relax or dilate • In neurogenic shock, the lean is to parasympathetic ANAPHYLACTIC • • • • Occurs rapidly Life threatening Caused by severe allergic reaction Tx: remove agent, antihistamine, epinephrine, nebulizers, CPR, intubate, IVF, assess allergies, educate about meds and treatment if exposure Treatment of Shock ABC Multisystem organ dysfunction • Complication of SIRS/Sepsis/tissue injury • Unknown trigger • Begins in lungs usually, then liver, GI, and kidneys • s/s: respiratory failure, hyperglycemia, hyperlacticacidemia, polyuria, infection, jaundice, • Tx: intubation, ICU, dialysis BURNS Causes • • • • • Thermal: electricity chemicals scalds Radiation inhaled http://www.youtube.com/watch?v=Gj4GgioI5CM&feature=related Superficial partial thickness • Epidermis destroyed • Parts of dermis injured • s/s: pain, appears red/dry – Example: sunburn Deep partial thickness • Destruction of epidermis and upper dermis • Injury to deeper portions of dermis • s/s: painful wound that appears red and exudes fluid…cap refill follows tissue blanching • Hair follicles are intact • May result in scars Full thickness • • • • • • Destroyed epidermis Destroyed dermis Appears white, red, brown, or black No pain Wound appears leathery Hair follicles and sweat glands destroyed Classifying Burns • • • • • How did injury occur Causative agentscald or chemical Temp of burn agent Duration of contact Thickness of skin Rules of nine Lund Browdner Formula Parkland Formula • Parkland Burn Formula: 4 cc. per kg. body weight per % deep burn during the first 24 hours 1. To calculate: multiply 4 X kg. X % burn ˜ total fluid requirement 2. Give half of this amount during the first 8 hours from the time of injury 3. In most cases, this will work out to 2 large bore IV’s wide open until hospital arrival a. Monitor and record the exact amounts given, and provide hospital personnel with this information 4. Lactated Ringer’s is the preferred fluid, if available • Electrical Burns • Worst to get • Will cause lifelong neurovascular problems • High voltage (>1000 volts) cause bone and tissue destruction – Leads to amputations and death • There is usually an entrance and exit wound – Travels from least resistance to ground • Clothes catch fire Compli cations • • • • • • • • • • HypoVolemia Decreased cardiac output Hypotension Edema Obstruction of blood flow Hyponatremia Hyperkalemia Inhalation injury Sepsis Ileus • REMEMBER CAB • http://www.youtube.com/watch?v=BB8k Tdbzzpo&feature=related TX • • • • • • • • • Current immediately contracts muscles Dysrhythmias and spinal injuries occur EKG Monitoring Spinal collar IVF LR Monitor urine output Prone to RF Frequent Neuro Checks ET tube ICU or Burn Center Stages Of Burn Care • Emergent • Acute • Rehab Emergent Care • From onset of injury to end of fluid resuscitation – Remove from harm/extinguish flames on victim – Establish airway – Cool wound with cool water – O2 – Large bore IV – Immobilize cervical spine At hospital • • • • • • • • • Airway O2 Chest x-rays CMP,CBC, Blood alcohol, ABG Clean sheets under and over pt Tetanus Photos taken Catheter placement Xfer to burn center Acute • From the beginning of diuresis to wound closure – Remove restrictive objects – Irrigate chemical burns/Cover wound – Nutritional support – Prevent complications • Priority is airway, pain control, wound care, and maintaining balance • Bronchial lavage may need to be done • May be placed on vasoactive meds, diuretics, and fluid restriction • ICU with Art line Infection prevention • • • • • • • Asepsis Antibx as ordered Wound cleaning Baths are painful Topical antibacterials Loose dressings Debridment Grafts • Autograft • Homograft • Biograft and synthetic dressings Care of graft site • Occlusive dressing initially • First dressing change 2-5 days after surgery • Monitor drainage • Position carefully • Exercise 5-7 days after surgery Care of donor site • • • • Pain management Moist gauze at surgery Vaseline gauze Heals in 7-14 days Nutritional support • • • • • • Control stress and pain Protein requirements: 1.5-4.0g per kg Include lipids Carbs good 5000 calories/day Or – Enteral feeding Scars • Hypertrophic cause contractures on joints • Ace wraps are helpful to promote circulation • rehab keloids • Mass of scar tissue • Mostly in dark skin individuals • Monitor healing process • Monitor contractures Rehab • • • • Prevent scars and contractures PT,OT, Speech Reconstructive Surgery Counseling Research • Nutrition • Artificial skins SHOCK Clinical Scenarios • 1) A 26 year old man with a comminuted closed fracture of the femur shaft undergoes intramedullary nail fixation. Two days post operatively, he develops a pyrexia, shortness of breath and tachycardia. • Discuss the emergency management? • 2) A 72 year old man develops sudden back pain and is brought to the emergency department with a swollen ,tense abdomen. He is tachycardic ,with a low volume pulse and low BP. • Discuss the emergency management? • 3) A 72 year old man with an underlying prostate carcinoma sustains a femoral shaft fracture .He undergoes intramedullary nail fixation. At post operative day 7 he develops a shortness of breath ,hypotension and a tachycardia • Discuss the emergency management? Questions